When to Avoid a Medication Family After a Severe Drug Reaction
 Dec, 23 2025
Dec, 23 2025
When you’ve had a bad reaction to a drug, it’s natural to want to avoid anything like it ever again. But not all reactions mean you need to avoid an entire class of medications. Many people are told to steer clear of penicillin, sulfa drugs, or NSAIDs after a single bad experience-only to find out years later they could’ve taken them safely. The truth is, severe drug reaction doesn’t always mean lifelong avoidance. Knowing when to draw the line-and when to question it-can keep you safe and get you the right treatment when you need it.
What Counts as a Severe Drug Reaction?
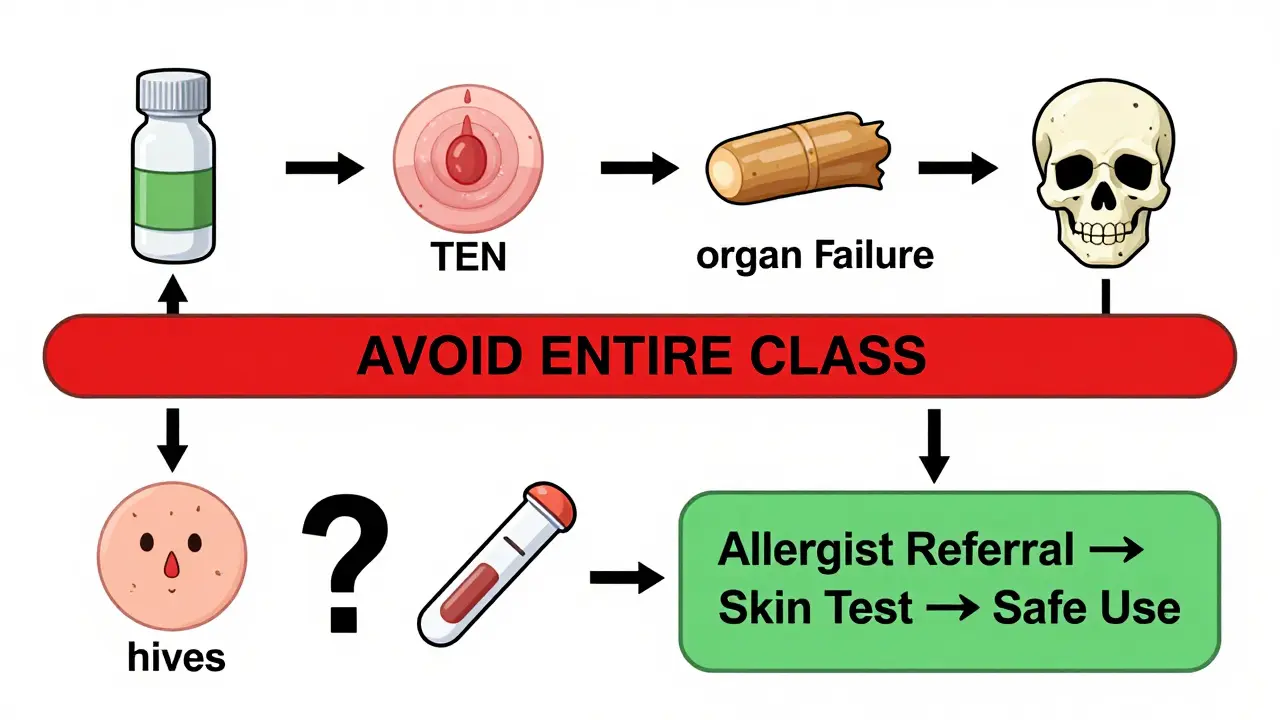
A severe drug reaction isn’t just a rash or an upset stomach. The FDA defines it as something that’s life-threatening, requires hospitalization, causes permanent disability, or leads to a birth defect. These are the reactions that demand serious attention. Common examples include anaphylaxis (a full-body allergic shock), Stevens-Johnson syndrome (SJS), toxic epidermal necrolysis (TEN), and DRESS syndrome (drug reaction with eosinophilia and systemic symptoms). These aren’t just uncomfortable-they can be deadly. TEN, for instance, kills 30% to 50% of people who get it.Most drug reactions aren’t this bad. About 80-90% of reported reactions are predictable side effects-like nausea from antibiotics or dizziness from blood pressure meds. These don’t usually mean you need to avoid the whole family. But if you break out in hives, your throat swells, your skin peels off, or you develop a high fever with organ damage, that’s a different story. Those are signs your immune system went rogue, and that’s where avoiding the entire drug class often becomes necessary.
Not All Reactions Are Allergies
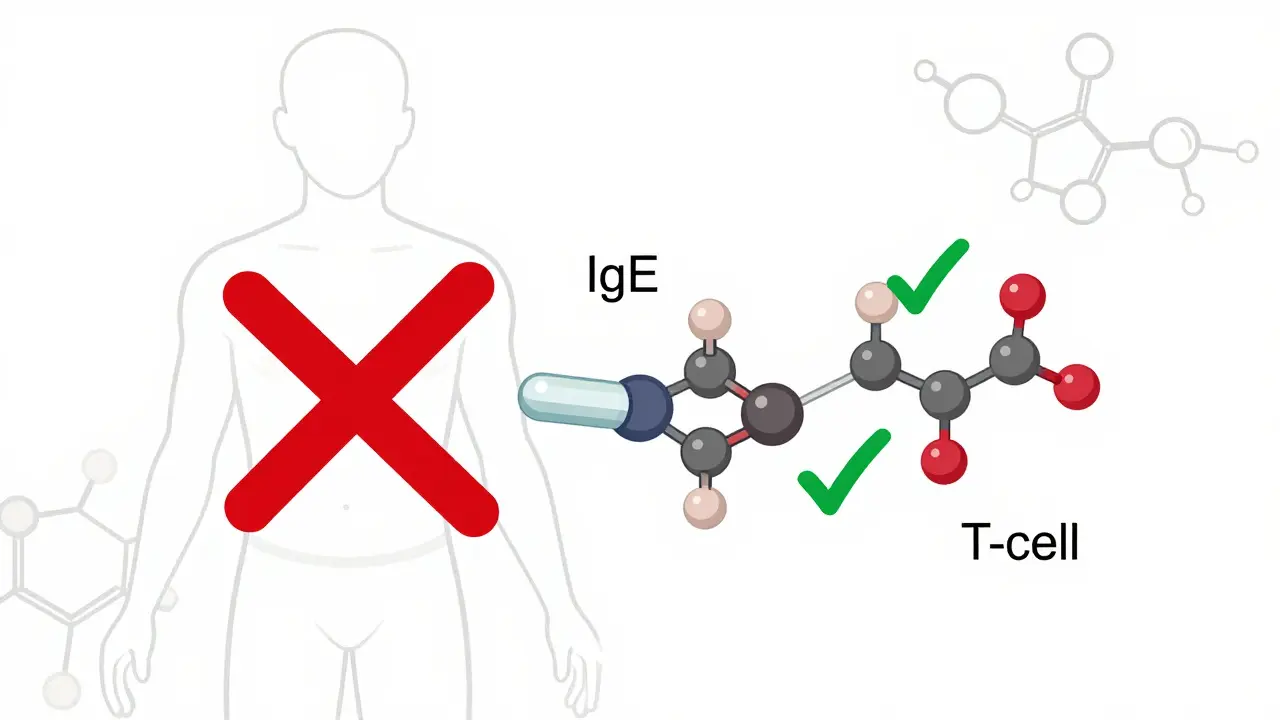
A lot of people think they’re allergic to penicillin because they got a rash as a kid. But in reality, only about 10% of people with that label actually have a true IgE-mediated allergy. Most of those rashes are non-allergic, caused by the virus you had at the same time, not the antibiotic. Yet, once that label sticks in your medical record, doctors assume the worst and avoid all beta-lactam antibiotics-penicillins, cephalosporins, even carbapenems.That’s a problem. A 2020 study from Harvard found that 95% of patients labeled with penicillin allergy could tolerate it after proper testing. Avoiding these drugs unnecessarily means you get stronger, broader-spectrum antibiotics instead-ones that cost more, disrupt your gut microbiome, and increase the risk of resistant infections like C. diff. The same goes for sulfa drugs. A reaction to Bactrim (sulfamethoxazole-trimethoprim) doesn’t mean you can’t take sulfa-based diuretics or diabetes meds. The cross-reactivity risk between sulfa antibiotics and other sulfa drugs is only about 10%.
When Avoidance Is Non-Negotiable
There are times when avoiding an entire class isn’t just smart-it’s life-saving. If you’ve had SJS, TEN, or DRESS after taking a drug, you almost certainly need to avoid the entire family. These reactions are immune-mediated and can happen again, even with tiny doses. The European Medicines Agency found that 95% of TEN cases are caused by just six drug classes: sulfa antibiotics, anticonvulsants like carbamazepine, allopurinol, NSAIDs, nevirapine, and corticosteroids.For example, if you had TEN after taking carbamazepine, you should never take another anticonvulsant in the same class-oxcarbazepine, phenytoin, lamotrigine-because they share similar chemical structures. The same goes for allopurinol. If you developed DRESS after taking it, avoid all xanthine oxidase inhibitors. There’s no safe gray area here. These reactions are unpredictable, rare, and deadly. Once you’ve been through one, you’re at much higher risk for another.
Cross-Reactivity: The Real Risk
Cross-reactivity means your body reacts to more than one drug because they’re chemically similar. But it’s not automatic. The risk varies wildly by drug family.With beta-lactam antibiotics (penicillins, cephalosporins), cross-reactivity is often overstated. If you’re allergic to amoxicillin, your risk of reacting to cefdinir is only about 2%. But if you reacted to ampicillin, the risk with ceftriaxone might be closer to 5%. The key is the side chain-the part of the molecule that sticks out. If two drugs have the same side chain, the risk jumps. That’s why some allergists test for specific components now, not just the whole class.
NSAIDs are another tricky area. If you have aspirin-exacerbated respiratory disease (AERD), you’re likely to react to nearly all traditional NSAIDs-ibuprofen, naproxen, diclofenac-because they block the same enzyme. That’s a 70% cross-reactivity rate. But COX-2 inhibitors like celecoxib don’t trigger this reaction in most cases. So, avoidance isn’t always total.
Statins are a good example of when avoidance isn’t needed. If you got muscle pain from atorvastatin, you might still tolerate rosuvastatin or pravastatin. Cross-reactivity is only 10-15%. The same goes for SSRIs-if one made you nauseous, another might not.
What You Should Do After a Severe Reaction
If you’ve had a serious reaction, here’s what to do next:- Get the details written down. What drug? When did symptoms start? What happened? Did you need epinephrine? Were you hospitalized? Vague notes like “allergic to penicillin” aren’t enough.
- Ask for a referral to an allergist. They can do skin tests or blood tests to confirm if it’s a true IgE-mediated allergy. For drugs like penicillin, these tests are highly accurate.
- Consider a drug challenge. If your reaction was mild and you need the drug, an allergist can give you a tiny dose under supervision to see if you react. Success rates are 70-85% for beta-lactams in low-risk cases.
- Update your medical records. Make sure your EHR has the exact reaction, not just a blanket label. Use terms like “anaphylaxis to amoxicillin” instead of “penicillin allergy.”
- Carry medical ID. If you’ve had anaphylaxis or SCARs, wear a bracelet or carry a card. Emergency rooms need to know immediately.
Why So Many People Are Avoiding Drugs They Can Tolerate
The problem isn’t just medical-it’s systemic. A 2021 study found that only 28% of electronic health records had enough detail to guide safe prescribing. Most entries just say “allergic to penicillin,” with no symptoms, no timeline, no severity. That leads to overcautious prescribing.Hospitals have automated alerts that block certain drugs if there’s any allergy in the record. In one trial, doctors overrode these alerts 23% of the time because they knew the label was wrong. But that’s risky. The NIH’s Preventing Overrides initiative cut those unsafe overrides by 37% by requiring doctors to explain why they were overriding the alert. That’s progress-but it’s not everywhere.
Patients, too, are scared. A survey by the Asthma and Allergy Foundation found that 42% of people with drug allergy labels had delays in treatment-on average, 3.2 days. One man in a Reddit thread said he waited a week for a UTI antibiotic because doctors refused to give him anything after his “sulfa allergy.” He ended up in the ER with sepsis.
What’s Changing in Drug Safety
The field is shifting toward precision. In 2022, the FDA approved a new test called ImmunoCap Specific IgE that can detect true drug allergies with 89% accuracy-up from 60% with old skin tests. Genetic testing is also helping. The HLA-B*57:01 gene test for abacavir (an HIV drug) is now standard. If you don’t have the gene, you can take it safely. No more unnecessary avoidance.AI tools are starting to help too. A 2022 Mayo Clinic trial used IBM Watson to analyze patient histories and found that 41% of drug avoidance recommendations were unnecessary. The system flagged cases where patients were labeled allergic based on mild rashes or viral infections.
And de-labeling is gaining traction. Eighty-seven percent of academic medical centers now have formal penicillin allergy assessment programs. That means more people are getting tested, more are finding out they’re not allergic, and more are getting the best, safest treatment.
Bottom Line: Don’t Assume-Ask
If you’ve had a severe reaction, take it seriously. But don’t let a label define your future care. Many people avoid entire drug families for decades based on a childhood rash or a vague doctor’s note. That’s not just inconvenient-it’s dangerous. You might be denied the most effective, safest, or cheapest option because of misinformation.Ask your doctor: Was this a true allergy? Do I need to avoid the whole class? Can I be tested? Is there a safer alternative? If your provider doesn’t know, ask for a referral to an allergist. Your next prescription could depend on it.
Do I have to avoid all antibiotics if I’m allergic to penicillin?
No. Only about 10% of people labeled with penicillin allergy have a true IgE-mediated reaction. Many can safely take cephalosporins or carbapenems, especially if the reaction was a mild rash. Skin testing or a supervised drug challenge can confirm whether you’re truly allergic. Avoiding all antibiotics unnecessarily increases your risk of resistant infections.
Can I take sulfa drugs if I had a reaction to Bactrim?
It depends. If you had a true allergic reaction-like hives, swelling, or anaphylaxis-avoid all sulfonamide antibiotics. But if you only had a rash or stomach upset, you may still safely take non-antibiotic sulfa drugs like furosemide (a diuretic) or sulfonylureas (for diabetes). Cross-reactivity between antibiotic and non-antibiotic sulfa drugs is only about 10%.
What’s the difference between a side effect and an allergic reaction?
A side effect is predictable and not immune-related-like nausea from antibiotics or dizziness from blood pressure meds. An allergic reaction involves your immune system and usually includes hives, swelling, trouble breathing, or anaphylaxis. Side effects can often be managed by switching drugs within the same class. Allergic reactions, especially severe ones, usually require avoiding the entire family.
Are drug allergy tests reliable?
For some drugs, yes. Skin tests and blood tests for penicillin are 90% accurate. For others, like NSAIDs or sulfa drugs, testing is less reliable. In those cases, a supervised drug challenge-where you’re given a small dose under medical watch-is the gold standard. It’s safe and helps confirm whether you truly react.
Can I outgrow a drug allergy?
Yes, especially with penicillin. About 80% of people who had a penicillin allergy in childhood lose it within 10 years. That’s why retesting is so important. If you were labeled allergic as a kid, you may be able to take it safely now. Don’t assume the label still applies.
What should I do if I had Stevens-Johnson syndrome from a drug?
Avoid the entire drug class permanently. SJS and TEN are life-threatening and can recur with even tiny amounts of the same drug or similar ones. If you had it from an anticonvulsant like carbamazepine, avoid all drugs in that class. Keep a medical alert bracelet and inform every provider you see. There’s no safe way to test for this reaction-it’s too dangerous.
Wilton Holliday
December 23, 2025 AT 20:27Been there. Got the rash at 12, labeled penicillin-allergic forever. Turned 30, went to an allergist, got tested-turned out I was fine. Took amoxicillin for a sinus infection last year like it was candy. No drama. Why do we still let childhood rashes dictate adult medicine? So many people are needlessly scared.
Also, if you’ve never had a drug challenge, you don’t know what you’re missing. It’s not scary if your doc knows what they’re doing. Just sayin’.
Raja P
December 24, 2025 AT 03:24Bro in India, we don’t even get tested. Doc says ‘sulfa bad’ and you get cipro even if you’re allergic to it. No choice. I had a rash from Bactrim, but my UTI came back worse. Took a sulfa diuretic last month for swelling-no problem. Maybe the system here is broken, but people just survive. No fancy tests. Just hope and pray.
Abby Polhill
December 25, 2025 AT 12:08Let’s talk about the HLA-B*57:01 genotype screening paradigm shift-this is the future. We’re moving from population-level avoidance to precision immunogenomics. The FDA’s recent validation of ImmunoCap Specific IgE assays has redefined diagnostic sensitivity for beta-lactams, reducing unnecessary avoidance by 40% in tertiary care settings.
Meanwhile, EHRs still default to ‘penicillin allergy’ as a blanket code because the UI doesn’t support granular phenotyping. It’s a systemic failure of clinical informatics, not patient ignorance. We need structured allergy documentation with SNOMED CT codes, not free-text blobs.
Bret Freeman
December 26, 2025 AT 11:56Oh my god. I can’t believe people are still getting away with this. You think a rash is ‘mild’? That’s your immune system screaming. You think you’re ‘fine’ after taking penicillin again? You’re playing Russian roulette with your organs. I had a cousin who got TEN from a sulfa drug. She lost 60% of her skin. Burned alive in a hospital bed for 3 months. Now she’s in a wheelchair.
Don’t be that person. Don’t be the one who says ‘I’m fine’ and then ends up in the ICU. This isn’t a game. You think you’re smart? You’re just lucky. And luck runs out.
Austin LeBlanc
December 27, 2025 AT 14:44Wait, so you’re telling me I should just trust some allergist who says ‘oh you’re not allergic’ after a poke and a drop? What if they’re wrong? What if they’re just trying to get rid of you? And what about all the lawsuits? Doctors are scared. They don’t want to be the one who lets someone die because they trusted a test.
Also, why do you think they call it a ‘drug allergy’? Because it’s an allergy. Not a ‘side effect.’ You don’t get to redefine medical terms because you don’t like the label. You think you’re helping? You’re putting lives at risk.
niharika hardikar
December 29, 2025 AT 12:13It is imperative to underscore that the misclassification of non-immunologic adverse drug reactions as allergic phenomena remains a pervasive issue in global clinical practice. The conflation of maculopapular rashes with IgE-mediated anaphylaxis is not merely a diagnostic error-it is a systemic failure in pharmacovigilance infrastructure.
Without mandatory allergist referral pathways and standardized electronic health record phenotyping, the prevalence of unnecessary drug avoidance will continue to contribute to antimicrobial resistance, increased healthcare expenditures, and preventable morbidity. The onus lies with regulatory bodies to enforce granular documentation protocols.
EMMANUEL EMEKAOGBOR
December 30, 2025 AT 15:50Respectfully, I must say that the approach described here is both scientifically sound and ethically necessary. In Nigeria, we face the opposite problem-patients are given drugs without any screening, and when reactions occur, they are buried under poverty and lack of access.
But for those who have access to testing, this is the way forward. I’ve seen patients avoid life-saving drugs for decades because of a single childhood rash. It breaks my heart. Testing should be made accessible, not a luxury. Let’s not let fear replace evidence.
Jillian Angus
January 1, 2026 AT 09:47I had a reaction to ibuprofen once. Swelling. Didn’t go to the doctor. Now I just take Tylenol. No big deal. Don’t need to test it. Just avoid it. Simple.
Also, I don’t trust doctors. They change their minds all the time. Why should I believe them now?
bharath vinay
January 2, 2026 AT 01:51Of course they’re lying. The pharmaceutical companies don’t want you to know that most ‘allergies’ are just side effects they engineered to sell you more expensive drugs. Penicillin? Cheap. Cephalosporins? Expensive. Carbapenems? Even more. They profit from fear. The whole ‘allergy’ thing is a scam to push you into their premium antibiotics.
And the ‘allergist’? Probably on their payroll. Why do you think they push testing? So you’ll pay for it. So they can sell you the next drug. Wake up. You’re being played.