Pulmonary Function Tests: How to Interpret Spirometry and DLCO Results
 Nov, 23 2025
Nov, 23 2025
When your doctor says you need a pulmonary function test, it’s not just another checkbox. It’s a clear window into how well your lungs are actually working - especially when you’re short of breath, coughing nonstop, or just feel like you can’t catch your air. Two of the most important tests in this group are spirometry and DLCO. Together, they tell a complete story: one measures how fast and how much air you can move in and out, the other measures how well oxygen actually gets from your lungs into your blood. Knowing how to read them helps you understand what’s really going on inside your chest - not just what symptoms you’re feeling.
What Spirometry Really Tells You
Spirometry is the most common lung test you’ll ever have. You blow into a tube as hard and fast as you can after taking the deepest breath possible. That’s it. No needles, no radiation, no discomfort. But what’s happening behind the numbers matters. The two key numbers you need to know are FEV1 and FVC. FEV1 is how much air you can blow out in the first second. FVC is the total amount you can blow out in one full breath. The ratio between them - FEV1/FVC - is the real star. If it’s below 0.7, you have airflow obstruction. That’s the hallmark of asthma or COPD. But if the ratio is normal and your FVC is low, that’s a different story. It suggests restriction - your lungs aren’t expanding fully. Here’s the catch: not all low FVC is the same. In obesity or scoliosis, your lungs are physically squeezed. In pulmonary fibrosis, your lung tissue itself is stiff and scarred. Spirometry alone can’t tell the difference. That’s where DLCO steps in.DLCO: The Test Most Doctors Don’t Fully Understand
DLCO stands for diffusing capacity of the lung for carbon monoxide. Sounds complicated? It’s not. It’s a simple test: you inhale a tiny, harmless mix of gases (including a trace of carbon monoxide), hold your breath for 10 seconds, then blow out. The machine measures how much carbon monoxide disappeared from the air you inhaled. That tells you how well oxygen can move from your lungs into your bloodstream. Normal DLCO is between 75% and 140% of what’s predicted for your age, height, and sex. Below 75%? Your lungs aren’t transferring oxygen efficiently. Above 140%? Something’s making your blood hold onto more gas than usual - like too many red blood cells or a heart shunt. Why is this test so often missed? Because it doesn’t show up in routine checkups. But here’s the truth: if you have unexplained shortness of breath and your spirometry is normal, DLCO is the next step. It’s the only test that can catch early lung scarring, pulmonary hypertension, or chronic blood clots in the lungs - conditions that won’t show up on spirometry until they’re advanced.Putting It Together: Real Patterns, Real Diagnoses
You don’t interpret these tests in isolation. You put them side by side. Here’s what the numbers actually mean in real cases:- Low FEV1/FVC + Normal DLCO: Classic asthma or COPD. The airways are narrowed, but the gas exchange surface is still intact.
- Low FVC + Low DLCO: This screams interstitial lung disease - like pulmonary fibrosis. The lung tissue is damaged, so both volume and oxygen transfer are down. DLCO often drops more than FVC, sometimes as low as 22% while FVC is still at 60%.
- Low FVC + Normal DLCO: This is "pseudorestriction." Your lungs aren’t damaged - they’re just squeezed. Think obesity, severe scoliosis, or a large belly from fluid buildup. The gas exchange is fine; the problem is mechanical.
- Normal spirometry + Low DLCO: This is the red flag most doctors miss. It could mean early pulmonary fibrosis, pulmonary embolism (blood clots in the lungs), or even early connective tissue disease. In fact, DLCO can drop 12-18 months before spirometry changes show up.
- High DLCO + Normal spirometry: This is unusual. It happens in asthma during flare-ups, polycythemia (too many red blood cells), or a heart defect that lets blood bypass the lungs.

Why Hemoglobin Matters More Than You Think
DLCO isn’t just about your lungs. It’s also about your blood. Hemoglobin carries oxygen. If you’re anemic, your DLCO will look artificially low - even if your lungs are perfect. For every 1 g/dL drop in hemoglobin, DLCO drops about 1%. That’s why every DLCO test should come with a recent blood count. If your hemoglobin was 10.5 instead of 14, your DLCO might be 20% lower than it should be. That’s not lung disease - that’s iron deficiency. Smoking also messes with DLCO. Carbon monoxide from cigarettes binds to hemoglobin, leaving less room for the test gas. That can falsely lower your DLCO by 5-10%. Always tell your technician if you smoked in the last 24 hours.When DLCO Changes Everything
There are cases where skipping DLCO leads to misdiagnosis. A patient with fatigue and mild shortness of breath has normal spirometry. They’re told it’s "just anxiety." But their DLCO is 58% of predicted. That’s not anxiety. That’s early pulmonary fibrosis - possibly from an autoimmune disease they didn’t even know they had. Catching it early means starting treatment before the lungs are permanently damaged. Another patient has a history of blood clots. Their breathing gets worse. Spirometry is normal. DLCO is 45%. That’s not just old clots - that’s chronic thromboembolic pulmonary hypertension. Without DLCO, this would’ve been missed for years. And then there’s the reverse: a patient with COPD and low DLCO. That tells you they’re not just smoking-related COPD - they likely have emphysema. That changes prognosis, treatment, and even eligibility for lung volume reduction surgery.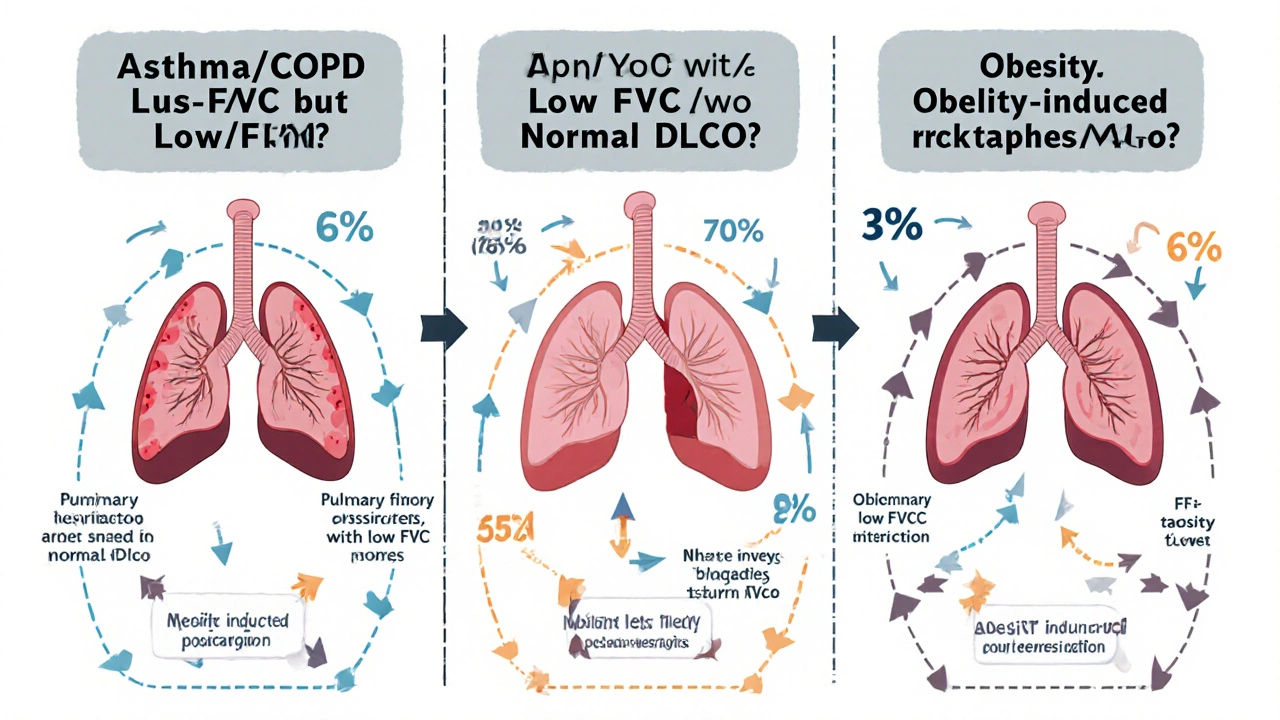
What Happens If You Don’t Get Tested?
Skipping these tests doesn’t make your symptoms go away. It just delays the truth. Many people live for years thinking they’re "just out of shape" when they actually have a progressive lung disease. By the time they’re diagnosed, their DLCO might be below 35% - a threshold tied to a nearly threefold increase in death risk for interstitial lung disease. Doctors don’t order DLCO because it’s expensive, complex, or they don’t understand it. But guidelines from the American Thoracic Society say it should be done for anyone with unexplained shortness of breath, before major surgery, and for anyone being monitored for lung scarring. It’s not optional. It’s essential.What to Do Next
If you’ve had spirometry and your doctor hasn’t mentioned DLCO - ask for it. Say: "My symptoms don’t match my spirometry results. Could I have a DLCO test?" If you have fibrosis, COPD, or a connective tissue disease like lupus or scleroderma, DLCO should be checked at least once a year. Make sure your lab measures your hemoglobin at the same time. Ask for the predicted percentage - not just the raw number. And if your DLCO is low, don’t accept "we’ll watch it" without asking why. What’s the next step? A CT scan? A heart echo? A blood test for autoimmune markers? The goal isn’t just to label a disease. It’s to catch it early enough to stop it from getting worse. Spirometry tells you how much air moves. DLCO tells you if that air is actually helping you live.What’s the difference between spirometry and DLCO?
Spirometry measures how much air you can move in and out of your lungs and how fast. It checks for blocked airways (like in asthma or COPD). DLCO measures how well oxygen moves from your lungs into your bloodstream. It finds problems with the lung tissue or blood vessels that spirometry can’t see.
Can DLCO be normal if I have lung disease?
Yes. In early-stage diseases like pulmonary fibrosis or chronic blood clots, spirometry can be normal while DLCO is already low. That’s why DLCO is so valuable - it catches damage before you start struggling to breathe. But if DLCO is normal, it doesn’t rule out all lung disease. Asthma, for example, often has normal DLCO unless it’s very advanced.
Why does my doctor need my hemoglobin level for DLCO?
Hemoglobin carries oxygen in your blood. If you’re anemic (low hemoglobin), your DLCO will read lower than it should - even if your lungs are healthy. For every 1 g/dL drop in hemoglobin, DLCO drops about 1%. Without knowing your hemoglobin, a low DLCO could be misread as lung damage when it’s really just iron deficiency.
Is DLCO painful or risky?
No. It’s completely safe. You breathe in a tiny amount of carbon monoxide - far less than you’d get from smoking one cigarette. The gas is harmless at these levels. The only challenge is holding your breath for 10 seconds, which can be hard for some older adults or people with severe breathlessness.
Can I get DLCO done at any clinic?
Not always. Spirometry is standard in most doctor’s offices. DLCO requires special equipment and trained staff to perform and interpret correctly. It’s usually done in pulmonary function labs, hospitals, or specialty clinics. Ask your doctor if they offer it or can refer you to one.
What if my DLCO is low but I feel fine?
Even if you feel okay, a low DLCO is a warning sign. It means your lungs aren’t transferring oxygen as well as they should. That could be early scarring, a small clot, or an autoimmune condition. You may not have symptoms yet because your body is compensating. But left unchecked, it can progress. The next step is usually imaging - like a CT scan - to find out what’s causing it.
Julie Pulvino
November 25, 2025 AT 00:33Finally, someone explained DLCO in a way that actually makes sense. I’ve had normal spirometry for years but kept feeling like I was suffocating-turns out my DLCO was at 62%. My doctor brushed it off until I asked. Don’t let them do that to you.
ann smith
November 25, 2025 AT 18:37This is such a needed post. I’ve been telling my patients for years that if they’re short of breath and spirometry is normal, DLCO is the next step. So many get misdiagnosed with anxiety. Thank you for breaking it down like this. 🙌
Patrick Marsh
November 27, 2025 AT 18:35DLCO matters. Hemoglobin matters. Smoking matters. Don’t skip the basics.
Danny Nicholls
November 28, 2025 AT 15:05Bro this is 🔥 I had no idea my DLCO was low until I asked for it after my last flare-up. Turns out I had early fibrosis-no symptoms yet, but now I’m on a treatment plan. Also, I smoked the day before my test and didn’t tell them… oops. 😅
Robin Johnson
November 29, 2025 AT 20:22If you’re not getting a DLCO when you have unexplained dyspnea, you’re not getting full care. This isn’t optional-it’s standard. Push back. Your lungs can’t wait.
Latonya Elarms-Radford
November 30, 2025 AT 13:14Isn’t it tragic, really? We live in a world where the body’s most vital exchange-oxygen for carbon dioxide-is reduced to a number on a screen, interpreted by overworked physicians who’ve never held a lung in their hands. We’ve forgotten that breath is the first prayer we utter, and the last we exhale. DLCO isn’t just a test-it’s a whisper from the soul of the respiratory system, begging to be heard before the silence takes over.
Mark Williams
December 2, 2025 AT 04:15DLCO reflects alveolar-capillary membrane integrity and pulmonary capillary blood volume. When FEV1/FVC is preserved but DLCO is reduced, it suggests microvascular or parenchymal pathology. In early ILD, DLCO decline precedes restrictive spirometry by 12–18 months. This is evidence-based. Not anecdotal.
james lucas
December 3, 2025 AT 16:49Man I didn’t even know DLCO was a thing until I read this. I thought if my breathing test was fine, I was good to go. Turns out I had a low DLCO and was just anemic-iron pills fixed it. So glad I didn’t just ignore it. Thanks for the heads up!
Nikhil Chaurasia
December 4, 2025 AT 02:20In India, most clinics don’t even have DLCO machines. My cousin was diagnosed with pulmonary fibrosis after 3 years of misdiagnosis because no one could run the test. Please, if you’re reading this and have access-get it done. Don’t wait for collapse.
Melvina Zelee
December 5, 2025 AT 23:33Love how you tied hemoglobin into this. I had a DLCO of 68% and thought I was dying… turns out my ferritin was 8. Iron infusion and now I can climb stairs again. This post saved me from a spiral of doom. Thank you.
Daniel Jean-Baptiste
December 7, 2025 AT 02:29Just got my DLCO done last week after reading this. Was nervous but it was totally fine. Held my breath for 10 sec like a champ. Also didn’t know you had to tell them if you smoked. Rookie mistake last time. Lesson learned.
Ravi Kumar Gupta
December 8, 2025 AT 16:42My father in India had COPD and was told his lungs were fine because spirometry was 'borderline.' He died at 62. His DLCO was 28%. If only someone had known. This post is not just education-it’s a lifeline. Please share it with every doctor you know.
Rahul Kanakarajan
December 9, 2025 AT 07:32Why are people so surprised by this? It’s basic pulmonology. If you’re not checking DLCO for unexplained dyspnea, you’re practicing lazy medicine. And yes, your anemia affects it-so what? That’s why you get labs. This isn’t rocket science. Stop acting like it is.