Post-Menopausal Women and Medication Changes: Safety Considerations
 Nov, 17 2025
Nov, 17 2025
Medication Safety Checker for Post-Menopausal Women
Check Your Medications for Safety
Enter your current medications to identify potential safety risks specific to post-menopausal women. This tool highlights medications that may be inappropriate or dangerous based on the latest clinical guidelines.
When you’re past menopause, your body doesn’t just stop changing-it starts reacting differently to the medicines you take. What worked at 50 might not be safe at 65. And with most women in this stage taking four or five prescriptions daily, the risk of harmful side effects, dangerous interactions, or even hospitalization rises sharply. This isn’t just about hot flashes or sleep trouble. It’s about whether your blood pressure pill could make your hip fracture worse, or if your estrogen patch could raise your stroke risk. The rules have changed. And if you’re not aware of them, you’re playing with fire.
Why Your Body Handles Medicines Differently After Menopause
Your liver and kidneys don’t work the same after menopause. Hormone shifts slow down how your body breaks down drugs. That means a dose that was fine at 52 might build up to toxic levels by 65. A common blood thinner, warfarin, for example, can become too strong in older women, leading to dangerous bleeding. Same with statins-your muscles are more likely to hurt or break down when you’re past menopause, even on low doses.
Then there’s body composition. You lose muscle and gain fat. Fat holds onto certain drugs longer. That’s why some antidepressants and anti-anxiety pills stick around in your system for days instead of hours. This isn’t theoretical. The Agency for Healthcare Research and Quality found that 35% of hospital stays in women over 65 are caused by bad reactions to medications. That’s not bad luck. That’s a system failing to adapt to biology.
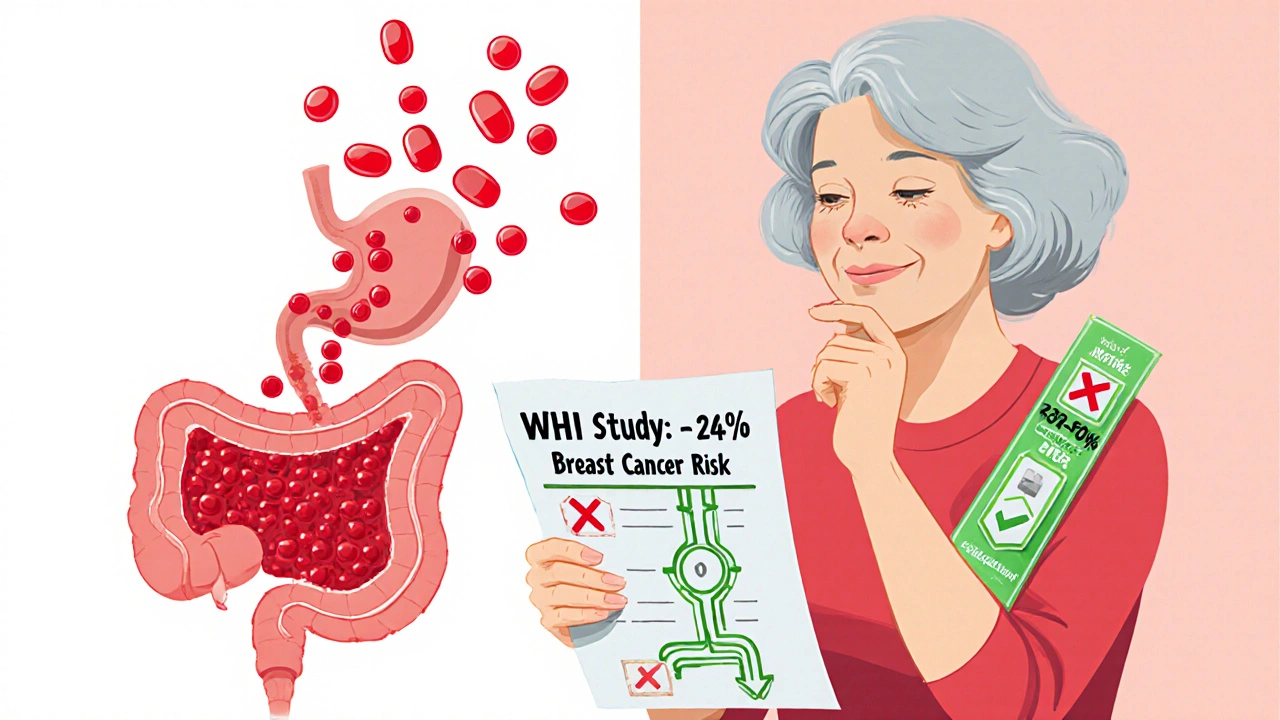
Hormone Therapy: The Real Risks Behind the Labels
Estrogen therapy isn’t the simple fix it was once thought to be. The FDA requires black box warnings on all estrogen products for increased risk of stroke, blood clots, and breast cancer. But here’s what most women don’t know: the route of delivery changes everything.
Oral estrogen-pills-goes straight to your liver. That triggers clotting factors. Transdermal estrogen-patches, gels, sprays-bypasses the liver. Studies show this cuts venous thromboembolism risk by 30 to 50%. If you have a history of clots, migraines with aura, or high triglycerides, oral estrogen is dangerous. Transdermal might still be an option, but only under close monitoring.
The Women’s Health Initiative study still shapes today’s guidelines. Combined estrogen-progestin therapy increased breast cancer risk by 24% after 5.6 years. Estrogen alone-only for women who’ve had hysterectomies-showed no increase in breast cancer, and even a slight drop. But the USPSTF says even that isn’t worth it for preventing heart disease or osteoporosis in women over 60. The harms outweigh the benefits. So why do doctors still prescribe it? Often because patients are desperate for relief from night sweats. The key is timing. Starting hormone therapy within 10 years of menopause, or before age 60, may offer heart protection. After that? The risk skyrockets.
Polypharmacy: The Silent Killer in Medicine Cabinets
Forty-four percent of women over 65 take five or more prescription drugs. That’s not unusual. It’s normal. And it’s deadly. Each additional pill multiplies your chance of a bad reaction. The WHO calls this a global crisis. Why? Because most doctors treat one condition at a time. Your cardiologist prescribes a beta-blocker. Your rheumatologist adds an NSAID. Your gynecologist prescribes a vaginal estrogen. None of them talk to each other.
Here’s what happens in real life: Mrs. Poly, a 72-year-old in a WHO case study, was on diclofenac for arthritis, simvastatin for cholesterol, enalapril for blood pressure, and atenolol for heart rate. She kept taking the diclofenac even after her doctor told her to stop. Within a week, she was hospitalized with a bleeding ulcer. Her hemoglobin dropped from 12.5 to 8.1. That’s severe anemia. All because one pill was ignored.
The Beers Criteria, updated in 2019, lists 30 medications older adults should avoid. Long-acting benzodiazepines like diazepam? They double the risk of hip fractures. Anticholinergics like diphenhydramine (Benadryl)? They raise dementia risk. Even some heartburn meds like proton pump inhibitors can weaken bones over time. The problem isn’t just what’s prescribed-it’s what’s still sitting in your cabinet from 10 years ago.
Deprescribing: The Forgotten Treatment
Most doctors don’t know how to stop prescribing. They know how to start. But sometimes, the best medicine is no medicine at all. Deprescribing-systematically reducing or stopping drugs that aren’t helping or are causing harm-isn’t optional. It’s essential.
Studies show that structured deprescribing reduces medication burden by 1.4 drugs per patient and cuts adverse events by 33%. But it’s not a quick fix. Tapering off antidepressants takes 4 to 8 weeks. Benzodiazepines need 8 to 12 weeks. Abrupt stops can trigger seizures, panic attacks, or rebound insomnia.
Ask your doctor: “Is this medication still necessary?” “What happens if I stop it?” “Are there non-drug options?” Use the START/STOPP criteria-a tool doctors use to spot inappropriate prescriptions and missed opportunities. If you’re on a drug that’s on the Beers list, push for a review. Don’t wait for your annual checkup. Bring your pill organizer to your next visit.
Non-Hormonal Alternatives That Actually Work
You don’t need estrogen to manage hot flashes. SSRIs like paroxetine (Brisdelle) are FDA-approved for hot flashes and reduce them by 50 to 60%. But here’s the catch: 30 to 40% of women report sexual side effects-low desire, trouble reaching orgasm. Gabapentin and clonidine work too, though they cause dizziness or dry mouth. Lifestyle changes help more than you think. Cooling your bedroom, wearing layers, avoiding spicy food and alcohol-these simple steps reduce hot flashes by 30% in many women.
For bone health, calcium and vitamin D aren’t enough. Weight-bearing exercise like walking, dancing, or resistance training is proven to maintain bone density better than any supplement. The National Institute on Aging recommends 30 minutes a day, five days a week. For heart health, aspirin lowers stroke risk by 24% in women over 45-but increases bleeding risk by 58% after 65. That’s why you shouldn’t take it unless your doctor says so. Don’t self-prescribe.

What You Can Do Today
Start with your medicine cabinet. Pull out every pill, bottle, and supplement. Write down: name, purpose, dose, time of day, and who prescribed it. Bring this list to every appointment-even if you’re seeing a new doctor. Use a pill organizer. They cut medication errors by 81%, according to JAMA Internal Medicine. But don’t just use it. Check it every morning. Are you taking the same pill twice? Are you skipping doses? 42% of errors are double doses. 38% are missed doses. You’re not alone. But you can fix it.
Ask for a brown bag review: bring everything you take to your provider. Let them see it. Let them ask, “Why are you still taking this?” If your doctor doesn’t know about the Beers Criteria or deprescribing, find one who does. You have the right to ask. You have the right to safety.
And if you’re considering hormone therapy? Don’t rush. Ask: Is it for symptom relief or disease prevention? If it’s the latter, the answer is almost always no. If it’s for severe hot flashes, ask for transdermal estrogen, not pills. And always, always get your liver and clotting tests checked first.
Future of Medication Safety for Post-Menopausal Women
Research is moving fast. Tissue-selective estrogen complexes (TSECs), like conjugated estrogens with bazedoxifene, reduce endometrial cancer risk by 70% compared to traditional hormone therapy. Pharmacogenomics-testing your genes to see how you metabolize drugs-is becoming more accessible. If you’re on tamoxifen, for example, a CYP2D6 test can tell you if it’ll work for you at all.
AI tools are now being tested to flag dangerous drug combinations before they’re prescribed. One pilot study reduced medication errors by 45%. But none of this matters if you’re not involved in your own care. The most powerful tool you have isn’t a pill or a patch. It’s your voice. Speak up. Ask questions. Demand clarity. Your health isn’t a checklist. It’s your life.
Is hormone therapy safe for post-menopausal women?
Hormone therapy can be safe for some women, but only under strict conditions. It’s generally recommended for symptom relief in women under 60 or within 10 years of menopause. Transdermal estrogen (patches or gels) is safer than oral pills because it doesn’t increase clotting risk as much. It’s not safe if you have a history of breast cancer, blood clots, stroke, liver disease, or unexplained vaginal bleeding. Never use it to prevent heart disease or osteoporosis-that’s no longer supported by guidelines.
How many medications are too many for a post-menopausal woman?
Taking five or more medications daily is considered polypharmacy, which increases the risk of side effects and dangerous interactions. The average post-menopausal woman takes 4 to 5 prescriptions, but studies show that 15% are taking inappropriate drugs. The goal isn’t to reduce pills for the sake of it-it’s to keep only what’s necessary. If a drug isn’t helping or is causing harm, it should be stopped, not added to.
Can I stop my blood pressure or cholesterol meds if I feel fine?
No. Feeling fine doesn’t mean the medication isn’t working. High blood pressure and cholesterol often have no symptoms until damage is done. Stopping them suddenly can cause heart attack, stroke, or dangerous spikes in pressure. If you want to reduce or stop a medication, talk to your doctor first. They can guide a safe taper or test whether lifestyle changes have made it unnecessary.
What are the most dangerous medications for older women?
The Beers Criteria lists 30 high-risk drugs for people over 65. Top offenders include long-acting benzodiazepines (like Valium), which increase hip fracture risk by 50%; anticholinergics like Benadryl, linked to dementia; and NSAIDs like ibuprofen or naproxen, which can cause stomach bleeding and kidney damage. Even some heartburn meds (PPIs) can weaken bones over time. Always ask: Is this still necessary? Is there a safer alternative?
How can I avoid medication errors at home?
Use a pill organizer with compartments for each day and time. Check it every morning. Keep a written list of every medication-including supplements-and bring it to every doctor visit. Never take a pill from an old bottle unless you’re sure what it is. Ask your pharmacist to review your list. And don’t be afraid to say, “I’m not sure why I’m taking this.” Many errors happen because patients don’t understand their own meds.
Are non-hormonal options effective for hot flashes?
Yes. SSRIs like paroxetine (Brisdelle) reduce hot flashes by 50-60%. Gabapentin and clonidine also work, though they may cause dizziness. Lifestyle changes help too: sleeping in a cool room, wearing breathable layers, avoiding alcohol and spicy food, and practicing paced breathing can cut symptoms by 30%. You don’t need hormones to feel better-just the right combination of tools.
Conor McNamara
November 19, 2025 AT 12:09they’re hiding the real truth-pharma’s been pushing estrogen patches like they’re magic crystals while quietly burying the studies that show they still spike clotting in women with MTHFR mutations. i’ve seen it in my aunt’s bloodwork. no one talks about this. the FDA? bought and paid for. you think they care if you bleed out? nah. they just want you on the next pill.
Leilani O'Neill
November 19, 2025 AT 17:07It’s frankly embarrassing that women over 65 are still being prescribed benzodiazepines like they’re candy. This isn’t America-it’s a pharmaceutical feeding ground. Ireland’s NICE guidelines have banned these for over a decade, yet here we are, letting American pharma dictate our grandmother’s medicine cabinet. If you’re still taking diazepam past 60, you’re not managing anxiety-you’re courting a hip fracture and dementia. Wake up.
Riohlo (Or Rio) Marie
November 21, 2025 AT 05:40Oh, sweet mercy. Let’s talk about the real tragedy: the medical-industrial complex has turned menopause into a profit pipeline. Estrogen patches? $800/month. SSRIs for hot flashes? $1,200. Meanwhile, the one intervention proven to reduce vasomotor symptoms by 40%-daily walking-isn’t patented, isn’t promoted, and isn’t reimbursed. Doctors don’t want to talk about lifestyle because they can’t bill for it. So we get a cocktail of drugs that turn our bodies into chemical soups. And we’re supposed to be grateful? Please. This isn’t medicine. It’s capitalism with a stethoscope.
And don’t get me started on the ‘brown bag review.’ That’s not a medical practice-it’s a trauma dump. You’re supposed to haul your entire pharmacy to a 10-minute appointment and hope the doctor doesn’t roll their eyes? Meanwhile, the Beers Criteria is a 12-page PDF nobody reads. The system isn’t broken. It’s designed to fail us.
I’ve watched my mother taper off three meds in six months. She cried. She panicked. She thought she’d die without the gabapentin. But after three weeks? Her brain fog lifted. Her balance improved. Her doctor didn’t even document it. Because ‘de-prescribing’ isn’t a CPT code. It’s a conspiracy theory to them.
And yet, here we are. Women over 65 are the most medicated demographic on earth. And the only thing more dangerous than the pills? The silence around them. We’re being drugged into compliance while our autonomy is quietly erased. Wake up. Your body is not a drug receptacle.
steffi walsh
November 21, 2025 AT 22:20I just started a brown bag review with my pharmacist last week and it changed everything. I realized I’d been taking a pill for acid reflux for 8 years-even though I stopped eating spicy food in 2019. She helped me cut it out and now I don’t feel like a zombie every morning. 🙏 You don’t need to be a genius to do this-just brave enough to ask, ‘Why am I still taking this?’
Yash Nair
November 21, 2025 AT 23:58you people are so weak. in india we dont take 5 pills a day we just eat turmeric and chill. you think your body is so special? your medicine cabinet is your weakness. stop blaming pharma and start being strong. my grandma at 78 walks 10km a day and never took a single pill. you are all just lazy.
Bailey Sheppard
November 23, 2025 AT 01:04Really appreciate this breakdown. I’m a nurse and I see this every day-women on 7 meds, none of them talking to each other. The biggest shift? When we start asking, ‘What if we stopped this?’ instead of ‘What else can we add?’ It’s not about being anti-medication. It’s about being pro-wellness. One woman I worked with cut her statin, and her muscle pain vanished. She’s now hiking every weekend. Simple changes, huge impact.
Girish Pai
November 24, 2025 AT 14:45The pharmacokinetic shifts post-menopause are a direct consequence of CYP450 enzyme downregulation due to estrogen withdrawal. This creates a non-linear pharmacodynamic curve that disproportionately elevates AUC and Cmax for lipophilic compounds. The Beers Criteria, while well-intentioned, lacks granular pharmacogenomic stratification. We need precision deprescribing protocols calibrated to CYP2D6, CYP3A4, and UGT1A1 haplotypes-not population-based heuristics.
Kristi Joy
November 25, 2025 AT 20:38For anyone reading this and feeling overwhelmed-start small. Pick one pill. Just one. Ask your doctor: ‘Is this still helping me?’ Write down their answer. You don’t have to fix everything today. But you deserve to understand why you’re taking what you’re taking. You’re not a burden. You’re not ‘too old.’ You’re a person who’s earned the right to be heard. And you’re not alone.
Hal Nicholas
November 26, 2025 AT 20:58They’re all just scared. Scared of death. Scared of aging. So they swallow pills like they’re prayers. But the truth? No drug can fix what society refuses to acknowledge: we don’t value older women. We medicate their pain because we don’t know how to sit with it. And the doctors? They’re just following the script. The real crisis isn’t polypharmacy-it’s loneliness. No one’s asking if you’re lonely. They’re just giving you another pill.