Pulmonary Rehabilitation Benefits for Asthma Patients
 Oct, 18 2025
Oct, 18 2025
Asthma Rehabilitation Benefit Estimator
Enter your current asthma status to see potential improvements from pulmonary rehabilitation.
Lung Function Improvement
Exacerbation Reduction
Hospitalization Savings
Annual Cost Savings
Based on average savings of $1,200 per year for patients completing pulmonary rehab
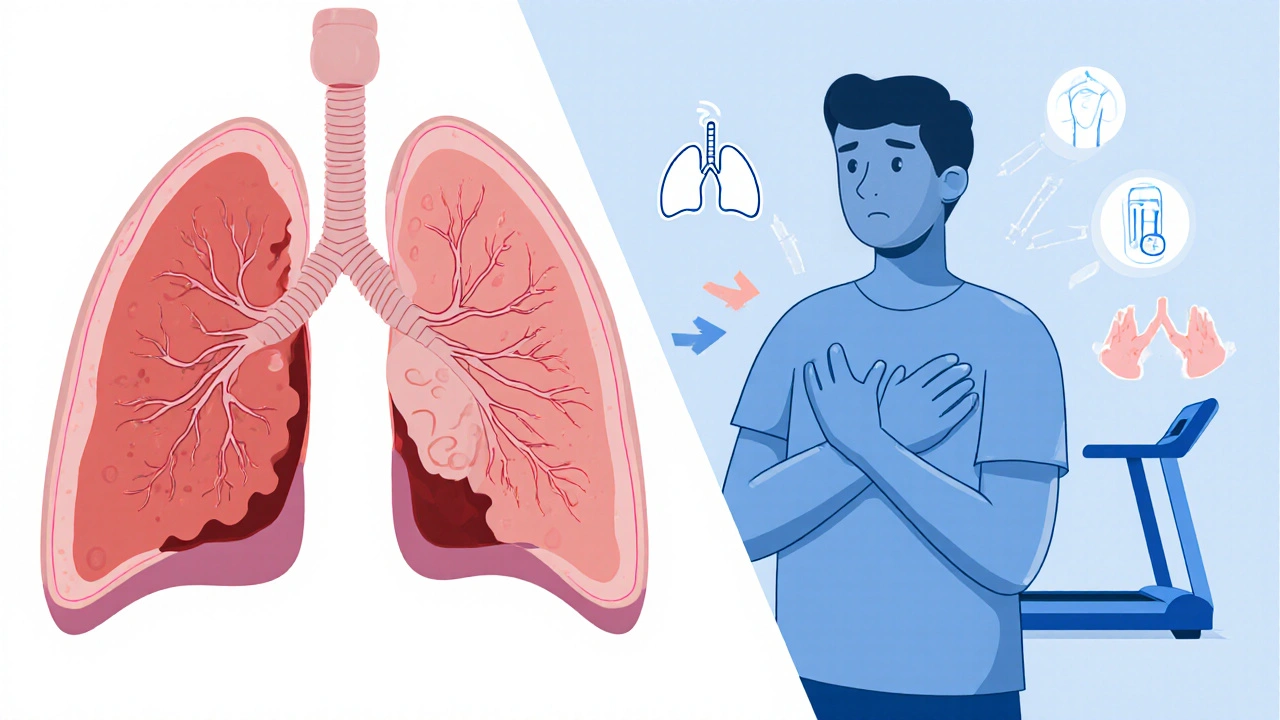
Living with bronchial asthma can feel like you're constantly on guard, waiting for the next breath‑less episode. What if a structured program could give you more control, fewer flare‑ups, and a better quality of life? That's exactly what pulmonary rehabilitation aims to do for asthma patients.
What Is Pulmonary Rehabilitation?
Pulmonary Rehabilitation is a multidisciplinary program designed to improve lung health through guided exercise, breathing training, education, and psychosocial support. It was originally created for chronic obstructive pulmonary disease (COPD) patients, but research over the past decade shows it works wonders for those with bronchial asthma too.
Understanding Bronchial Asthma
Bronchial Asthma is a chronic inflammatory disease of the airways that causes recurring wheeze, shortness of breath, chest tightness, and cough. The inflammation makes the airway muscles hyper‑responsive, so even mild triggers can cause a sudden narrowing of the airways.
How Pulmonary Rehabilitation Helps Asthma
The program attacks asthma from several angles:
- Exercise Training boosts overall fitness and strengthens respiratory muscles, making it easier to breathe during an attack.
- Breathing Exercises teach controlled techniques that reduce hyper‑responsiveness and improve airflow.
- Patient Education empowers individuals to recognize early signs, adjust medication, and avoid triggers.
- Psychosocial Support addresses anxiety and depression, which are common in chronic lung disease.
These components work together to lower airway inflammation, improve lung capacity, and increase confidence in managing symptoms.
Core Components of a Rehab Program
Exercise Training typically involves aerobic activities like treadmill walking, cycling, or swimming, performed at 60‑80% of the patient's maximum heart rate. Sessions last 30‑45 minutes, three times per week, and are gradually intensified as fitness improves.
Breathing Exercises such as diaphragmatic breathing, pursed‑lip breathing, and the “blow‑out” technique help patients control the rate of expiration and keep airways open. Practicing these techniques daily reduces the work of breathing during an asthma episode.
Patient Education covers trigger identification, proper inhaler technique, action‑plan creation, and the role of anti‑inflammatory medication. Knowledge alone can cut emergency visits by up to 30%.
Psychosocial Support often includes group counseling, stress‑reduction workshops, and access to a mental‑health professional. Addressing anxiety lowers the perception of breathlessness, which itself can trigger bronchoconstriction.

Measurable Benefits for Asthma Patients
Clinical studies published between 2020‑2024 show consistent improvements:
- Improved Lung Function: Average increase of 8‑12% in FEV1 (forced expiratory volume in 1 second) after 8‑week programs.
- Reduced Exacerbations: 35% fewer moderate‑to‑severe flare‑ups compared with standard care.
- Better Quality of Life: Scores on the Asthma Quality of Life Questionnaire (AQLQ) rise by 0.9 points, exceeding the minimal clinically important difference.
- Lower Hospital Readmission: 40% drop in asthma‑related hospital stays within six months of completing rehab.
These numbers translate into fewer missed workdays, lower medication costs, and a more active lifestyle.
Real‑World Example
Maria, a 42‑year‑old teacher from Asheville, had frequent nighttime attacks despite using an inhaled corticosteroid. After enrolling in a 10‑week pulmonary rehabilitation program, she reported sleeping through the night, could climb a flight of stairs without wheeze, and her rescue‑inhaler use fell from four times a day to once a week. A post‑program spirometry test showed a 10% rise in FEV1, confirming the physiological gains.
Getting Started: How to Enroll
- Ask your pulmonologist or primary‑care physician for a referral to the nearest pulmonary rehab center.
- Confirm that the program offers a dedicated asthma track; not all centers specialize in asthma.
- Schedule an initial assessment, which will include a Spirometry test to measure baseline lung function.
- Work with the rehab team to set realistic goals (e.g., walk 30 minutes without wheeze).
- Commit to the recommended 8‑12 week schedule; consistency drives results.
Tips to Maximize Your Rehab Results
- Use a Peak Flow Meter daily to track airway variability and adjust actions before symptoms worsen.
- Log your exercise, breathing sessions, and medication usage in a simple notebook or app.
- Stay hydrated; thin mucus is easier to clear.
- Practice breathing techniques during calm moments, not just during attacks.
- Engage with the support group; sharing experiences reinforces adherence.

Pulmonary Rehabilitation vs. Standard Asthma Care
| Aspect | Pulmonary Rehabilitation | Standard Care |
|---|---|---|
| Primary Focus | Exercise, breathing training, education, psychosocial support | Medication and occasional physician visits |
| Delivery Format | Supervised, multi‑week program (8‑12 weeks) | Clinic visits as needed |
| Measured Outcomes | FEV1, AQLQ, exacerbation rate, hospital readmission | Symptom diary, rescue‑inhaler use |
| Patient Involvement | Active daily participation (exercise, breathing, self‑monitoring) | Passive (medication adherence) |
| Cost Effectiveness | Reduced hospitalizations offset program fees (average savings $1,200 per year) | Higher long‑term costs due to frequent ER visits |
Frequently Asked Questions
Frequently Asked Questions
Is pulmonary rehabilitation safe for all asthma severity levels?
Yes, programs are tailored to each patient. Mild, moderate, and severe asthma patients all receive a customized exercise intensity and breathing drills that match their current lung function.
How often should I attend sessions?
Most centers recommend three supervised sessions per week, plus daily home practice of breathing techniques and light aerobic activity.
Will my insurance cover pulmonary rehab for asthma?
Many health plans cover rehab when a physician writes a referral and the program is coded for chronic respiratory disease. It’s worth checking your policy before starting.
How long do the benefits last?
If you keep up with regular exercise, breathing drills, and self‑monitoring, the improvements can be sustained for years. Stopping the routine often leads to a gradual return of symptoms.
Can I do pulmonary rehab at home?
Hybrid models are emerging: initial supervised weeks followed by tele‑health coaching and home‑based exercise plans. Talk to your provider about a remote option if travel is a barrier.
Next Steps
If you or a loved one lives with bronchial asthma, consider asking your doctor about a pulmonary rehabilitation referral. The program isn't just another medical appointment-it's a proven pathway to breathing easier, moving more, and feeling less limited by asthma.
Norman Adams
October 18, 2025 AT 17:44Oh, because adding another hour of treadmill to a wheezy day is exactly what every asthma sufferer dreamed of, right?
Margaret pope
October 19, 2025 AT 22:04Stay active keep breathing easy
Karla Johnson
October 21, 2025 AT 02:24I’ve read through a ton of the literature on pulmonary rehabilitation and can say with confidence that the data speak loudly.
First, the consistent 8‑12% boost in FEV1 across multiple trials is not a fluke.
Second, the reduction in exacerbations by roughly one‑third translates directly into fewer ER visits.
Third, those quality‑of‑life scores moving by nearly a full point are clinically meaningful.
Fourth, the multidisciplinary nature of the programs means patients receive education that they can actually apply at home.
Fifth, the breathing exercises like pursed‑lip and diaphragmatic techniques are low‑cost and can be taught in a single session.
Sixth, the psychosocial support component addresses anxiety, which we know can exacerbate airway constriction.
Seventh, adherence rates improve when patients see tangible gains week after week.
Eighth, insurance providers are beginning to recognize the cost‑saving potential, which helps with coverage.
Ninth, the flexibility of hybrid models-initial supervised weeks followed by tele‑health coaching-makes it accessible even for those in remote areas.
Tenth, the program’s structured schedule instills a habit that lasts well beyond the official end date.
Eleventh, clinicians report that patients feel more empowered to adjust their medication based on objective measures like peak flow.
Twelfth, the community aspect of group sessions fosters peer support, which is a known predictor of better outcomes.
Thirteenth, the overall reduction in hospital readmissions eases the burden on the healthcare system.
Finally, when you combine these physiological and psychological benefits, the argument for making pulmonary rehab a standard part of asthma care becomes undeniable.
Linda A
October 22, 2025 AT 06:44In the quiet corridors of breath, we discover that each inhalation is a fleeting promise, a reminder that even the smallest air currents can shape the vast landscapes of our lives.
Joe Moore
October 23, 2025 AT 11:04Yo they dont tell u that big pharma pushin those inhalers just to keep us hooked on meds while they sell us on fancy rehab programs that are really just a way to collect more data on us lol
Ayla Stewart
October 24, 2025 AT 15:24It’s good to see programs that teach practical steps and give clear guidance on how to track progress.
Poornima Ganesan
October 25, 2025 AT 19:44Honestly, if you haven’t read the latest meta‑analysis, you’re missing the point: pulmonary rehab isn’t just a nice add‑on, it’s the cornerstone of modern asthma management and any clinic that downplays it simply lacks competence.
Rajesh Singh
October 26, 2025 AT 23:04We have a duty to our patients to demand the highest standard of care, and that means refusing to settle for medication alone when comprehensive rehabilitation can deliver true relief.
Matthew Miller
October 28, 2025 AT 03:24Let’s get moving! A little jog, a few breaths, and watch that lung capacity climb – you’ll thank yourself later when the wheeze disappears.
Alex Lineses
October 29, 2025 AT 07:44Integrating cardio‑vascular conditioning with bronchial provocation assessments maximizes ventilatory efficiency; stay consistent with the protocol and you’ll see measurable improvements in tidal volume and VO₂ max.
Lyle Mills
October 30, 2025 AT 12:04Feeling frustrated with asthma is normal and it’s okay to take it one step at a time
Barbara Grzegorzewska
October 31, 2025 AT 16:24Only true believers in our great nation understand that cutting edge rehab is a privilege, not some cheap foreign fad – if you’re not up to the standard, maybe you’re just not cut from the right cloth.
Nis Hansen
November 1, 2025 AT 20:44When we contemplate the act of breathing, we confront the intersection of biology and agency; pulmonary rehabilitation invites us to reclaim agency through disciplined practice, aligning physiological capacity with intentional effort.
Fabian Märkl
November 3, 2025 AT 01:04Absolutely love this approach! 🏃♂️💨 Keep it up and you’ll be breathing easy in no time! 🌟
Avril Harrison
November 4, 2025 AT 05:24Interesting stuff, especially the bit about hybrid programs – makes it way more doable for busy folks.