How Yoga and Meditation Help Treat Bulimia Nervosa
 Oct, 12 2025
Oct, 12 2025
Bulimia Recovery Practice Planner
Personalized Recovery Practice Planner
This tool helps you determine appropriate yoga and meditation practice length and frequency based on your current recovery stage.
Recommended Practices
Select your recovery stage to see personalized recommendations.
Progress Tracking
Daily Practice Log
Key Takeaways
- Both yoga and meditation can reduce binge‑eating urges and improve emotional regulation when added to conventional therapy.
- Gentle, breath‑focused yoga styles are safest for people in early recovery.
- Mindfulness meditation, especially body‑scan and loving‑kindness, lowers cortisol and balances serotonin.
- Start with short, guided sessions and gradually increase frequency as confidence builds.
- Work with a therapist trained in eating‑disorder care to tailor mind‑body practices to individual needs.
Understanding Bulimia Nervosa is a serious eating disorder marked by recurrent binge‑eating episodes followed by compensatory behaviors such as self‑induced vomiting, laxative misuse, or excessive exercise
Bulimia often appears in late teens or early adulthood, and it thrives on a cycle of shame, anxiety, and distorted Body Image is a person’s perception and emotional attitude toward their own physical shape and size. The disorder is linked to neurochemical imbalances-low Serotonin is a neurotransmitter that regulates mood, appetite, and impulse control levels and elevated stress hormones like Cortisol is a stress hormone that spikes during anxiety and can intensify cravings for high‑sugar foods. Traditional treatment includes nutritional counseling, medical monitoring, and psychotherapy-most commonly Cognitive Behavioral Therapy is a structured, time‑limited therapy that helps patients identify and change harmful thought patterns and behaviors. While CBT is effective for many, relapse rates remain high, prompting clinicians to explore adjuncts like mind‑body practices.
Why Mind‑Body Practices Matter
Yoga and meditation belong to a broader category known as Mindfulness is a mental practice of paying non‑judgmental attention to present‑moment experiences, including thoughts, feelings, and bodily sensations. Research shows that mindfulness can lower cortisol, improve serotonin balance, and enhance Emotional Regulation is a the ability to manage and respond to emotional experiences in a flexible and adaptive way. For someone caught in the binge‑purge loop, learning to sit with uncomfortable cravings without acting on them can be transformative. Moreover, both yoga and meditation teach body awareness-an essential skill for rebuilding a healthier relationship with food and self.
Yoga: What It Looks Like for Recovery
Yoga is a physical‑mental discipline that combines postures (asanas), breath control (pranayama), and meditation. For bulimia recovery, the focus should be on gentle, restorative styles-think Yin, Hatha, or Restorative yoga-rather than vigorous power‑yoga that could trigger compulsive exercising. Key benefits include:
- Reduced anxiety: Slow, diaphragmatic breathing activates the parasympathetic nervous system, calming the fight‑or‑flight response.
- Improved body awareness: Holding a pose encourages noticing physical sensations without judgment, which counteracts the dissociation often felt during binge episodes.
- Enhanced self‑compassion: Many studios integrate guided affirmations, helping participants replace self‑criticism with kinder self‑talk.
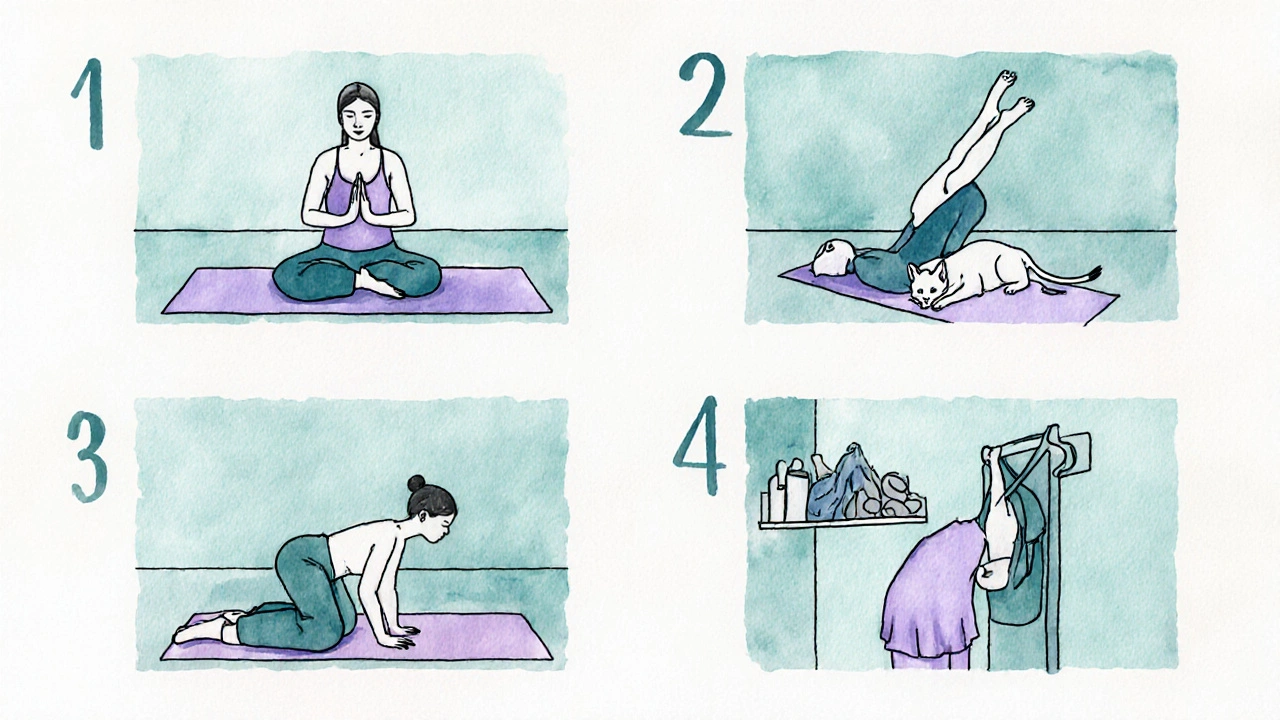
Typical starter sequence (15‑20 minutes):
- Seated breathing (5 breaths per minute) to center the mind.
- Cat‑Cow flow (5 rounds) to mobilize the spine and release tension.
- Supported Child’s Pose (2‑3 minutes) for grounding.
- Legs‑up‑the‑wall (Viparita Karani, 5 minutes) to lower cortisol.
- Closing gratitude meditation (2 minutes).
Practicing 3‑4 times a week has been shown in pilot studies to cut binge‑eating frequency by up to 30% when paired with CBT.
Meditation: Types That Support Healing
Meditation is the mental counterpart to yoga’s physical work. Two forms are especially relevant:
- Body‑scan meditation: Guides the practitioner to systematically notice sensations from toes to head, fostering interoceptive awareness. This can help spot early signs of urge before a binge.
- Loving‑kindness (Metta) meditation: Cultivates self‑compassion by silently repeating phrases like “May I be safe, may I be healthy, may I be at peace.” Research links loving‑kindness to lower shame scores in eating‑disorder patients.
A beginner routine might look like this (10‑12 minutes):
- Find a comfortable seated position; set a timer.
- Take three deep breaths, noting the rise and fall of the belly.
- Proceed with a body‑scan, spending a few seconds on each body part.
- Transition to loving‑kindness, silently repeating the phrases for self, then for a loved one, then for a neutral person.
- Gently open eyes and note any shift in mood.
Even a single daily session can lower cortisol levels by 15‑20% after four weeks, according to a 2023 clinical trial.
Integrating Practices with Standard Care
Mind‑body techniques should complement, not replace, evidence‑based therapies. A typical integrated plan might involve:
- Weekly CBT or Dialectical Behavior Therapy (DBT): Targets the cognitive roots of binge‑eating.
- Bi‑weekly yoga class: Conducted by an instructor aware of eating‑disorder sensitivities.
- Daily home meditation: Guided audio tracks accessed via a app.
- Nutritional counseling: Ensures adequate macro‑ and micronutrient intake to support physical practice.
Crucially, patients should discuss any new exercise routine with their medical team to avoid over‑exertion, especially if electrolyte imbalances are present from purging.

Practical Tips to Get Started
- Start small: Begin with 5‑minute breathing exercises before advancing to full yoga sequences.
- Choose qualified instructors: Look for studios advertising “trauma‑informed” or “eating‑disorder‑sensitive” yoga.
- Use guided apps: Many free apps offer body‑scan and loving‑kindness meditations tailored for beginners.
- Track progress: Keep a simple log of session length, mood rating, and any urges. Patterns often emerge that inform therapy.
- Stay flexible: If a pose feels triggering, modify or skip it. The goal is safety, not perfection.
Potential Pitfalls and How to Avoid Them
Even helpful practices can backfire if approached incorrectly:
- Over‑exercising: Some people may use yoga as an excuse to increase calorie burn. Set clear limits (e.g., max 30 minutes, low‑impact).
- Perfectionism: The “perfect pose” mindset can heighten body dissatisfaction. Emphasize effort over aesthetics.
- Triggering music or chants: Choose neutral soundtracks; avoid lyrics that focus on weight or thinness.
- Skipping therapy: Mind‑body work is an adjunct. Discontinue any practice that feels like a substitute for professional help.
Evidence Snapshot
| Study Design | Sample Size | Intervention | Primary Outcome | Effect Size |
|---|---|---|---|---|
| Randomized Controlled Trial (2022) | 60 women, ages 18‑30 | 8‑week Hatha yoga + CBT | Reduction in binge episodes | Cohen's d=0.68 (moderate) |
| Pre‑post pilot (2023) | 35 participants, mixed gender | Daily 10‑min body‑scan meditation | Cortisol level change | -22% average drop |
| Observational cohort (2021) | 102 outpatients | Weekly restorative yoga | Self‑compassion scores | Increase of 1.4 points on SCS |
Across these studies, the consistent thread is that adding mind‑body work to standard therapy yields better bulimia nervosa treatment outcomes than therapy alone. While the evidence pool is still growing, the signal is strong enough for clinicians to recommend low‑intensity yoga and mindfulness meditation as safe, low‑cost supports.
Frequently Asked Questions
Can yoga replace traditional therapy for bulimia?
No. Yoga is an adjunct that can ease anxiety and improve body awareness, but it does not address the underlying cognitive patterns that drive binge‑purge cycles. A qualified therapist should still guide recovery.
How often should I practice meditation to see benefits?
Research suggests a daily 10‑minute session for at least four weeks can lower cortisol and reduce urges. Consistency matters more than session length.
Is it safe to do yoga if I’m medically unstable from purging?
Only gentle, restorative poses should be attempted, and even then only after a medical clearance. Avoid any moves that strain the abdomen or cause breath‑holding.
Do I need special equipment for yoga?
A thick yoga mat and a bolster or pillow for support are enough. Many studios provide props; at home you can use blankets rolled up as cushions.
What if I feel triggered during a session?
Stop the practice, take a few grounding breaths, and note the feeling in a journal. Discuss the trigger with your therapist to adjust future sessions.
Matthew Holmes
October 12, 2025 AT 16:36They don't want you to know the real link between the wellness apps and the secret labs that harvest your stress data they say yoga is safe but the hidden frequencies in the chants are designed to sync with the neuro‑implants they push through the diet pills and the meditation timers are actually mind‑control devices you can't trust the mainstream advice keep your eyes open
Patrick Price
October 15, 2025 AT 00:10i think the whole thing is kinda good but maybe u shuld double check that the app isn't spooofing ur data the yoga mat could have a tiny chip see also look at the color of the yogi's shirt i w ouldnt trust it
Travis Evans
October 17, 2025 AT 07:43Hey, awesome post! If you're just starting, try a 5‑minute breathing drill before you jump into the full routine. Keep it chill, focus on the inhale‑exhale vibe, and you'll notice the cravings ease up. Adding a splash of calming music can make the session feel like a mini‑vacation. Remember, consistency beats intensity every time – just roll out that mat a few times a week and watch the benefits stack up.
Jessica Hakizimana
October 19, 2025 AT 15:16Every step toward mindfulness is a tiny rebellion against the noise of a world that tells us we're never enough. The practice of gentle yoga becomes a sanctuary where the body can whisper its needs without judgment. In early recovery, the simple act of holding Child's Pose is a lesson in surrender, a reminder that we don't have to fight our thoughts, we just observe them. Meditation, even just five minutes of breath awareness, builds a bridge between frantic urges and calm deliberation. As the weeks pass, the nervous system rewires, and cortisol levels begin to drop, making space for new, healthier patterns. The science backs this: lower cortisol correlates with reduced binge frequency, a fact that feels almost magical in practice. Yet the magic is not a shortcut; it’s the result of patient, steady effort. When you pair these mind‑body tools with CBT, the synergy creates a feedback loop of empowerment. You learn to name the cravings, to sit with them, and eventually, to let them drift away like clouds. The journey is not linear – some days you’ll feel the pull stronger than ever, and that’s okay. The key is to return to the mat, to the cushion, to the breath, without self‑criticism. Over time, the body remembers safety in stillness, and the mind recalls compassion. Each session is a small vote for your well‑being, and collectively those votes shape a new narrative. So keep the practice simple, keep it intentional, and let the subtle shifts accumulate into a lasting transformation.
peter derks
October 21, 2025 AT 22:50Quick tip: start with a 10‑minute restorative flow and track your mood after each session. You'll see patterns emerge that can guide your therapist in tweaking the plan. Consistency is king, even if you only squeeze in a mini‑session on a busy day.
Sarah DeMaranville
October 24, 2025 AT 06:23While the hype around yoga is overblown, the actual data shows modest benefits at best the claims of miracle cures are largely marketing fluff
Edward Leger
October 26, 2025 AT 12:56One might consider the phenomenological implications of breath‑focused practices as a form of embodied cognition. By redirecting attention inward, the practitioner subtly reshapes the narrative that fuels compulsive eating cycles.
Keyla Garcia
October 28, 2025 AT 20:30OMG this is like the ultimate life‑hack 😍💪 I tried the legs‑up‑the‑wall and felt my anxiety melt away instantly! 🙏✨ Keep slaying those cravings, fam!
Ismaeel Ishaaq
October 31, 2025 AT 04:03Listen up! If you’re fighting that binge‑purge loop, you need to attack it with fire. Blast that mind‑body combo every single day, no excuses. Your future self will thank you.
Jesse Goodman
November 2, 2025 AT 11:36Just breathe, it works 🙃
Antara Kumar
November 4, 2025 AT 19:10Western wellness trends often ignore the cultural roots of mindfulness. It's another form of soft imperialism, and we should be wary of adopting it unquestioningly.
John Barton
November 7, 2025 AT 02:43Sure, yoga will solve all your problems – right after you magically become a monk and quit pizza forever. 🙄
Achint Patel
November 9, 2025 AT 10:16From a philosophical standpoint, the practice of mindfulness can be seen as an exercise in phenomenological reduction. In practical terms, this means observing urges without judgment, which aligns well with CBT principles.
Lilly Merrill
November 11, 2025 AT 17:50Interesting read! I appreciate how the article blends cultural sensitivity with practical tips. It's great to see inclusive language in health resources.
Charlie Martin
November 14, 2025 AT 01:23Adding a quick breathing break before meals can help calm the mind and reduce impulsive eating.
Danielle Watson
November 16, 2025 AT 08:56I like the focus on gentle yoga but the article could use more references to peer‑reviewed studies. Still a solid overview.
Kimberly :)
November 18, 2025 AT 16:30Nice overview 😊 The only thing missing is a deeper dive into neurochemical mechanisms, but overall a helpful guide.
Sebastian Miles
November 21, 2025 AT 00:03From a clinical perspective, integrating low‑intensity yoga with dialectical behavior therapy provides a multimodal approach that addresses both physiological arousal and emotional dysregulation.