Zoonotic Diseases: How Animal-to-Human Infections Spread and How to Stop Them
 Jan, 4 2026
Jan, 4 2026
More than 60% of all known infectious diseases in humans come from animals. That’s not a guess-it’s a fact backed by the World Health Organization. Every time you handle a pet, eat undercooked meat, get bitten by a tick, or even walk through a forest where wild animals live, you’re at risk of coming into contact with a zoonotic disease. These aren’t rare oddities. They’re common, dangerous, and often preventable.
What Exactly Are Zoonotic Diseases?
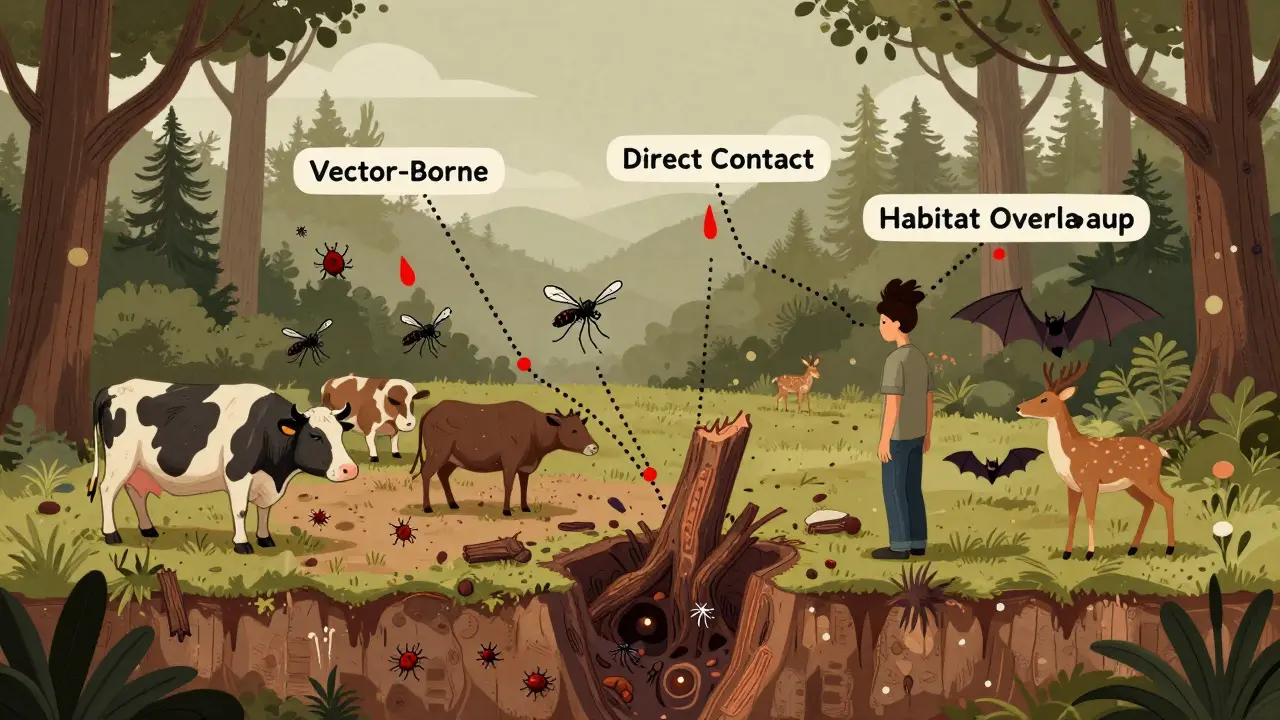
Zoonotic diseases, or zoonoses, are infections that jump from animals to people. The pathogens behind them can be viruses, bacteria, parasites, or fungi. Some are well-known-like rabies, Lyme disease, and salmonella. Others are less familiar, like Q fever or trichinosis. But they all share one thing: they start in animals and find their way into humans. Rabies is the oldest scientifically documented zoonosis. Louis Pasteur developed the first vaccine for it in 1885. But humans have been getting sick from animals for thousands of years. Ancient Greek physician Hippocrates wrote about anthrax in livestock affecting people back in 400 BCE. Today, these diseases are more common than ever. About 75% of new diseases emerging in humans-like Ebola, COVID-19, and Nipah virus-originated in animals.How Do These Diseases Jump to Humans?
There are five main ways zoonotic diseases spread:- Direct contact: Touching, petting, or being bitten by an infected animal. A dog with rabies, a cat with cat scratch disease, or a reptile carrying salmonella can all pass the infection directly.
- Indirect contact: Coming into contact with surfaces or environments contaminated by animals. Cleaning a birdcage, touching a turtle tank, or walking barefoot in soil where livestock defecated can expose you.
- Vector-borne: Bites from ticks, mosquitoes, or fleas. Lyme disease spreads through tick bites. West Nile virus comes from mosquitoes that fed on infected birds.
- Foodborne: Eating undercooked meat, raw milk, or eggs contaminated with bacteria like Salmonella, E. coli, or Listeria. The CDC says 1 in 6 Americans get sick from contaminated food every year-and many of those cases come from animals.
- Waterborne: Drinking or swimming in water polluted by animal waste. Giardia, a parasite that causes severe diarrhea, often spreads this way.
Common Zoonotic Diseases You Should Know
Here are some of the most frequent and dangerous ones:- Rabies: Almost always fatal once symptoms appear. Spread by bites from infected dogs, bats, raccoons, or skunks. Vaccinating pets cuts human cases by 90%.
- Salmonella: Often from reptiles, birds, or undercooked poultry. Symptoms: fever, diarrhea, stomach cramps. A Wisconsin family got sick from pet turtles-two kids ended up in the hospital.
- Lyme disease: Caused by bacteria carried by ticks. Early signs include a bull’s-eye rash and flu-like symptoms. Left untreated, it can damage your heart, joints, and nervous system.
- Brucellosis: From unpasteurized milk or undercooked meat from infected cows, goats, or pigs. Causes fever, sweating, joint pain. Common among farmers and veterinarians.
- Toxoplasmosis: From cat feces or undercooked meat. Especially dangerous for pregnant women-it can cause birth defects.
- Psittacosis: Also called parrot fever. Spread by birds like parrots and chickens. One poultry farmer spent 14 days in the hospital after catching it from his flock.
- Ringworm: Not a worm-it’s a fungal infection. Easily passed from pets, especially dogs and cats. Causes itchy, circular rashes on the skin.
Why Are These Diseases Getting Worse?
It’s not just bad luck. Human behavior is making zoonotic diseases more likely to spread. Deforestation and land development push people into wildlife habitats. That’s why 31% of new zoonotic outbreaks are linked to habitat loss. The wildlife trade-selling live animals in markets-spreads pathogens across continents. Agricultural expansion brings livestock into closer contact with wild animals. Climate change expands the range of ticks and mosquitoes, making diseases like Lyme and dengue spread into new areas. Dr. Anthony Fauci once said: “About four out of every five emerging infectious diseases come from animals.” That’s not a warning-it’s a pattern. And it’s accelerating.Who’s at Highest Risk?
Some people are more exposed than others:- Veterinarians: 8 times more likely to get zoonotic infections than the general public.
- Farmers and livestock workers: 5.2 cases per 1,000 workers each year.
- Pet owners: 23% have had exposure to zoonotic diseases. Ringworm and cat scratch disease are the most common.
- Children under 5: More likely to put things in their mouths and have close contact with pets. Salmonella from turtles is a top cause of hospitalization in toddlers.
- Travelers: Visiting areas with poor sanitation or exotic animal markets increases risk.
How to Protect Yourself-Simple, Proven Steps
You don’t need a lab coat to stay safe. Here’s what actually works:- Wash your hands: After handling animals, cleaning cages, or before eating. Twenty seconds with soap reduces transmission by 90%. Use a timer if you need to.
- Cook meat properly: Poultry must reach 165°F. Ground beef should hit 160°F. Use a food thermometer-guessing doesn’t work.
- Don’t kiss your pets: Saliva can carry bacteria. Avoid letting animals lick your face or open wounds.
- Use gloves: When cleaning litter boxes, handling animal waste, or gardening in soil where animals roam. A 2021 study found this cuts infection risk by 85%.
- Keep pets vaccinated: Rabies, leptospirosis, and other vaccines protect both animals and people.
- Check for ticks: After hiking or being in grassy areas. Remove them with tweezers within 24 hours to prevent Lyme disease.
- Avoid wild animals: Don’t touch, feed, or adopt them. Even cute baby animals can carry deadly pathogens.
- Don’t buy exotic pets: Reptiles, primates, and wild birds are high-risk carriers. Many states ban them for good reason.
Why the One Health Approach Matters
You can’t solve zoonotic diseases by treating only humans. That’s why experts call it “One Health”-the idea that human, animal, and environmental health are deeply connected. In Uganda, vaccinating 70% of dogs against rabies led to a 92% drop in human cases. In the U.S., only 28 states require all zoonotic diseases to be reported. That’s a gap. When a farmer gets sick from brucellosis, the health department should notify the agriculture agency. When a deer dies from a strange illness, wildlife officials should alert public health. But most places don’t have systems to connect those dots. The CDC, WHO, and FAO are pushing for integrated surveillance. Countries with full One Health coordination have reduced outbreaks by 37%. That’s not a small win-it’s life-saving.What’s Next? The Future of Zoonotic Disease Control
The global market for zoonotic disease testing is expected to grow to over $3 billion by 2028. New tools are coming-faster lab tests, AI-driven outbreak prediction models, and drone-based wildlife monitoring. But technology alone won’t fix this. The real solution is better training. Right now, 68% of doctors in the U.S. haven’t received enough education to recognize zoonotic diseases. That means people get misdiagnosed, treated with the wrong antibiotics, or sent home too early. Climate change will make things harder. By 2050, the area in North America suitable for Lyme disease could increase by 45%. The World Bank says investing $10 billion a year in One Health programs could prevent 70% of future pandemics-and save $1 trillion in economic damage.Final Thought: It’s Not About Fear-It’s About Awareness
Zoonotic diseases aren’t something to panic about. They’re something to understand. You don’t have to give up your pets or stop eating meat. You just need to know the risks and take simple steps to reduce them. A child with a pet turtle isn’t doomed. A farmer working with cattle isn’t doomed. A hiker walking through the woods isn’t doomed. But without basic precautions-handwashing, cooking meat right, checking for ticks-those risks become real. The next pandemic won’t come from nowhere. It will start with an animal. And the next time it does, the difference between a controlled outbreak and a global crisis will come down to what we do today.Can you get sick from your pet dog or cat?
Yes. Dogs and cats can carry bacteria like Salmonella, Campylobacter, and ringworm fungi. Cat scratch disease, caused by Bartonella bacteria, is common in people who get scratched or licked on open skin. Always wash your hands after petting your animal, especially before eating. Keep their nails trimmed and avoid letting them lick your face.
Is it safe to eat raw meat or unpasteurized milk?
No. Raw or undercooked meat can contain E. coli, Salmonella, or Toxoplasma. Unpasteurized milk can carry Listeria, Brucella, and other dangerous bacteria. These pathogens don’t disappear just because the product is labeled “organic” or “natural.” Cooking meat to safe temperatures and choosing pasteurized dairy are the only reliable protections.
Do I need to get rid of my pet if I’m pregnant?
No. You don’t need to give up your cat or dog. But you should avoid cleaning the litter box yourself-Toxoplasma gondii, a parasite in cat feces, can harm a developing fetus. Have someone else handle it, or wear gloves and wash your hands thoroughly afterward. Also, avoid handling stray animals and raw meat during pregnancy.
Can you get rabies from a squirrel or rabbit?
It’s extremely rare. Rabies is most commonly spread by bats, raccoons, skunks, foxes, and unvaccinated dogs. Small rodents like squirrels, hamsters, and rabbits almost never carry rabies. But if you’re bitten by any wild animal, wash the wound immediately and contact your doctor. Don’t assume it’s safe.
How do I know if an animal has a zoonotic disease?
You often can’t tell. Many infected animals show no symptoms. A healthy-looking dog can carry Salmonella. A cat with toxoplasmosis may act perfectly normal. That’s why prevention is based on behavior, not appearance. Always assume animals can carry germs and take precautions-wash hands, avoid bites, cook meat properly.
Are zoonotic diseases more dangerous than regular infections?
Some are. Rabies has a near 100% fatality rate once symptoms appear. Ebola kills up to 90% of untreated cases. Others, like salmonella, are usually mild but can be deadly for children or elderly people. The big difference is that zoonotic diseases often come from unexpected sources-your pet, your lunch, a tick bite-and doctors may not think to test for them right away, leading to delays in treatment.
Can you prevent zoonotic diseases with vaccines?
Only for a few. Rabies vaccines for pets and humans are highly effective. There’s also a vaccine for tick-borne encephalitis in Europe. But for most zoonotic diseases-like Lyme, salmonella, or toxoplasmosis-there are no human vaccines. Prevention relies on hygiene, food safety, and avoiding exposure. Vaccinating your pets is one of the most powerful tools you have.
Stephen Craig
January 4, 2026 AT 12:14It’s not the animals we should fear-it’s the illusion that we’re separate from them. We build walls, call them wildlife, then wonder why the walls crumble. The truth is, we’re just one species in a web of life that’s been whispering warnings for millennia. We just stopped listening.
Handwashing saves lives. Vaccinating pets isn’t optional-it’s basic reciprocity. We take their companionship; they deserve our responsibility.
One Health isn’t a buzzword. It’s the only sane way forward.
Connor Hale
January 4, 2026 AT 13:35I’ve lived with three dogs and two cats over the last 15 years. Never gotten sick. But I also never let them lick my face, wash my hands after scooping litter, and always cook my chicken to 170°F. It’s not complicated. Just consistent.
People act like this is some new threat. It’s not. We’ve always lived with germs. We just forgot how to respect them.
Roshan Aryal
January 5, 2026 AT 13:25Westerners love to panic about pets and ticks while ignoring the real source: China’s wet markets, India’s unregulated livestock, Africa’s bushmeat trade. You want to stop zoonotic spillover? Stop romanticizing nature and start enforcing borders on biological risk. No more ‘ecotourism’ that turns into a pathogen shuttle.
And stop blaming capitalism-it’s population density and poor sanitation in the Global South that’s the engine here. Not your damn organic kale.
Jack Wernet
January 6, 2026 AT 18:05Thank you for this comprehensive and well-researched piece. The integration of public health, veterinary medicine, and environmental stewardship is not merely advisable-it is imperative. The data presented underscores a systemic failure in interagency communication, particularly in the United States, where siloed governance undermines preparedness.
I would respectfully suggest that educational curricula in primary and secondary schools incorporate One Health principles as a foundational component. Early exposure cultivates lifelong awareness, which is more sustainable than reactive fear.
Additionally, policy reform must incentivize cross-sector data sharing. Without it, we remain blind to the earliest signals of the next outbreak.
Catherine HARDY
January 7, 2026 AT 16:43They’re not just talking about rabies and ticks. They’re hiding the real agenda. The CDC and WHO are pushing One Health because they want to track your pets, your food, your water-even your DNA. They’ve been building this surveillance net since 2015 under the guise of ‘safety.’
Remember when they said ‘flatten the curve’? Now it’s ‘vaccinate your dog’ and ‘avoid reptiles.’ Next thing you know, they’ll mandate microchips in cats and scan your hands before you enter a grocery store.
Don’t let them normalize this. This isn’t prevention. It’s control.
Vicki Yuan
January 8, 2026 AT 23:17This is exactly the kind of information we need to stop treating zoonotic diseases like scary myths and start treating them like preventable risks-like car accidents or food poisoning.
My nephew got salmonella from his pet turtle last year. He was in the hospital for five days. His parents didn’t even know turtles could carry it.
Let’s stop acting like ‘it won’t happen to me’ and start acting like responsible humans. Wash your hands. Cook your meat. Get your pets vaccinated. It’s not hard. It’s just inconvenient.
And if you’re pregnant-yes, someone else should clean the litter box. No, your cat isn’t judging you. The parasite is.
Uzoamaka Nwankpa
January 10, 2026 AT 02:44I read this and cried. Not because I’m scared, but because I feel so alone in this. Everyone I know thinks pets are just cute toys. My dog licked my face after eating raw chicken and I screamed at him-my husband said I was overreacting.
He doesn’t understand. I’ve seen what happens when people ignore this. My cousin in Lagos died from brucellosis. They thought it was just the flu. No one tested for it. No one cared.
It’s not about fear. It’s about love. Love for the animals. Love for the people. Love for the future.
Please. Just wash your hands.
Chris Cantey
January 10, 2026 AT 13:39There’s a deeper truth here that no one wants to admit: we’ve been living in a fantasy of control. We think we’re the apex species, that we’ve tamed nature. But every time a virus jumps from a bat to a human, nature reminds us we’re still just meat in a world full of other meat.
Our arrogance is the real zoonosis.
And vaccines? They’re just Band-Aids on a hemorrhage. Until we stop eating the forests and selling the wild like souvenirs, this cycle won’t end.
We’re not the heroes here. We’re the virus.
Abhishek Mondal
January 11, 2026 AT 02:18Let us not conflate correlation with causation: the claim that ‘75% of emerging diseases originate in animals’ is statistically misleading, as it conflates zoonotic origin with zoonotic transmission-two entirely distinct phenomena. Moreover, the WHO’s own 2020 report notes that anthropogenic land-use change is the proximate cause, not the animal itself.
Furthermore, the assertion that ‘washing hands reduces transmission by 90%’ is derived from a single, non-peer-reviewed CDC internal memo from 2018-its methodology was flawed, with no control for confounding variables such as socioeconomic status or access to clean water.
One must question the epistemic authority of the entire narrative. Is this science-or is it performative public health theater?
Oluwapelumi Yakubu
January 11, 2026 AT 16:34Bro, this post is fire. Real talk-I’m from Nigeria, and we’ve been dealing with this since our grandmas used to boil milk over open fire because ‘it kills the bad spirits.’ Now we got fancy terms like ‘One Health’ and ‘zoonotic spillover,’ but the truth? It’s the same old game.
My uncle got sick from eating raw goat meat during a wedding. He was fine, but his cousin didn’t make it. No one tested for brucellosis. Just said ‘he ate too much.’
So yeah-wash your hands. Don’t kiss your dog. Cook your meat. And if someone tells you ‘it’s organic, so it’s safe’? Laugh in their face.
We ain’t got time for fancy labels. Just keep it clean.
Akshaya Gandra _ Student - EastCaryMS
January 13, 2026 AT 01:36wait so if i have a pet hamster and i wash my hands after holding it im fine right? also i think the part about not kissing pets is kinda mean?? like my cat licks me and its so cute?? also is it bad if i eat raw chicken if i like it rare??