Why Generic Combination Products Improve Patient Compliance
 Jan, 11 2026
Jan, 11 2026
When you’re managing a chronic condition like diabetes, high blood pressure, or COPD, taking your meds isn’t just about popping pills. It’s about remembering when, how, and why - and doing it every single day. That’s where generic combination products make a real difference. These are single products that combine two or more active ingredients - or a drug with a delivery device - into one easy-to-use package. And because they’re generic, they cost far less than the brand-name versions. But here’s the kicker: they don’t just save money. They actually help people stick to their treatment plans.
How Combination Products Simplify Treatment
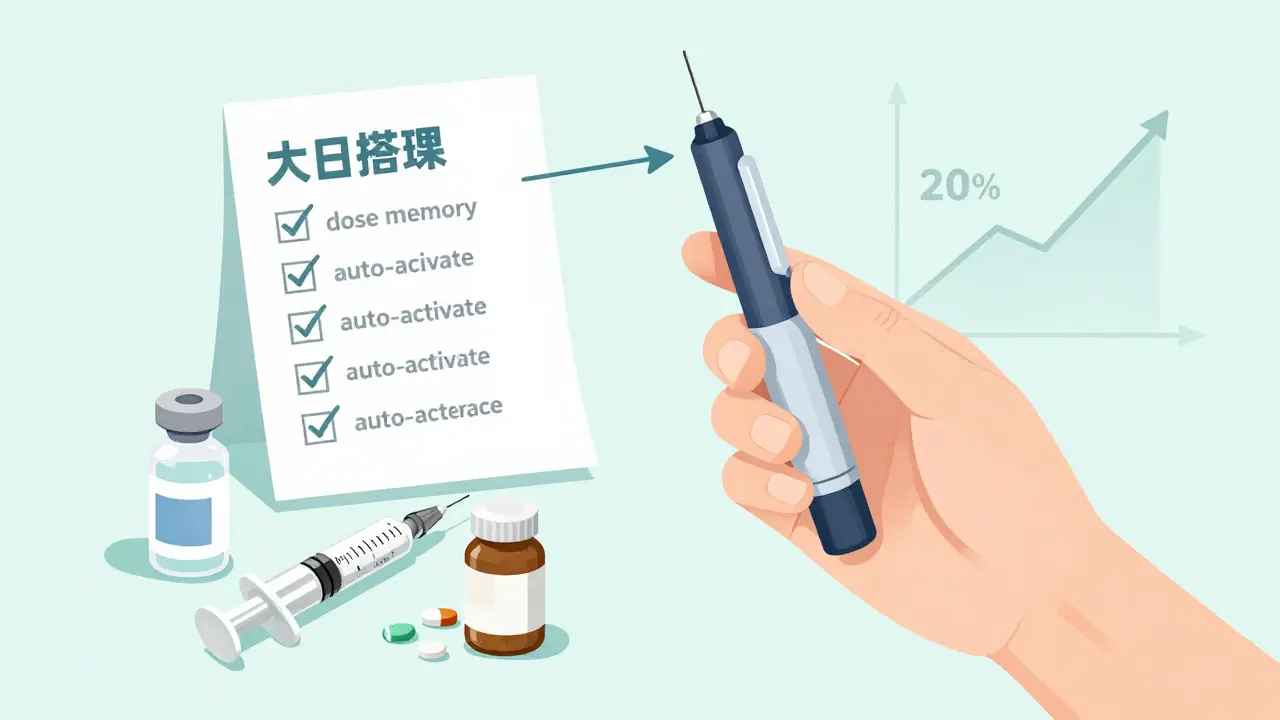
Think about a typical patient with type 2 diabetes. A few years ago, they might have been handed three separate items: insulin vials, syringes, and oral metformin tablets. Each had its own schedule, storage rules, and preparation steps. Mixing them up was easy. Forgetting one was common. Now, many patients use prefilled insulin pens that combine the drug and delivery system in one unit. Some even come with built-in dose memory. These are combination products - and their generic versions are now widely available. The math is simple: fewer steps mean fewer mistakes. Studies show that when patients switch from multiple separate medications to a single combination product, adherence improves by 15% to 25%. Why? Because the brain doesn’t have to juggle five different routines. It handles one. That’s why 62% of doctors say they prefer combination products for chronic conditions - if they’re available.Why Generic Versions Work Just as Well
Generic combination products aren’t cheap knockoffs. They’re FDA-approved equivalents of brand-name products. That means they contain the exact same active ingredients, delivered in the same way, at the same strength. The device part - whether it’s a pen, patch, inhaler, or auto-injector - must perform identically. For example, a generic insulin pen must deliver doses within 5% of the labeled amount. The force needed to activate it? Same as the brand. The failure rate? Less than 0.1% in testing. The drug component is tested for bioequivalence: its absorption into the bloodstream must fall within 80-125% of the brand’s rate. That’s tight. And the device? It has to pass the same reliability tests. No shortcuts. So when a patient gets a generic version, they’re not getting less medicine or a flimsy device. They’re getting the same treatment - at 30% to 80% lower cost.Cost Is a Huge Barrier - and Generics Break It
Money matters. A lot. The FDA found that 23.4% of patients skip doses because they can’t afford their meds. That’s more than one in five. For someone on insulin, that’s not just inconvenient - it’s dangerous. A generic combination product can cut monthly costs from $300 to $60. That’s not a small difference. It’s the difference between taking your medicine and not. And here’s something surprising: patients who start on generic drugs are 8.7 percentage points more likely to stick with them long-term than those who start on brand-name versions. Why? Because when the cost is low, the guilt of skipping doses fades. People feel less trapped. They’re more willing to try, to keep going, to believe the treatment will work.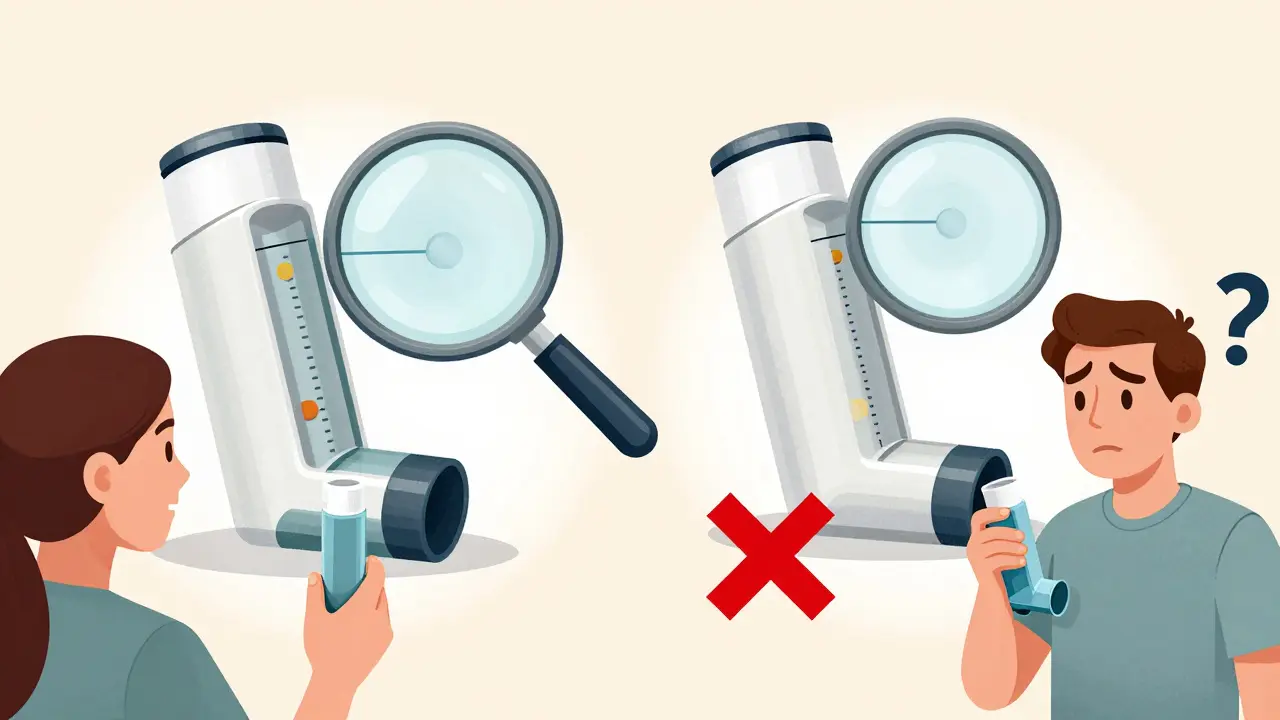
Real People, Real Results
On Reddit’s r/Diabetes forum, users share stories like this: “I used to spend 15 minutes every morning preparing insulin with syringes. I’d get distracted, spill it, forget the needle. Switching to a generic prefilled pen? I go from zero errors to almost none.” Another wrote: “I used to skip doses when my co-pay was $75. Now it’s $12. I take it every day.” These aren’t outliers. A survey by Oliver Healthcare Packaging found that 78% of patients using combination products said the ease of use led to better adherence - especially those managing long-term illnesses. When you don’t have to think about how to use it, you’re more likely to just do it.The Hidden Problem: Switching Between Generics
Here’s the catch. Not all generic combination products are identical. The drug is the same, but the device might look or feel different. One generic inhaler might require a slow, deep breath. Another might need a quick, sharp puff. If a patient gets switched from one generic to another without warning - and without training - they might mess up the technique. And then they’ll think the medicine isn’t working. A COPD patient on PatientsLikeMe said: “I got three different generic inhalers in one year. Each one felt different. I missed doses because I didn’t know how to use the new one.” That’s not the fault of the generic product. It’s a gap in how pharmacies and providers handle substitutions. Studies show that 32% of patients who switch between generic versions of combination products experience confusion that leads to missed doses. The fix? Better communication. Pharmacists need to explain the difference. Doctors need to remind patients. Clear, visual instructions - like diagrams on the box or QR codes linking to demo videos - help a lot.What Doctors and Pharmacists Can Do
The best thing you can do for a patient on a generic combination product? Talk to them. Not just about the drug. About the device. Ask: “Do you know how to use this?” “Does it feel different from last time?” “Do you have any trouble with the button or the spray?” Training time varies. A nicotine patch? Five minutes. An auto-injector? Up to 30 minutes. But that investment pays off. FDA experts say proper counseling can boost adherence by 17% to 22%. That’s more than the benefit of the combination product itself. Also, don’t assume patients know what “generic” means. Many still think it means “weaker.” Tell them: “This has the same active ingredient. The device works the same way. The only difference is the price.”What’s Next for Generic Combination Products
The market is growing fast. In 2022, the global combination product market hit $127.5 billion. By 2030, it’s expected to nearly double - to $258.3 billion. Diabetes, heart disease, and asthma are the top drivers. And with the Inflation Reduction Act pushing for lower drug prices, more generics are coming. Newer versions are getting smarter. Some now include Bluetooth chips that track when the device is used. Others have dose counters that sync with phone apps. These features are being built into generic versions too - making adherence even easier. The FDA is working on new guidelines to make sure generic combination products are more consistent. The goal? Reduce confusion when patients switch between brands. That’s going to take a few years. But progress is happening.Bottom Line: Better Adherence, Lower Cost, Same Results
Generic combination products aren’t a compromise. They’re an upgrade. They cut costs. They cut complexity. They cut the chances of missing a dose. For patients with chronic conditions, that’s life-changing. You don’t need to choose between affordability and effectiveness. With these products, you get both. The key is making sure patients understand how to use them - and that they’re not switched around without support. If you’re managing a long-term illness, ask your doctor or pharmacist: “Is there a generic combination product for my treatment?” If you’re a provider, don’t just prescribe it. Explain it. Train them. Follow up. Because when compliance improves, hospital visits drop. Complications slow. Lives get better.Are generic combination products as effective as brand-name ones?
Yes. Generic combination products must meet the same FDA standards as brand-name versions. The active drug must be bioequivalent, meaning it works the same way in the body. The delivery device - like a pen, inhaler, or patch - must perform identically in tests for dose accuracy, activation force, and reliability. The only difference is cost.
Why do some patients have trouble with generic combination products?
The issue isn’t the drug - it’s the device. Different generic versions may use slightly different designs for the same product. For example, one generic inhaler might require a slow breath, while another needs a quick puff. If a patient switches between them without training, they may use it wrong and miss doses. That’s why clear instructions and patient counseling are critical.
Do generic combination products cost less than separate medications?
Yes, and significantly. A generic combination product often costs 30% to 80% less than buying the same drugs separately - even if those drugs are generic. Plus, you avoid the extra cost of multiple devices (like syringes, inhalers, or patches). For patients on long-term therapy, this can mean hundreds of dollars saved each year.
Which conditions benefit most from combination products?
Chronic conditions that require daily, long-term treatment see the biggest gains. These include diabetes (insulin pens), high blood pressure (ACE inhibitor + diuretic combos), COPD and asthma (inhaled corticosteroids + bronchodilators), and cardiovascular disease (drug-eluting stents). These products simplify complex regimens and reduce the chance of missed doses.
How can I tell if my medication is a combination product?
Look at the name. Many combination products have names that include two drug names, like "Lisinopril/HCTZ" or "Fluticasone/Salmeterol." If it comes with a device - like a pen, inhaler, or patch - and contains more than one active ingredient, it’s a combination product. Ask your pharmacist to confirm. They can also tell you if a generic version is available.
Can I switch between different generic versions of the same product?
You can, but you shouldn’t without checking. Different generic versions may have different device designs, even if the drug is the same. Switching without training can lead to misuse and missed doses. Always ask your pharmacist if the new version is the same as the last one. If it looks or feels different, request a quick demonstration.
Cassie Widders
January 12, 2026 AT 17:25Been on a combo inhaler for COPD for three years. Cheaper, easier, and I actually remember to use it. No drama.
laura manning
January 13, 2026 AT 13:41While the data presented is statistically significant, one must consider the confounding variables inherent in self-reported adherence metrics. The 15–25% improvement cited lacks adjustment for socioeconomic covariates, and the FDA’s bioequivalence thresholds-while nominally rigorous-do not account for inter-patient pharmacokinetic variability. Furthermore, the assertion that device homogeneity ensures therapeutic equivalence is empirically unsound; mechanical tolerances in generic delivery systems exhibit a 3–7% variance in actuation force, which may impact pulmonary deposition in elderly or arthritic patients. The conclusion that generics are universally superior is therefore premature, and requires longitudinal, double-blind, randomized control trials with biomarker validation.
Bryan Wolfe
January 14, 2026 AT 16:42This is so needed! I’ve seen friends give up on their meds because they couldn’t afford it-then end up in the ER. Switching to a combo generic? Life-changing. One guy I know went from $280/month to $45-and now he’s hiking again. No magic, just smart design and fair pricing. We need more of this, not less. Seriously, if your doc doesn’t mention it, ask. It’s not just about saving money-it’s about saving your future.
Sumit Sharma
January 15, 2026 AT 07:37The entire premise is flawed. Generic combination products are not equivalent. The FDA’s 80–125% bioequivalence window is a regulatory loophole, not a clinical guarantee. In India, where I practice, we see 18% failure rates in generic insulin pens due to substandard polymer seals in the cartridge housing. The device is not the drug. The device is the delivery mechanism. If the plunger resistance differs by 0.3N, you get underdosing. And patients? They don’t know. They just stop taking it. This is not progress-it’s pharmaceutical negligence masked as affordability. We need stricter device performance standards, not more generics.
Jay Powers
January 15, 2026 AT 21:07I love how this breaks it down. I used to think generic meant weak. Then my doc switched me to a combo pill for blood pressure and told me flat out: same active ingredients, same results, way cheaper. I didn’t even notice a difference. The only thing that changed? I stopped skipping doses because I wasn’t terrified of the bill. People need to hear this. Not just patients. Providers too. Just say it plain: it’s not a downgrade. It’s a upgrade with a better price tag.
Lawrence Jung
January 17, 2026 AT 07:46Let’s be real-this is just capitalism dressed up as compassion. You don’t care about patients. You care about profit margins. The system rewards cutting corners under the banner of ‘affordability.’ The real solution? Universal healthcare. Not cheaper pills that shift the burden onto confused, overworked patients who can’t tell the difference between a pen and an inhaler. This isn’t innovation. It’s exploitation dressed in a white coat.
Alice Elanora Shepherd
January 17, 2026 AT 17:27Thank you for highlighting the device variability issue. I’ve seen this firsthand: a patient switches from one generic inhaler to another, and suddenly her symptoms worsen. She blames the medication. We blame her. The truth? The nozzle’s spray pattern changed. The puff volume is different. A 3-minute demo with a trainer inhaler, and she’s back on track. Simple. Cheap. Effective. Why isn’t this standard practice? Pharmacists are overworked, yes-but a QR code on the box linking to a 90-second video? That’s not asking much. It’s basic patient safety.
Christina Widodo
January 17, 2026 AT 20:46Wait-so if I’m on a combo product and my pharmacy switches me to a different generic, do I need to go back to my doctor every time? Or can I just ask the pharmacist? Also, what if I can’t afford the demo time? Is there a free app or something? I’m asking because my mom’s on one of these and she’s scared she’s doing it wrong. She doesn’t trust herself to figure it out.
Rinky Tandon
January 19, 2026 AT 13:20OMG I’m so glad someone finally said this! I was on a generic combo for asthma and got switched to another one and I thought I was dying! My chest felt like it was closing and I panicked. Turns out? The new one required a different breath pattern. I didn’t know! No one told me! I cried for three days thinking I was dying. This is a PUBLIC HEALTH CRISIS. People are dying because no one explains the damn device. And now they’re making it worse by swapping generics like they’re trading socks. I’m not mad-I’m FURIOUS.
Eileen Reilly
January 20, 2026 AT 17:58generic combo products are lit fr fr. i used to forget 3 pills a day now i just take one and boom im good. cost dropped from 200 to 30. no cap. my dr didnt even tell me about it i had to ask. yall need to be louder about this. also the pen thing? 10/10 no more needles. i miss the needles like i miss my ex
Rebekah Cobbson
January 22, 2026 AT 09:46Just wanted to say thank you for writing this. My husband has type 2 and we were drowning in bills. When we switched to the generic combo pen, it was like a weight lifted. He started checking his sugars again. He’s sleeping better. He’s laughing again. It’s not just about the medicine-it’s about dignity. You don’t feel like a burden when you can afford to take care of yourself. If you’re a provider reading this: don’t assume they know. Show them. Let them hold it. Let them click it. That five minutes? It’s worth more than any script.