Weight Loss Medications and Their Interactions with Blood Pressure Drugs and Antidepressants
 Jan, 30 2026
Jan, 30 2026
Weight Loss Medication Interaction Risk Calculator
Medication Selection
Results
Why Your Weight Loss Medication Might Be Lowering Your Blood Pressure Too Much
If you're taking a weight loss drug like Wegovy or Saxenda and also have high blood pressure, you might be surprised to find your blood pressure dropping too low. This isn’t rare-it’s common. Around 18% of people using GLP-1 medications like these end up with blood pressure readings below 90/60 mmHg, especially if they're already on meds like lisinopril or losartan. The problem? Your body is losing weight fast, your stomach is digesting food slower, and your blood vessels are relaxing-all of which naturally bring down blood pressure. But when you add that to antihypertensive drugs, the effect can become dangerous.
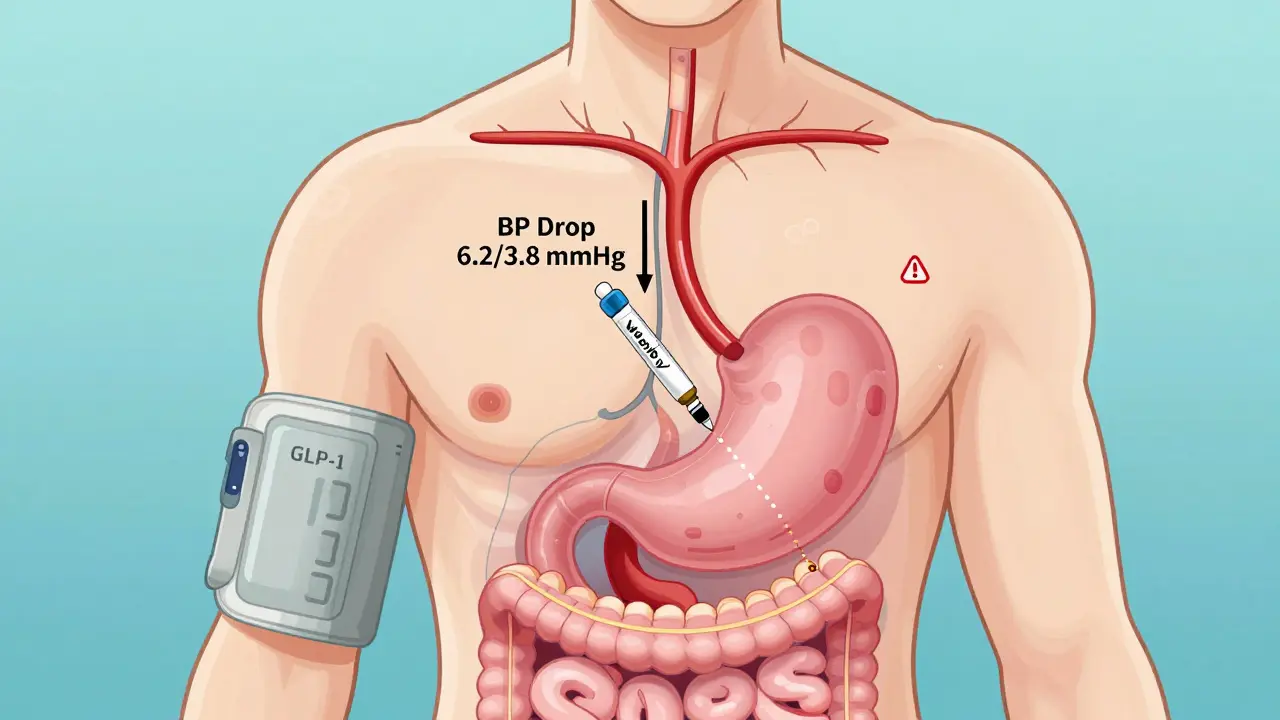
Take Wegovy (semaglutide), for example. Clinical trials showed it lowers systolic blood pressure by an average of 6.2 mmHg and diastolic by 3.8 mmHg-even in people who didn’t start out with high blood pressure. That’s not just a side effect; it’s a direct result of how the drug works. Saxenda (liraglutide) does the same, but less dramatically: about 4.1 mmHg systolic drop. Meanwhile, if you’re on ACE inhibitors or ARBs, the risk of low blood pressure jumps even higher because these drugs already reduce pressure, and GLP-1 medications amplify that effect. The American Association of Clinical Endocrinologists recommends cutting your blood pressure medication dose by 25-50% when you start these weight loss drugs. Many doctors don’t know this unless they specialize in obesity medicine.
What Happens When You Combine Phentermine with Blood Pressure Meds
Not all weight loss pills work the same way. Phentermine, an older stimulant approved in 1959, does the opposite of GLP-1 drugs. It raises blood pressure by triggering norepinephrine release-your body’s natural fight-or-flight signal. Studies show it can push systolic pressure up by 5-15 mmHg and diastolic by 3-10 mmHg. For someone already managing hypertension, this is risky. The CDC estimates 107 million U.S. adults have high blood pressure. Adding phentermine without adjusting other meds can push someone into dangerous territory.
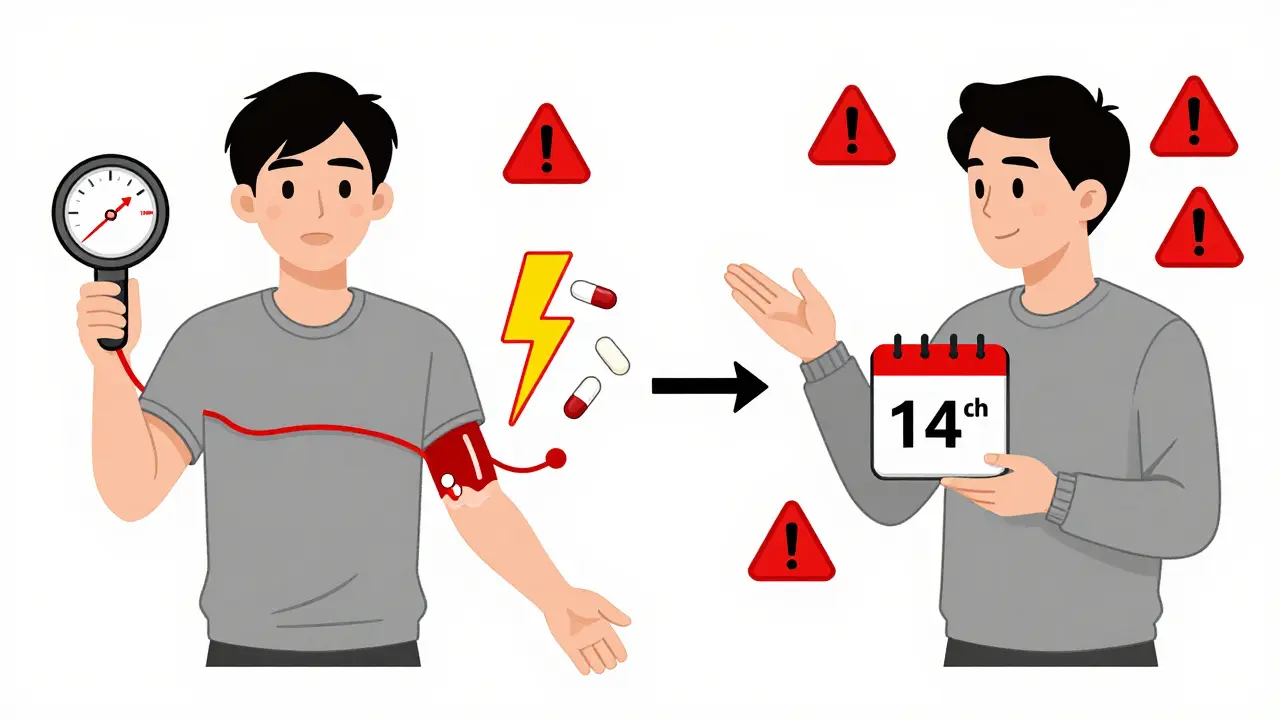
Even more alarming is the interaction between phentermine and MAOIs (monoamine oxidase inhibitors), a type of antidepressant. When taken together, they can cause a hypertensive crisis-blood pressure spikes over 180/120 mmHg, sometimes beyond 220/120. These aren’t theoretical risks. The FDA has documented emergency room visits from this combo. That’s why the FDA requires patients to stop MAOIs at least 14 days before starting phentermine. Many people don’t realize their antidepressant falls into this category, especially if they’ve been on it for years.
How GLP-1 Medications Affect Antidepressants Like Sertraline
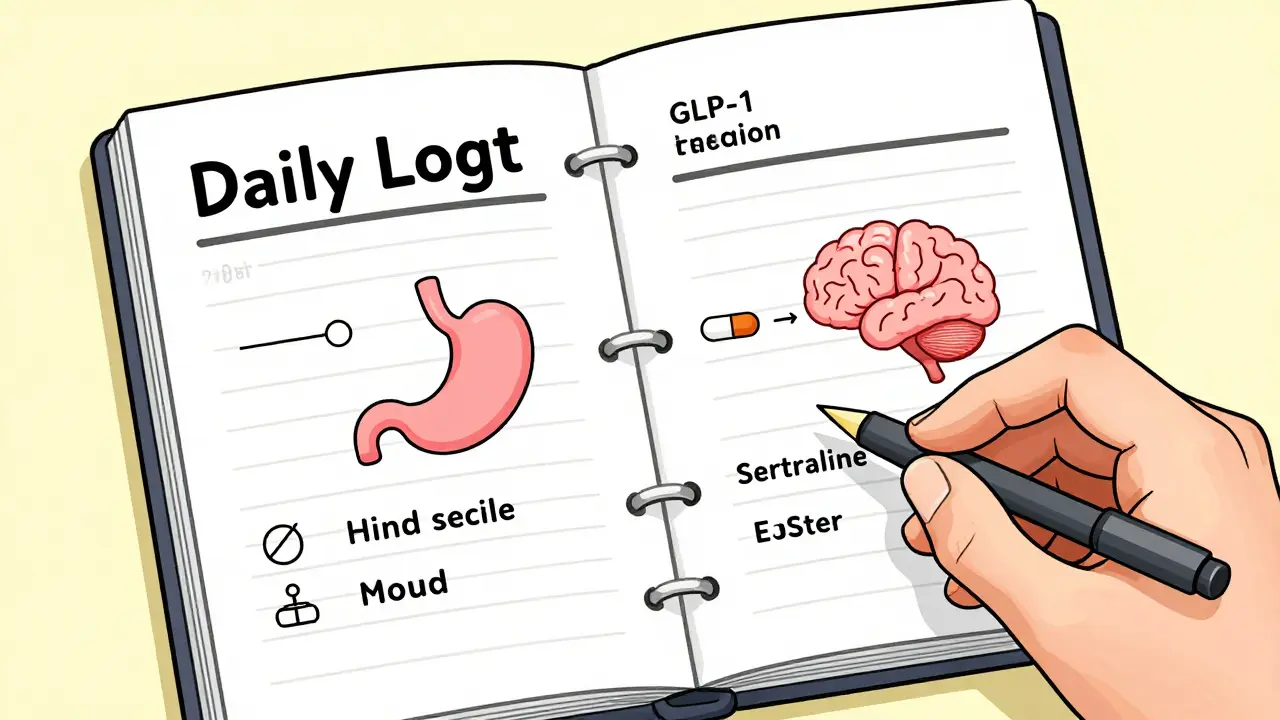
Another hidden issue: your antidepressant might not be working as well as it used to. GLP-1 medications like Wegovy and Saxenda slow down how fast your stomach empties-by 25-35%. That’s great for feeling full longer, but it messes with how your body absorbs pills taken by mouth. SSRIs like sertraline (Zoloft), fluoxetine (Prozac), and escitalopram (Lexapro) rely on consistent absorption. If your stomach delays emptying, the drug may not enter your bloodstream at the usual rate. A 2022 study found absorption of sertraline could drop by 18-25% in people taking liraglutide.
Patients have reported this in real life. On Reddit, someone wrote, “My sertraline stopped working after starting Saxenda.” Their psychiatrist confirmed delayed gastric emptying was likely the culprit. The American Psychiatric Association now recommends spacing out antidepressant doses from GLP-1 meds by at least two hours. Some psychiatrists are even checking blood levels of SSRIs in patients who report mood changes after starting weight loss drugs. If your anxiety or depression seems to be worsening, it’s not just in your head-it could be your medication timing.
Who’s at Highest Risk-and What to Watch For
Not everyone will have problems, but certain groups are more vulnerable. If you’re over 65, you’re at double the risk of dangerous drops in blood pressure. Studies show 22% of older adults on GLP-1 drugs and antihypertensives experience systolic pressure drops over 20 mmHg. That means dizziness, fainting, fatigue, or falls. The same group is also more likely to have kidney issues, which compounds the risk when GLP-1 drugs reduce kidney perfusion and raise potassium levels when combined with ACE inhibitors or ARBs.
People with type 2 diabetes are another high-risk group. GLP-1 medications improve blood sugar control, but when paired with sulfonylureas like glipizide or glimepiride, the risk of hypoglycemia spikes by 23-37%. That’s because the weight loss improves insulin sensitivity, and the diabetes meds are still dosed for the old, heavier body. The result? Low blood sugar symptoms-shaking, sweating, confusion-can hit hard and fast.
Watch for these signs: lightheadedness when standing, unusual fatigue, blurred vision, confusion, or heart palpitations. These aren’t normal side effects of losing weight-they’re red flags. If you’re on any combination of weight loss meds, blood pressure drugs, or antidepressants, keep a daily log of your symptoms and blood pressure readings. Bring it to your doctor.
How Doctors Are Managing These Interactions Today
Smart clinicians aren’t guessing anymore. They’re following clear protocols. Before starting any weight loss medication, they check your current blood pressure, kidney function, and all your medications. They ask: Are you on an ACE inhibitor? An ARB? A diuretic? An SSRI? An MAOI? If yes, they adjust. For GLP-1 users on blood pressure meds, most doctors reduce the dose by 25-50% upfront and recheck in one week. After that, they monitor monthly for three months, then every three months.
For antidepressants, the standard advice is to take them two hours before or after your GLP-1 shot. Some doctors switch patients from oral SSRIs to patches (like transdermal selegiline) or injections to bypass the gut entirely. If you’re on phentermine, your doctor should confirm you’ve been off MAOIs for at least two weeks. And if you’re taking Qsymia (phentermine-topiramate), they’ll know topiramate has its own blood pressure-lowering effect, so the net result is usually mild reduction-not dangerous spikes.
There’s also new tech helping. Novo Nordisk updated Wegovy’s prescribing guide in late 2023 to include specific warnings about hypotension. And by 2025, most electronic health records will auto-flag dangerous drug combos. Right now, though, it’s still up to you and your doctor to connect the dots.
What You Should Do Right Now
- Review all your meds with your doctor or pharmacist. Don’t assume your primary care provider knows about your weight loss drug unless you tell them.
- Check your blood pressure at home daily for the first month after starting any weight loss medication. Write it down.
- Track mood changes. If your antidepressant feels less effective, mention it. Don’t assume it’s just stress.
- Never stop or change doses on your own. Too many people lower their blood pressure meds because they feel better-only to crash later.
- Ask about alternatives. If you’re on phentermine and MAOIs, ask if there’s a safer weight loss option. If you’re on an SSRI and having side effects, ask about switching to a non-oral form.
The goal isn’t to scare you off weight loss meds. These drugs have helped millions lose weight, reverse prediabetes, and reduce heart disease risk. But they’re powerful. And like any powerful tool, they need careful handling. The key is communication-between you, your doctor, your pharmacist, and your mental health provider.
Frequently Asked Questions
Can I take Wegovy if I’m on lisinopril for high blood pressure?
Yes, but your dose of lisinopril will likely need to be lowered. Wegovy reduces blood pressure significantly, and combining it with lisinopril can cause your pressure to drop too low. Most doctors reduce the lisinopril dose by 25-50% when starting Wegovy and monitor blood pressure weekly for the first month. Symptoms like dizziness, fainting, or fatigue mean you need a dose adjustment.
Why did my Zoloft stop working after I started Saxenda?
Saxenda slows stomach emptying, which can delay or reduce how much sertraline (Zoloft) gets absorbed into your bloodstream. Studies show absorption can drop by 18-25%. If your depression or anxiety symptoms return, talk to your psychiatrist. They may recommend taking your antidepressant two hours before your Saxenda injection, switching to a different SSRI, or changing to a patch or injection form.
Is it safe to take phentermine with antidepressants?
Only if you’re not taking MAOIs. Phentermine combined with MAOIs can cause a life-threatening hypertensive crisis with blood pressure over 200/120 mmHg. If you’re on an MAOI like phenelzine or tranylcypromine, you must stop it at least 14 days before starting phentermine. For other antidepressants like SSRIs or SNRIs, the risk is lower, but your blood pressure should still be monitored closely.
How often should I check my blood pressure on weight loss meds?
Check it daily for the first month, especially if you’re on blood pressure meds. After that, check at least once a week for the next two months, then monthly. If you lose more than 10% of your body weight, your doctor should reassess all your medications. Many patients need to reduce their blood pressure meds after 15% weight loss.
Do GLP-1 medications interact with all blood pressure drugs the same way?
No. ACE inhibitors and ARBs increase the risk of low blood pressure and high potassium. Diuretics make the blood pressure-lowering effect stronger. Beta-blockers and calcium channel blockers have less interaction, but still require monitoring. The biggest danger is with ACE inhibitors and ARBs, especially in people with diabetes or kidney issues.
Sidhanth SY
January 31, 2026 AT 03:08Man, I started Wegovy last month and my BP dropped from 140/90 to 102/64 in two weeks. My doc didn’t warn me about the lisinopril interaction-had to google it myself. Now I’m on half my usual dose and not passing out when I stand up. Glad I didn’t just power through.
Adarsh Uttral
February 1, 2026 AT 20:38so i took saxenda and zoloft together and felt like a zombie for 3 weeks. my anxiety came back hard. turned out my body was barely absorbing the zoloft. switched to the patch and boom-back to normal. why dont more drs know this??
Sheila Garfield
February 2, 2026 AT 19:33I’m a nurse in London and I’ve seen this happen way too often. Patients come in dizzy, confused, thinking it’s ‘just aging’-but it’s the combo of GLP-1s and their BP meds. We now have a checklist we hand out with every new prescription. Simple stuff, but it saves lives. Just tell your doctor everything. Even the ‘tiny’ supplements.
Sarah Blevins
February 3, 2026 AT 06:52The data presented here is statistically significant but lacks longitudinal follow-up. The 18% hypotension rate cited is from a 12-week trial with a non-representative sample. Real-world adherence and polypharmacy are rarely accounted for in these studies. Further research is required before clinical protocols are standardized.