Autoimmune Uveitis: Understanding Eye Inflammation and Steroid-Sparing Treatment Options
 Jan, 8 2026
Jan, 8 2026
Autoimmune uveitis isn't something most people hear about until it affects them or someone they love. It’s not just a red eye or a temporary irritation-it’s a serious inflammation inside the eye caused by the body attacking its own tissues. Left unchecked, it can lead to permanent vision loss. And while steroids are often the first line of defense, they come with heavy risks when used long-term. That’s why steroid-sparing therapy is becoming the new standard for people with chronic autoimmune uveitis.
What Exactly Is Autoimmune Uveitis?
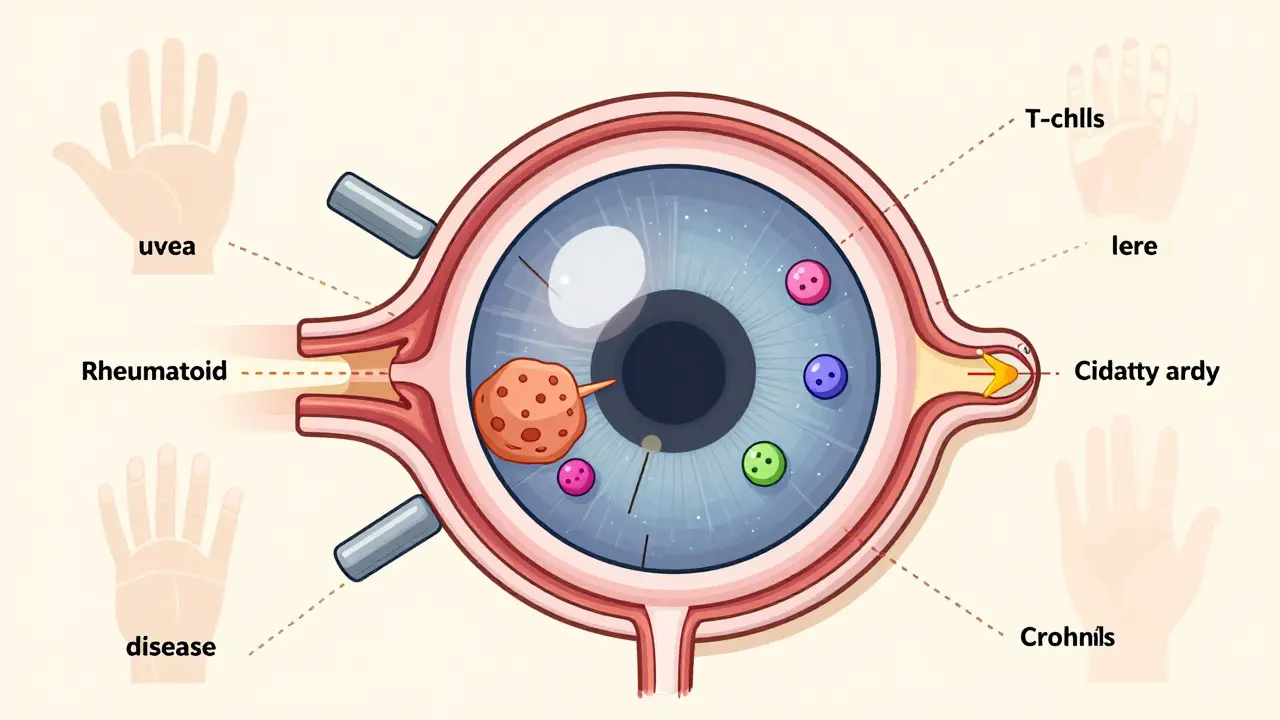
Uveitis means inflammation of the uvea-the middle layer of the eye that includes the iris, ciliary body, and choroid. When it’s autoimmune, your immune system mistakenly targets healthy eye tissue. It’s not caused by an infection like bacteria or viruses. Instead, it’s tied to your body’s own defenses going rogue.This condition doesn’t always show up suddenly. Some people notice blurred vision, light sensitivity, or floaters over days. Others wake up with a red, painful eye. It can strike one eye or both. The symptoms might seem mild at first, but they’re a warning sign. Without treatment, uveitis can trigger cataracts, glaucoma, retinal detachment, or irreversible damage to the optic nerve.
What makes autoimmune uveitis tricky is that it often doesn’t happen alone. It’s linked to other autoimmune diseases like ankylosing spondylitis, rheumatoid arthritis, lupus, Crohn’s disease, psoriasis, and sarcoidosis. If you have one of these conditions and start having eye problems, uveitis should be ruled out immediately.
Why Steroids Are a Double-Edged Sword
Corticosteroids-whether as eye drops, injections, or pills-are powerful at calming inflammation fast. For a sudden flare-up, they’re essential. But here’s the problem: long-term steroid use damages the very thing you’re trying to protect.Using steroid eye drops for months can cause cataracts or raise eye pressure, leading to glaucoma. Oral steroids? They can cause weight gain, bone thinning, high blood sugar, mood swings, and increased infection risk. For someone with uveitis that keeps coming back, these side effects become a bigger threat than the disease itself.
That’s why doctors don’t want patients stuck on steroids. The goal isn’t just to control inflammation-it’s to stop it without relying on drugs that wear down your body over time. This is where steroid-sparing therapy comes in.
What Is Steroid-Sparing Therapy?
Steroid-sparing therapy means using other medications that reduce inflammation by targeting the immune system directly-so you can lower or stop steroids altogether. These aren’t experimental. Many have been used for years in rheumatology and are now standard in uveitis care.Common steroid-sparing drugs include:
- Methotrexate: An old-school immunosuppressant, often used for rheumatoid arthritis. It’s taken weekly, usually as a pill or injection. It’s affordable and well-studied for uveitis.
- Cyclosporine: Works by blocking T-cells, the immune cells that drive inflammation. Requires regular blood tests to monitor kidney function.
- Adalimumab (Humira): The first FDA-approved biologic specifically for non-infectious uveitis. It blocks TNF-alpha, a protein that fuels inflammation. Many patients see rapid improvement and can cut steroid doses by 50% or more.
- Infliximab: Another TNF inhibitor, given by IV. Especially effective in children with uveitis and in cases tied to juvenile arthritis.
These drugs don’t work overnight. It can take weeks or even months to see full benefit. But the payoff is huge: fewer side effects, less vision loss, and better quality of life.
How Doctors Decide Which Treatment to Use
There’s no one-size-fits-all plan. Treatment depends on three things: where the inflammation is, how bad it is, and whether another autoimmune disease is involved.Anterior uveitis (front of the eye) might start with eye drops and a short steroid course. But if it keeps flaring, they’ll add methotrexate or Humira. Posterior uveitis (back of the eye) is harder to treat. It often needs injections or pills from the start. Panuveitis-where the whole eye is inflamed-almost always requires systemic therapy.
Doctors also look at your overall health. If you have Crohn’s disease and uveitis, Humira might treat both at once. If you’ve had tuberculosis before, certain drugs like methotrexate or biologics could reactivate it. That’s why blood tests and screenings are non-negotiable before starting treatment.
Specialized uveitis clinics-now over 50 across the U.S.-bring together ophthalmologists and rheumatologists. This teamwork is critical. One specialist sees the eye damage. The other understands the full autoimmune picture. Together, they design a plan that protects your vision and your body.
Why Humira Changed the Game
Before 2016, almost all uveitis treatments were used off-label. That meant doctors were prescribing drugs approved for arthritis or psoriasis to treat eye inflammation. No formal guidelines. No insurance certainty. No long-term safety data.Then Humira got FDA approval specifically for non-infectious uveitis. That wasn’t just a paperwork change. It meant:
- Insurance companies had to cover it for this use
- Doctors had clear prescribing guidelines
- Patient registries and research studies could now track outcomes
Studies show that patients on Humira or infliximab often achieve complete remission. Many stop steroids entirely within six months. For kids with chronic uveitis, the results are even more dramatic-reduced flare-ups, better school attendance, and less risk of blindness.
It’s not perfect. Humira can increase infection risk. Some people develop antibodies and lose response over time. But compared to lifelong steroids, it’s a massive improvement.
What Happens After You Start Steroid-Sparing Therapy?
You won’t be left on your own. Regular follow-ups are part of the deal. You’ll need:- Monthly eye exams early on, then every 2-3 months
- Visual acuity tests to track vision changes
- Eye pressure checks for glaucoma risk
- OCT scans to look for swelling in the retina
- Blood work every 3-6 months to monitor liver and kidney function
Some people worry about being on immunosuppressants. Yes, you’re more prone to colds or infections. But that doesn’t mean you need to live in isolation. Simple steps help: wash hands often, avoid sick people, get flu and pneumonia shots (but not live vaccines), and tell your doctor if you have a fever or unexplained fatigue.
Many patients report feeling better than they have in years-not just because their vision improved, but because they’re no longer bloated, moody, or scared of steroid side effects.
What’s Next for Uveitis Treatment?
Research is moving fast. Scientists are testing drugs that block other parts of the immune system, like interleukin-6 (IL-6) and JAK pathways. Early results in tough cases show promise.One big frontier is personalized medicine. Right now, doctors guess which drug will work. In the future, blood tests might identify your specific immune signature-like which cytokines are overactive-and match you to the best drug before you even start.
There’s also talk about gene testing to predict who’s likely to respond to biologics or who’s at risk for side effects. This isn’t science fiction-it’s already being studied in major centers.
For now, the message is clear: if you have chronic autoimmune uveitis, don’t accept steroids as your only option. Ask about steroid-sparing therapy. Ask for a referral to a uveitis specialist. The tools to protect your vision are here-and they’re better than ever.
When to Seek Help Immediately
Don’t wait for symptoms to get worse. See an ophthalmologist within 24 hours if you have:- Sudden blurry vision
- Eye pain or redness that doesn’t go away
- Light sensitivity so bad you can’t open your eyes
- Floaters that appear suddenly or increase in number
Early treatment saves sight. Delayed treatment can cost you your vision forever.
Can autoimmune uveitis be cured?
There’s no cure for autoimmune uveitis, but it can be controlled. With the right treatment, many people achieve long-term remission and live without vision loss. The goal isn’t to eliminate the disease entirely-it’s to keep it quiet so it doesn’t damage your eyes.
Are steroid-sparing drugs safe?
They carry risks, like any immune system drug. You might get more infections, or have liver or blood cell changes. But these are monitored closely with regular blood tests. The risks of long-term steroids-like cataracts, glaucoma, and bone loss-are often worse. For most patients, the benefits outweigh the risks.
How long do I need to stay on steroid-sparing therapy?
It depends. Some people need it for years. Others can slowly taper off after 1-2 years of remission. But stopping too soon can cause a flare. Your doctor will guide you based on eye exams, symptoms, and lab results-not just how you feel.
Can I use natural remedies instead of medication?
No. There’s no proven natural treatment for autoimmune uveitis. Supplements, herbs, or diets won’t stop the immune system from attacking your eye. Delaying real treatment can lead to permanent damage. Always work with a specialist.
Is Humira the only biologic approved for uveitis?
Humira was the first, but others are now approved or in late-stage trials. Drugs like adalimumab biosimilars, tocilizumab (an IL-6 blocker), and upadacitinib (a JAK inhibitor) are being used off-label or studied for uveitis. Ask your doctor what’s available and appropriate for your case.
Patty Walters
January 8, 2026 AT 19:14man i wish i knew all this when my mom was going through uveitis 5 years ago. they just threw prednisone at her and said 'good luck'. she got cataracts in both eyes and still can't drive at night. glad things are changing.
Diana Stoyanova
January 9, 2026 AT 15:02OMG YES. I was on steroids for 18 months after my diagnosis and felt like a balloon with anxiety and insomnia. Started Humira last year and it’s like my body finally remembered how to chill. My ophthalmologist said my retina looks better than it has in 7 years. Also, no more moonface. I’m basically a new person. 🙌
tali murah
January 11, 2026 AT 12:22Let me guess-someone got paid to write this PR piece for AbbVie. 'Steroid-sparing therapy' is just corporate speak for 'we’re selling you a $10,000/month biologic instead of a $5 pill.' Don’t be fooled. The real solution is fixing the immune system, not suppressing it with expensive toys. And no, your 'specialized uveitis clinic' isn’t magic-it’s just a billing scheme.
Kiruthiga Udayakumar
January 11, 2026 AT 15:44How is this even still a debate? People are going blind because they’re too lazy to take a pill that costs less than their monthly Netflix subscription. Methotrexate has been around since the 1950s. Why are we still playing Russian roulette with steroids? It’s not rocket science. It’s basic medicine. Stop being passive and start advocating for yourself. Your eyes aren’t replaceable.
Lindsey Wellmann
January 13, 2026 AT 06:03Just wanted to say… I’m crying. 😭 My 8-year-old got diagnosed last year. We went from daily steroid drops to Humira in 3 months. She’s back in soccer, no more glasses, no more ‘I can’t see the board.’ I’m so grateful. Thank you for writing this. 💙
Jeffrey Hu
January 14, 2026 AT 05:07Actually, you missed a key point. Adalimumab isn't the only biologic approved-there's also rituximab, which targets B-cells, and it's been used off-label with great success in refractory cases. Also, JAK inhibitors like tofacitinib are showing 85% remission rates in phase 2 trials. You're cherry-picking the marketing-friendly drugs. Real clinicians know the landscape is way more nuanced.
Ian Long
January 15, 2026 AT 19:25I get why you’re mad, tali. But your anger is missing the point. Yes, drugs are expensive. But the alternative is a 60-year-old blind from steroid-induced glaucoma. That’s not a business model-that’s a tragedy. We need better pricing, sure. But don’t throw the baby out with the bathwater. People are saving their vision. That matters more than your cynicism.
Heather Wilson
January 16, 2026 AT 17:33Wow. This reads like a drug rep’s PowerPoint. Where’s the data on long-term remission? What’s the dropout rate for Humira? How many patients develop TB or lymphoma? You glossed over the black box warnings like they’re footnotes. This isn’t education-it’s advocacy with a side of placebo.
Angela Stanton
January 17, 2026 AT 13:30Let’s be real: the real villain here is the FDA’s approval lag. Biologics were used off-label for uveitis for over a decade before Humira got the nod. That’s not innovation-that’s bureaucratic inertia. And now that it’s approved, insurance is forcing patients to fail 3 other drugs first. It’s a goddamn obstacle course. We need faster access, not more pamphlets.
Gregory Clayton
January 17, 2026 AT 22:18So we’re paying $20K a year so some guy in a lab coat can avoid giving out steroids? Meanwhile, in China they’re using traditional herbs with 70% success. Why are we letting Big Pharma dictate eye care? This is why America’s healthcare is a joke.
Johanna Baxter
January 19, 2026 AT 08:33I lost my vision in one eye because I waited 6 months to see a specialist. They told me it was 'just allergies.' I’m 32. I’ll never get that back. Please. If you have any of these symptoms-GO. NOW. Don’t wait. Don’t Google. Don’t wait for insurance. Just go.
Phil Kemling
January 20, 2026 AT 02:46It’s ironic, isn’t it? We treat the immune system like an enemy to be crushed-when maybe it’s just confused. Maybe uveitis isn’t a defect in the system, but a signal that something deeper is out of alignment. Diet? Stress? Environmental toxins? We treat the eye like a separate machine, but the body isn’t modular. Maybe the cure isn’t in a pill at all-it’s in listening.
Maggie Noe
January 20, 2026 AT 19:42Phil, you’re onto something. I used to think meds were the answer-until I started doing breathwork, cutting out gluten, and sleeping 8 hours. My flares dropped 80%. I’m still on Humira for safety, but my doctor says my biomarkers look like a 25-year-old’s. Maybe it’s not either/or. Maybe it’s both. We’re so obsessed with the pill that we forget the person.
Ashley Kronenwetter
January 20, 2026 AT 20:02As a clinical nurse specialist in rheumatology, I’ve seen patients transition from prednisone dependence to steroid-free remission with methotrexate and adalimumab. The data is robust. The key is early intervention and multidisciplinary care. This post accurately reflects current guidelines. Those who dismiss biologics as 'corporate tools' misunderstand the severity of sight-threatening inflammation.
Jerian Lewis
January 21, 2026 AT 02:39Everyone’s talking about drugs. But what about the emotional toll? I was diagnosed at 24. I thought I’d go blind by 30. I cried every night for a year. The meds helped my eyes-but therapy helped me live. Don’t ignore the mental health piece. This disease doesn’t just attack your retina. It attacks your soul.