Thyroid Medications: Levothyroxine Safety and Monitoring
 Dec, 15 2025
Dec, 15 2025
Levothyroxine is one of the most commonly prescribed medications in the world. Millions of people take it every day to treat an underactive thyroid. It works. It’s reliable. But that doesn’t mean it’s risk-free. The real danger isn’t the drug itself-it’s what happens when it’s not managed right.
Why Levothyroxine Works (and When It Doesn’t)
Levothyroxine replaces the hormone your thyroid isn’t making enough of. When your thyroid slows down-whether from Hashimoto’s, surgery, radiation, or just aging-your body starts to feel it. Fatigue. Weight gain. Cold intolerance. Brain fog. Levothyroxine fixes that by giving your body the T4 hormone it’s missing. Most people feel better within weeks. Studies show about 90% of patients see their symptoms fade within 3 to 6 months of getting the dose right.
But here’s the catch: getting the dose right isn’t a one-time thing. It’s a process. Your body changes. Your metabolism slows with age. You gain or lose weight. You start or stop other meds. Even small shifts can throw your hormone levels off. That’s why monitoring isn’t optional. It’s the difference between feeling normal and feeling awful.
How Often Should You Get Tested?
Many patients go months-or even years-without a TSH test. That’s dangerous. The Specialist Pharmacy Service and the American Thyroid Association both say: test your TSH every 6 to 12 weeks after starting or changing your dose. Once you’re stable, test at least once a year. But if you’re over 65, pregnant, have heart disease, or take other medications like iron or antacids, you need more frequent checks.
Here’s what the data shows: in the UK, only 58% of primary care practices follow recommended monitoring schedules. That means nearly half of patients are flying blind. In one survey, 42% of patients said they hadn’t had a TSH test in over 18 months-even though they were still experiencing fatigue, weight gain, or anxiety. That’s not just negligence. It’s a systemic failure.
Don’t wait for symptoms to come back. Get tested. Even if you feel fine. TSH levels can drift silently. A level of 6.0 mIU/L might be "normal" on a lab report, but if your target is 2.5 (especially if you’re under 65), you’re under-treated. Your doctor should personalize your goal-not just rely on the lab’s "normal" range.
The Hidden Danger: Switching Brands
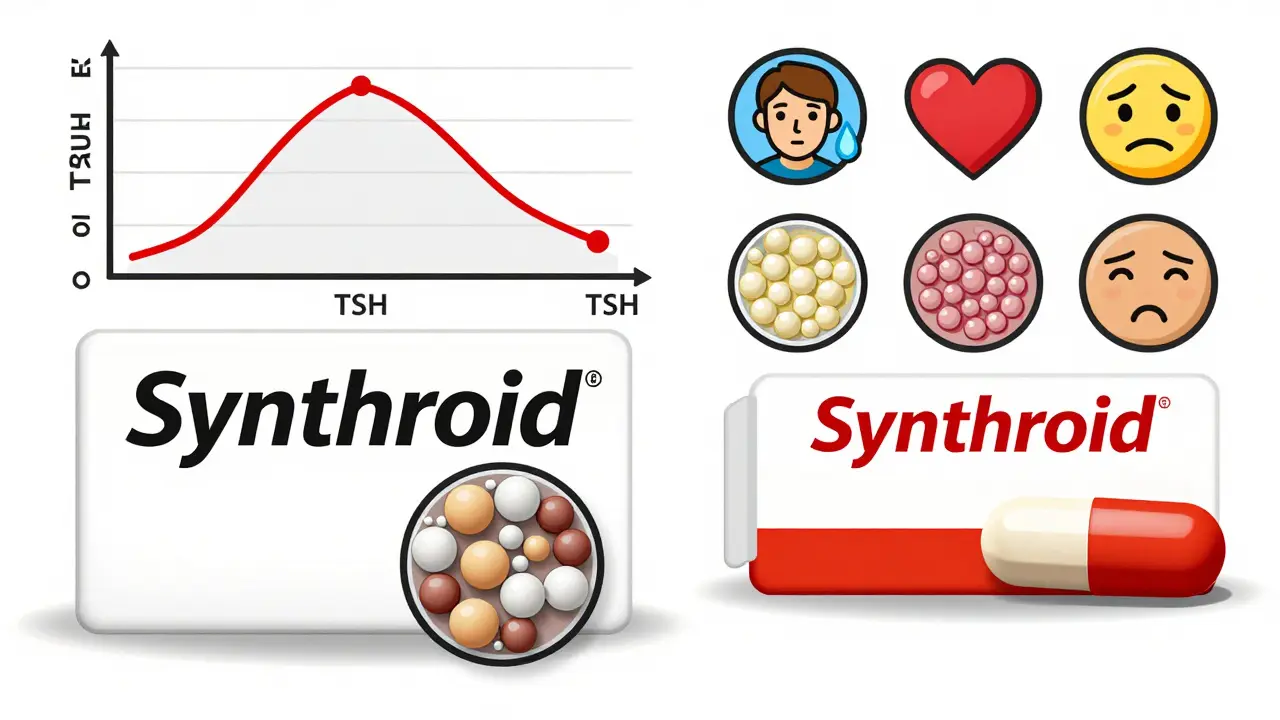
Here’s something most patients don’t know: not all levothyroxine is the same. Generic versions are chemically identical, but they’re not biologically identical. Small differences in fillers, coatings, and absorption rates can cause real symptoms.
The UK’s Medicines and Healthcare products Regulatory Agency (MHRA) reviewed over 300 reports between 2015 and 2019. In 78% of cases, people reported fatigue after switching brands. Others had headaches, palpitations, anxiety, or unexplained weight gain. And here’s the kicker: only 27 of those 335 cases included any thyroid blood tests. Doctors didn’t even check if the symptoms were thyroid-related.
On patient forums like Thyroid UK, 68% of 1,245 respondents said they had bad reactions after a pharmacy switched their prescription. One Reddit user wrote: "I was on Synthroid for 8 years. Switched to a generic. Within two weeks, my heart was racing. I couldn’t sleep. My doctor said, ‘It’s just stress.’ I went back to Synthroid-and I felt like myself again."
The FDA and EMA require generics to be within 90-110% of the brand’s potency. Sounds tight, right? But for a hormone with a narrow therapeutic window, that 20% variation can be enough to push you from euthyroid to hyper- or hypothyroid. If you’ve ever felt worse after a refill, don’t assume it’s in your head. Ask for your original brand to be specified on the prescription.
What You Can Do: A Practical Checklist
Levothyroxine isn’t a set-it-and-forget-it drug. Here’s how to stay safe:
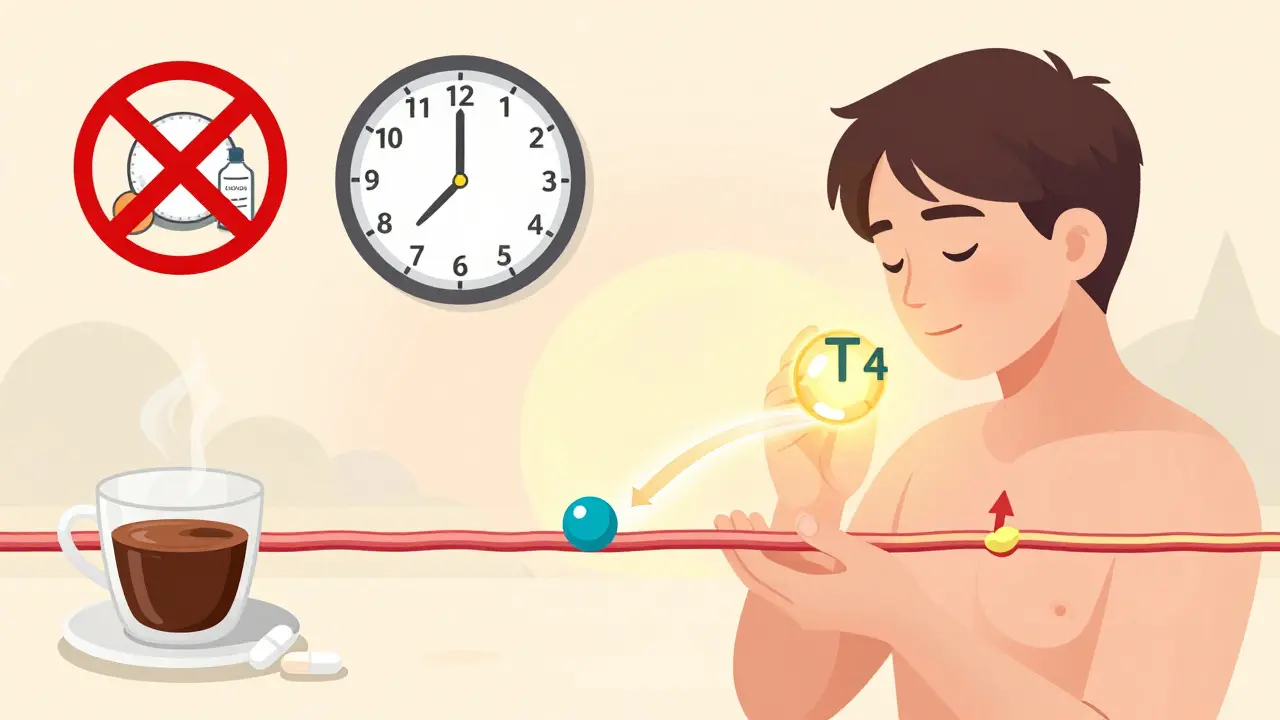
- Take it on an empty stomach. 30 to 60 minutes before breakfast. Coffee, calcium, iron, and antacids can block absorption. If you take supplements, wait at least 4 hours.
- Don’t switch brands without telling your doctor. If you’ve had issues before, ask for the brand name to be written on the prescription. "Dispense as written" is your friend.
- Get TSH tested regularly. Every 6-12 weeks after a dose change. Once stable, at least once a year. More often if you’re pregnant, elderly, or have heart disease.
- Track your symptoms. Use a simple journal: energy levels, weight, mood, heart rate. Bring it to appointments. Numbers matter, but how you feel matters too.
- Know your TSH target. For most adults under 65, 0.5-4.5 mIU/L is ideal. For older adults, up to 7.5 may be acceptable. Ask your doctor what your goal should be.
When to See an Endocrinologist
Not every case needs a specialist. But some do. You should be referred if:
- You’re under 16
- You’re pregnant or postpartum
- You have heart disease, especially if you’ve had a heart attack
- You’re taking amiodarone, lithium, or other drugs that interfere with thyroid function
- You’ve had thyroid cancer and need precise hormone suppression
- Your TSH keeps fluctuating despite dose changes
- You still feel unwell even when your labs look "normal"
Endocrinologists don’t just adjust doses. They look at the whole picture. They check for autoimmune markers, review your medication list, and consider whether you might benefit from T3 combination therapy. If you’ve been struggling for years, it’s not you. It’s the system. Ask for help.

The Bigger Picture
Levothyroxine is prescribed over 127 million times a year in the U.S. alone. It’s cheap. It’s accessible. But accessibility doesn’t mean it’s handled well. The problem isn’t the drug. It’s the lack of follow-up. A pill can’t fix your thyroid if no one’s watching your levels.
Patients who stay on top of their monitoring report 85% satisfaction rates. Those who don’t? They’re the ones stuck in cycles of fatigue, weight gain, and frustration. They’re told it’s depression. Or aging. Or stress. But it’s often just a TSH level that’s out of whack.
Thyroid health isn’t just about taking a pill. It’s about consistency. Communication. And vigilance. Your body needs steady hormone levels. So should your care.
What’s Changing in 2025?
New research is making things more precise. Mayo Clinic studies show that 23% of why people need different doses might be genetic. Some people naturally absorb levothyroxine slower. Others break it down faster. Future dosing might include a simple DNA test to guide your starting dose.
Also, the American Thyroid Association is updating its guidelines to recognize that older adults don’t need the same TSH targets as younger people. A TSH of 6.0 might be perfectly fine for a 72-year-old with no symptoms. But for a 35-year-old? That’s under-treated.
And while combination therapy (T3 + T4) isn’t standard yet, it’s being studied for people who still feel awful despite normal TSH. If you’ve tried everything and still don’t feel right, ask about it. You’re not crazy. You’re just not being heard.
Can I stop taking levothyroxine if I feel better?
No. Hypothyroidism is usually a lifelong condition. Stopping levothyroxine will bring back your symptoms-and can lead to serious complications like heart problems or myxedema coma in extreme cases. Feeling better means the medication is working, not that you no longer need it.
Why do I feel worse after switching to a generic brand?
Even though generics are chemically the same, small differences in how they’re made can affect how your body absorbs the hormone. This can cause subtle shifts in your TSH and free T4 levels, leading to symptoms like fatigue, anxiety, or heart palpitations. If this happens, ask your doctor to prescribe the brand you tolerated best.
Is it safe to take levothyroxine with coffee or calcium supplements?
No. Coffee, calcium, iron, and antacids can block absorption. Take levothyroxine on an empty stomach, at least 30-60 minutes before breakfast. Wait 4 hours before taking supplements or antacids. Consistency matters-do it the same way every day.
How long does it take for levothyroxine to start working?
You might notice small improvements in energy or mood within 2-3 weeks. But full symptom relief usually takes 3-6 months, once your dose is properly adjusted. Blood tests are needed every 6-8 weeks during this time to fine-tune your dose.
Can levothyroxine cause weight loss?
If you were severely under-treated, correcting your thyroid levels may help you lose a few pounds as your metabolism normalizes. But levothyroxine is not a weight-loss drug. Taking more than prescribed can cause dangerous side effects like heart rhythm problems or bone loss. Never increase your dose to lose weight.
What should I do if my doctor won’t test my TSH?
Insist. If your doctor refuses, ask for a referral to an endocrinologist. You have a right to proper monitoring. Keep a symptom journal and bring it with you. Mention that guidelines from the American Thyroid Association and the Specialist Pharmacy Service recommend annual (or more frequent) testing. If you’re still blocked, consider switching providers.
Final Thought: You’re the Key
Doctors rely on labs. But labs don’t tell the whole story. You know how you feel. If something’s off, speak up. Track your symptoms. Know your numbers. Don’t let a pharmacy change your brand without telling your doctor. Don’t skip your blood tests because you "feel fine."
Levothyroxine is a powerful tool. But like any tool, it only works when used correctly. Your health isn’t a statistic. It’s your life. Make sure it’s being managed right.
Christina Bischof
December 16, 2025 AT 09:03Just wanted to say thank you for this. I’ve been on levothyroxine for 7 years and no one ever told me about brand switching being a thing. I thought I was just getting older. Turns out my pharmacy switched me to a generic and I was crashing. Took me 6 months to figure it out. Now I insist on Synthroid. My energy’s back.
RONALD Randolph
December 16, 2025 AT 15:45THIS. IS. NON-NEGOTIABLE. The FDA’s 90–110% bioequivalence window is a JOKE for thyroid hormones. You don’t play roulette with your metabolism. If your doctor won’t write ‘DAW’ or ‘dispense as written,’ find a new one. This isn’t aspirin-it’s endocrine surgery in pill form.
Lisa Davies
December 17, 2025 AT 00:54Thank you for writing this!! 🙌 I was told I was ‘just stressed’ for 2 years until I demanded a TSH test. My level was 8.7. I cried when I finally felt like me again. Please, if you’re tired and it’s not going away-get tested. It’s not in your head.
Cassie Henriques
December 17, 2025 AT 06:48From a clinical pharmacist perspective: the 20% bioavailability variance in generics is clinically significant for levothyroxine because of its narrow therapeutic index. TSH is a log-linear sensor-0.1 mIU/L shift can mean a 12–15% change in free T4. That’s why we track FT4 + TSH, not just TSH. Also, T4-to-T3 conversion varies by SNP rs225014 in DIO1. Genetic testing is the future.
Sai Nguyen
December 17, 2025 AT 08:57Americans always over-medicalize everything. Just take the pill. Stop complaining. In India, we don’t have brand names-we take what’s available. If you feel bad, maybe you’re just lazy.
Benjamin Glover
December 17, 2025 AT 15:25How quaint. In the UK, we’ve known about this since 2016. The MHRA issued guidance. Yet here you are, reinventing the wheel. And you think your ‘checklist’ is revolutionary? It’s basic pharmacology. The real issue is American primary care’s chronic under-resourcing.
Mike Nordby
December 18, 2025 AT 10:59I appreciate the depth here. One thing missing: the role of gut health. Many patients with Hashimoto’s also have SIBO or low stomach acid, which impairs absorption. I’ve seen patients respond dramatically after addressing H. pylori or supplementing with betaine HCl. It’s not just about the pill-it’s about the environment it’s absorbed in.
Nupur Vimal
December 19, 2025 AT 22:47you think your thyroid is the problem? i had a friend who was on levo for 10 years and turned out to have celiac. once she went gluten free her tsh dropped to 1.2. stop blaming the pill. look at your diet. you’re all just looking for magic pills
John Samuel
December 20, 2025 AT 22:17As a former endocrinology nurse and now a patient advocate, I’ve seen the devastation of under-treated hypothyroidism. I’ve held the hands of patients who developed myxedema coma because their TSH was 18.5 and no one checked for 2 years. This isn’t a ‘minor condition.’ It’s a silent killer. Please, if you’re reading this-get tested. Bring a printed copy of the ATA guidelines to your appointment. Print it. Tape it to your fridge. Make your doctor see it. You deserve better than a 5-minute visit and a shrug.
Jocelyn Lachapelle
December 22, 2025 AT 20:17you’re not alone 💛 I was told I was depressed for 3 years. Turns out I was just low on T4. Now I take my pill with a glass of water before coffee. I journal my energy. I say no to brand switches. I’m alive again. You got this.
Jake Sinatra
December 24, 2025 AT 14:21Thank you for highlighting the genetic component. Recent studies from Mayo Clinic and the Thyroid Pharmacogenomics Consortium suggest that polymorphisms in SLCO1B1 and DIO2 account for up to 30% of inter-individual variability in levothyroxine dose requirements. We’re moving toward precision endocrinology. Clinicians who ignore this are practicing 1990s medicine.
Raj Kumar
December 25, 2025 AT 20:36bro i switched to generic and felt like death for 3 months then i went back to synthroid and boom energy back. my doc was like oh u just had a bad week. no. its the pill. always ask for the brand. and dont take it with ur morning protein shake. i learned that the hard way lol