Steroid Hyperglycemia in Diabetes: How to Adjust Insulin and Medications
 Dec, 10 2025
Dec, 10 2025
Steroid Insulin Adjustment Calculator
Steroid Insulin Adjustment Guide
When taking steroids (prednisone, hydrocortisone), insulin needs increase by 30-50% for moderate doses (20mg+ prednisone equivalent) and can double for high doses (100mg+). Adjustments should focus on mealtime insulin for breakfast/lunch and use basal-bolus, not sliding scale.
Key Timing: Steroid-induced glucose spikes typically peak 4-8 hours after dosing. For morning steroid doses, expect largest spikes after breakfast and lunch. Monitor glucose 4x daily: fasting, 2 hours after breakfast, 2 hours after lunch, and before bed.
Your Current Insulin Regimen
Steroid Details
Adjusted Insulin Recommendations
Results will appear here after calculation
Why Steroids Make Blood Sugar Spike in People with Diabetes
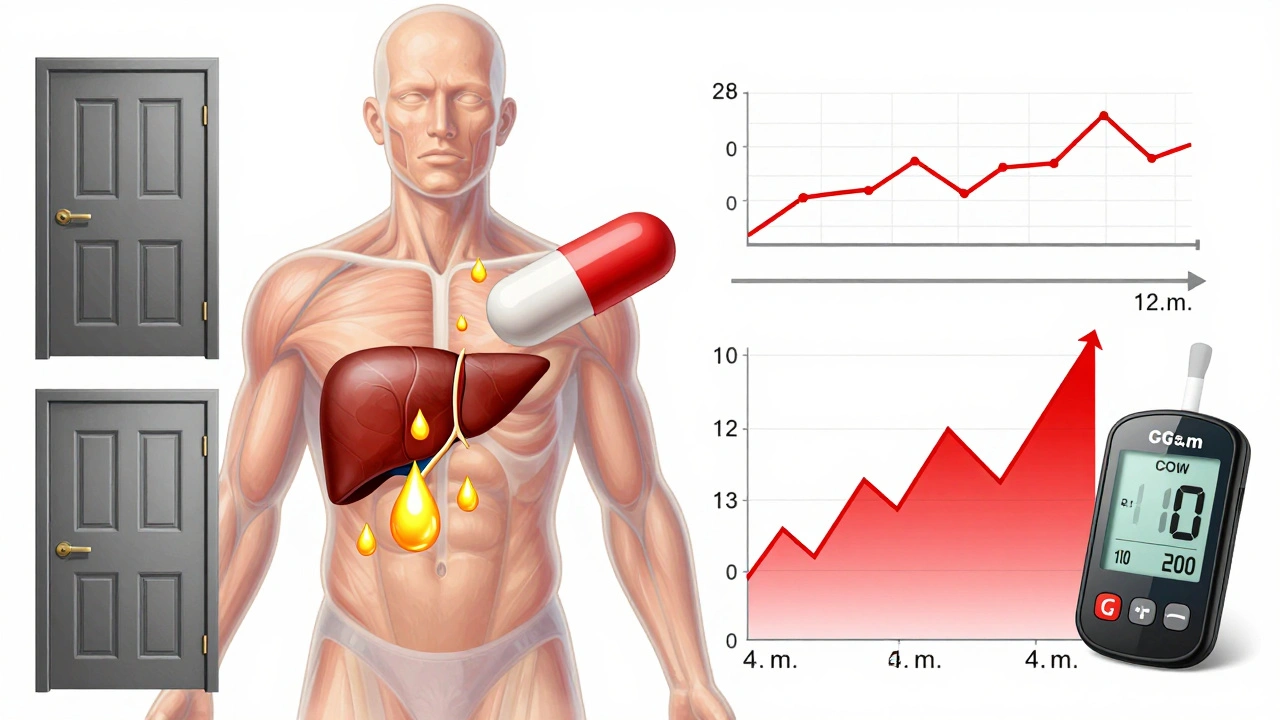
When you start taking steroids like prednisone or hydrocortisone, your blood sugar doesn’t just rise a little-it can go through the roof. This isn’t a coincidence. Steroids interfere with how your body uses insulin. They make your liver dump more glucose into your bloodstream, block insulin from doing its job in muscles and fat, and even reduce how much insulin your pancreas can produce. For someone with diabetes, this is like adding gasoline to a fire. Even people who never had diabetes before can develop high blood sugar from steroids. About 40% of hospitalized patients on steroids end up needing insulin because their blood sugar won’t stay in range.
How Steroids Actually Break Down Your Blood Sugar Control
Steroids don’t just raise blood sugar randomly. They follow a clear pattern. The biggest spike happens 4 to 8 hours after you take your dose. If you take prednisone in the morning, your blood sugar will peak after breakfast and again after lunch. Dinner? Often fine. That’s why checking your glucose only at bedtime or first thing in the morning misses the real problem. Studies show fasting glucose underestimates steroid-induced high blood sugar by 15-20%. The real issue is post-meal spikes, especially after the first two meals of the day.
The science behind it is simple but powerful. Steroids disrupt insulin signaling pathways. They block GLUT4, the protein that pulls glucose into your cells. They ramp up glucagon, the hormone that tells your liver to release sugar. And they damage your pancreatic beta cells so they can’t respond to rising glucose. The higher the steroid dose, the worse it gets. People on 100 mg of hydrocortisone daily are over 10 times more likely to need insulin than those not on steroids.
Who’s Most at Risk for Steroid-Induced High Blood Sugar
Not everyone reacts the same way. If you already have type 2 diabetes, your risk jumps dramatically. But even people without diabetes can crash into hyperglycemia. Key risk factors include:
- Previous diagnosis of diabetes or prediabetes
- Being over 65 years old
- BMI over 30
- Family history of diabetes
- Taking steroids for more than 7 days
- Using other immunosuppressants like tacrolimus (common after transplants)
- Low magnesium levels
- Chronic hepatitis C
Patients on transplant medications face a double hit. Tacrolimus suppresses insulin production, and steroids block insulin action. Together, they make blood sugar control nearly impossible without insulin. One study found that transplant patients on both drugs had a 35-45% higher chance of developing diabetes than those on steroids alone.
How Much Insulin Do You Really Need?
There’s no one-size-fits-all answer, but here’s what works in real-world practice. For patients with existing diabetes starting moderate steroid doses (20 mg prednisone or more per day), insulin needs typically jump by 30-50%. For those on high doses (100 mg hydrocortisone equivalent or more), insulin requirements can double.
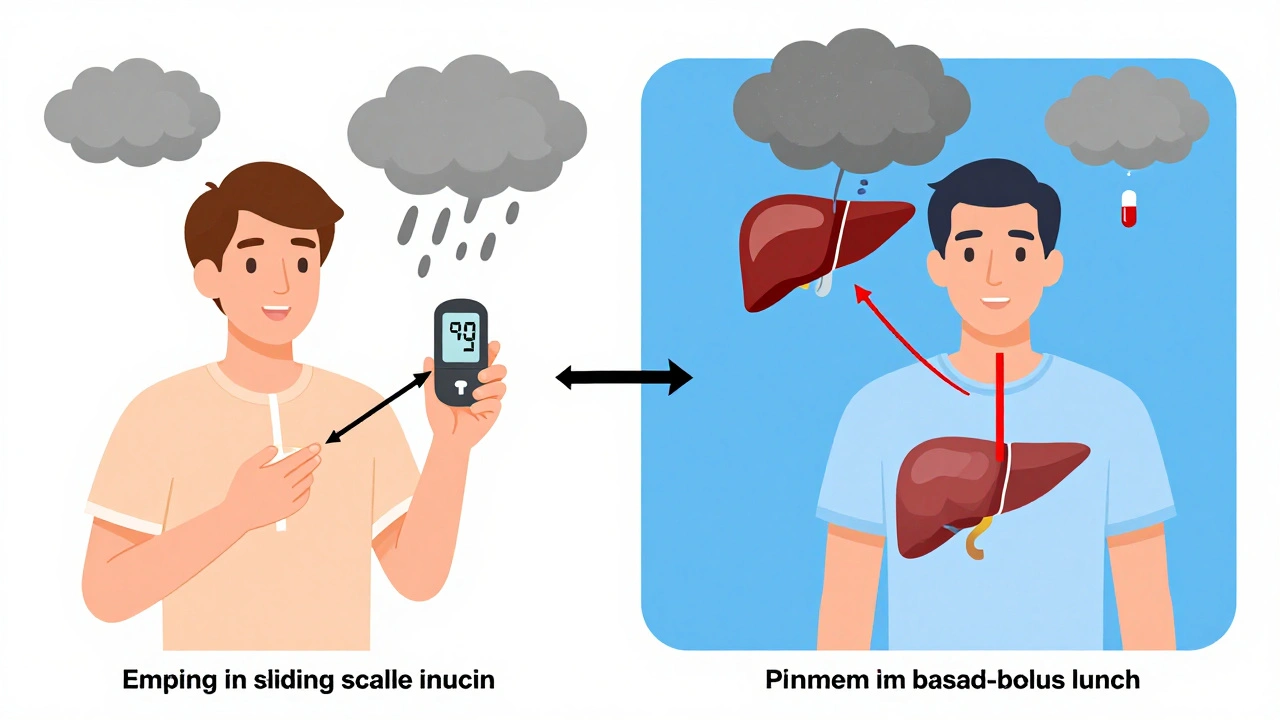
The key is using a basal-bolus insulin plan, not sliding scale alone. Sliding scale just reacts to high numbers-it doesn’t prevent them. Basal-bolus gives you steady background insulin (long-acting) plus fast-acting insulin at meals to cover spikes.
Here’s a practical starting point:
- Basal insulin: Increase by 20-30% from your pre-steroid dose
- Mealtime insulin: Increase by 50-100%, especially for breakfast and lunch
- Evening insulin: Often unchanged, since steroid effects fade by dinner
For example, if you normally take 20 units of Lantus and 8 units of Humalog at breakfast, you might switch to 26 units of Lantus and 16 units of Humalog at breakfast during steroid therapy. Always adjust under medical supervision.
Timing Matters: When to Check Glucose and Adjust Doses
Checking blood sugar only in the morning is like driving with your eyes closed half the time. You need to check at least four times a day: fasting, 2 hours after breakfast, 2 hours after lunch, and before bed. If glucose is above 180 mg/dL twice in a row, increase mealtime insulin by 10-20%.
Here’s the trick: match insulin timing to steroid timing. If you take prednisone at 8 a.m., your blood sugar will peak between 12 p.m. and 4 p.m. That means your lunchtime insulin dose needs to be the biggest. Dinner? Often you can use your usual dose-or even less.
Continuous glucose monitors (CGMs) are game-changers here. A 2021 study showed CGM users adjusted insulin doses 37% more accurately than those using fingersticks. Real-time trends let you see the spike coming and act before it gets dangerous.
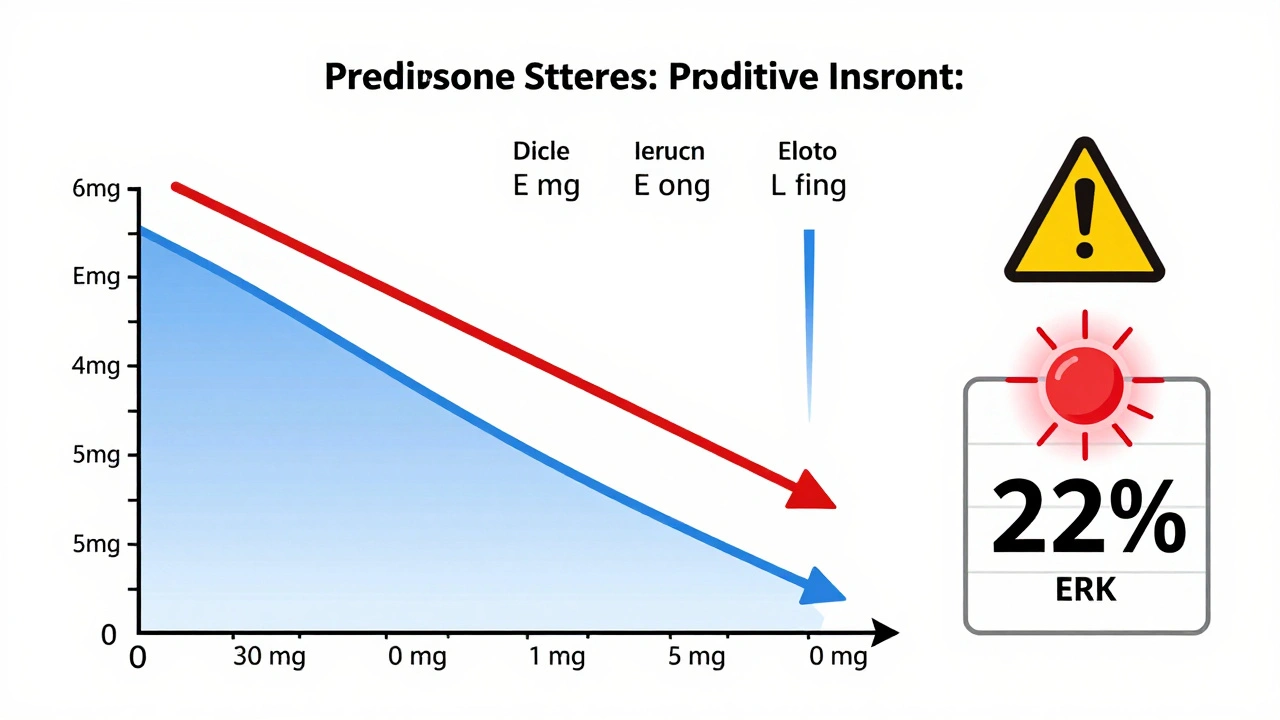
What Happens When You Stop the Steroids?
This is where most people get hurt. When the steroid dose drops, your body starts to recover. Insulin sensitivity improves. Your pancreas wakes up. But if your insulin dose stays the same, you’re setting yourself up for low blood sugar.
Studies show 22% of patients who don’t reduce insulin during steroid tapering end up in the ER with hypoglycemia. That’s not rare-it’s predictable.
Here’s how to avoid it:
- Reduce total daily insulin by 10-20% for every 10 mg drop in prednisone equivalent
- Start reducing insulin when steroid dose drops below 20 mg/day
- Monitor glucose more often during tapering-up to 6-8 times a day
- Don’t wait for symptoms. Low blood sugar can sneak up fast
One hospital found that 18% of readmissions within 30 days after steroid discharge were due to hypoglycemia from unchanged insulin regimens. That’s preventable.
Special Cases: Kids, Transplant Patients, and Outpatients
Children on high-dose steroids (like for asthma or autoimmune disease) often need 25-40% more insulin than adults, with the biggest increases at breakfast and lunch. Parents should work with pediatric endocrinologists to adjust doses weekly.
Transplant patients are the most complex. They’re often on steroids, tacrolimus, and mycophenolate-all of which hurt glucose control. Many need insulin from day one. Some hospitals use specialized tools like Glytec’s eGlucose System, which cuts hypoglycemia by 33% during steroid tapering.
Outpatients are the most at-risk group. Primary care doctors often don’t know how to adjust insulin for steroids. A 2022 CMS report found 22% of steroid-treated patients had preventable complications because no one told them to change their meds. If you’re on steroids at home, ask your doctor: “Do I need to adjust my insulin? When? By how much?” Don’t assume it’s the same as before.
What Not to Do
Here are the top three mistakes doctors and patients make:
- Using sliding scale insulin only-this is reactive, not proactive
- Relying on fasting glucose-misses the real problem (post-meal spikes)
- Not reducing insulin during taper-leads to dangerous lows
Also avoid oral diabetes meds like metformin or sulfonylureas during acute steroid use. They’re often ineffective and can add risk. Insulin is the only reliable tool here.
What’s Changing in 2025
Hospitals are finally catching up. Over 68% of major U.S. medical centers now have formal steroid hyperglycemia protocols. The Joint Commission requires them. Tools like EndoTool and Glytec use algorithms to predict insulin needs based on steroid dose, BMI, and baseline glucose. A 2023 study showed machine learning models can predict insulin needs with 85% accuracy.
Future systems will integrate CGM data with electronic health records. Imagine your insulin pump adjusting doses automatically when your steroid dose changes. Pilot programs at Mayo Clinic and Stanford are already doing this. By 2027, this will be standard for anyone on steroids longer than a week.
Bottom Line: You Can Control This
Steroid-induced hyperglycemia isn’t a death sentence. It’s a temporary, predictable problem with a clear solution: insulin adjustments timed to steroid peaks, frequent monitoring, and careful tapering. The key is acting early-not waiting for blood sugar to hit 300. Work with your care team. Use a CGM if you can. Track your numbers. And never stop adjusting insulin as your steroid dose changes. You’re not fighting your body-you’re helping it cope. And that’s something you can manage, one dose at a time.
Eddie Bennett
December 12, 2025 AT 10:35Monica Evan
December 13, 2025 AT 19:00Lisa Stringfellow
December 13, 2025 AT 22:35Kristi Pope
December 15, 2025 AT 05:25Aman deep
December 15, 2025 AT 05:35Jimmy Kärnfeldt
December 15, 2025 AT 12:26Vivian Amadi
December 16, 2025 AT 17:21Ariel Nichole
December 17, 2025 AT 11:21john damon
December 18, 2025 AT 20:38matthew dendle
December 19, 2025 AT 09:36Taylor Dressler
December 21, 2025 AT 02:24Jean Claude de La Ronde
December 22, 2025 AT 05:41Jim Irish
December 23, 2025 AT 10:29Mia Kingsley
December 24, 2025 AT 19:10Katherine Liu-Bevan
December 25, 2025 AT 23:46