Psoriasis Treatment Options: Plaque, Guttate, and Systemic Therapies Explained
 Feb, 14 2026
Feb, 14 2026
Psoriasis isn’t just a skin rash. It’s a full-body immune system glitch that shows up on your skin - sometimes as thick, scaly plaques, other times as tiny, drop-like spots, or even as widespread inflammation that affects your joints, heart, and metabolism. If you’ve been told you have psoriasis, you’re not alone. Around 125 million people worldwide live with it, and the type you have - plaque, guttate, or something more systemic - determines what treatments actually work.
What You’re Really Dealing With
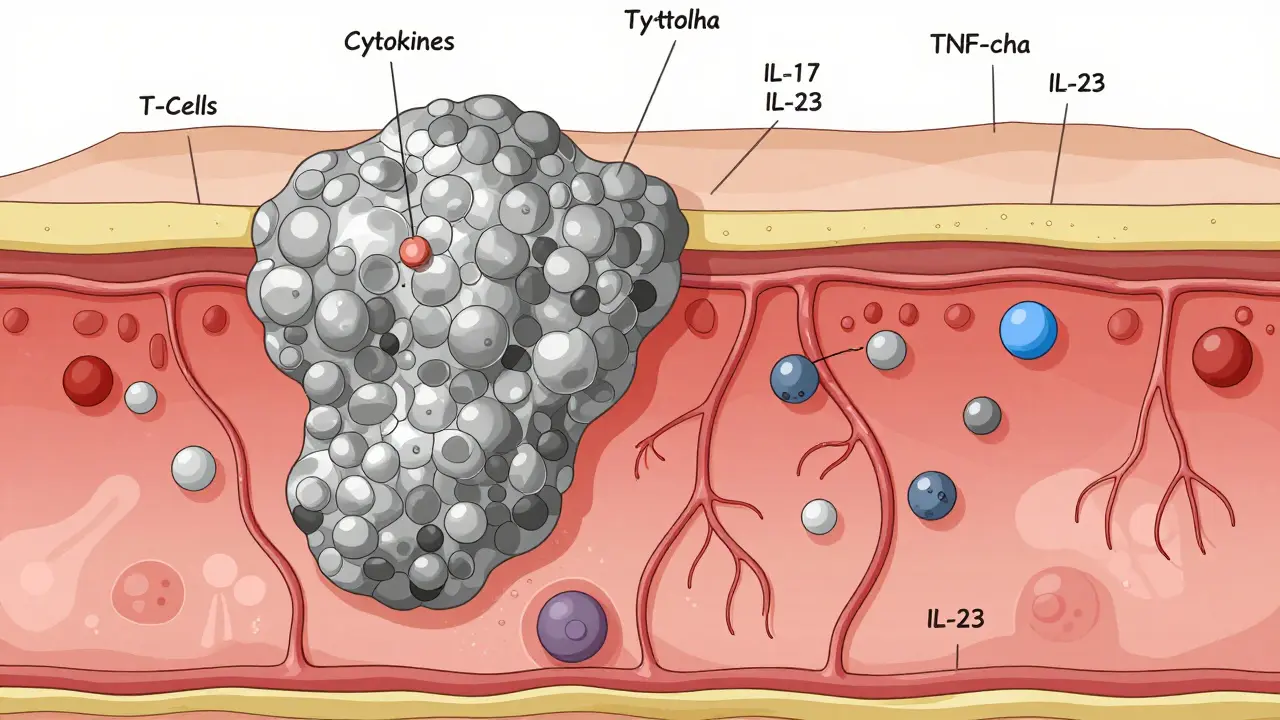
Most people (80-90%) have plaque psoriasis. That’s the classic red, raised, silvery-scaled patch, often on elbows, knees, scalp, or lower back. It’s stubborn, it’s visible, and it doesn’t just sit on the surface. Underneath, your immune system is stuck in overdrive, firing off inflammatory signals like TNF-alpha, IL-17, and IL-23. These chemicals tell skin cells to multiply too fast, building up those thick plaques. Then there’s guttate psoriasis - often triggered by a strep throat or viral infection. It shows up as dozens of small, teardrop-shaped spots across the torso, arms, or legs. It’s more common in kids and young adults. Unlike plaque psoriasis, guttate can sometimes clear on its own, especially if the infection is treated. But if it sticks around, it can turn into plaque psoriasis later. And then there’s the hidden part - the systemic side. About 30% of people with psoriasis develop psoriatic arthritis. That’s joint pain, stiffness, swelling - sometimes before the skin even flares. You’re also at higher risk for heart disease, diabetes, and fatty liver. This isn’t just a skin condition. It’s a chronic inflammatory disease that needs a whole-body approach.Topical Treatments: The First Line
If your psoriasis covers less than 5% of your body, you might start with creams and ointments. But don’t expect miracles. Topicals help manage mild cases, but they rarely clear severe disease. Corticosteroids are the go-to. They come in different strengths - from mild (like hydrocortisone) to very strong (class I). But long-term use on thin skin (like your face or groin) can cause thinning, stretch marks, or rebound flares. That’s why doctors often pair them with calcipotriol, a vitamin D analog that slows skin cell growth. Together, they’re more effective than either alone. Newer options like tapinarof cream (1%) are changing the game. In clinical trials, about 35% of users hit 75% skin clearance after 12 weeks. It works differently - not by suppressing immunity, but by calming inflammation at the cellular level. It’s less likely to cause skin thinning, which makes it safer for long-term use on sensitive areas. For scalp psoriasis, a foam or solution works better than a thick cream. A combo of calcipotriol and betamethasone foam has an 89% response rate. For nail psoriasis, a single shot of triamcinolone directly into the nail bed improves pitting and discoloration in 75% of cases.Oral Systemic Drugs: Beyond the Cream
When topical treatments aren’t enough, you move to pills. These work from the inside out. Methotrexate has been around for decades. It’s cheap, effective, and used for both psoriasis and psoriatic arthritis. At 10-25 mg per week, about half of users get 75% skin clearance in 16 weeks. But it needs regular blood tests - it can affect your liver and bone marrow. Folic acid supplements help reduce side effects like nausea. Cyclosporine works faster. In 12-16 weeks, 60-70% of users see major improvement. But it can raise blood pressure and damage kidneys. That’s why it’s usually a short-term option - 6 to 12 months max. Acitretin is a retinoid, a vitamin A derivative. It helps with thick, scaly plaques. But it’s not for women who could get pregnant - it causes severe birth defects. You must avoid alcohol while taking it, and it can dry out your eyes and lips. Apremilast (Otezla) is newer. It’s taken twice daily, and about one-third of users get 75% clearer skin in 16 weeks. It’s not as strong as biologics, but it’s safer. No blood tests needed. Common side effects? Diarrhea and headache - usually mild and temporary. Deucravacitinib (Sotyktu) is the first oral TYK2 inhibitor approved for psoriasis. Taken once daily, it clears 59% of users to 75% at 16 weeks. It’s targeted, so it doesn’t suppress your whole immune system like older drugs. It’s also easier to take than injections.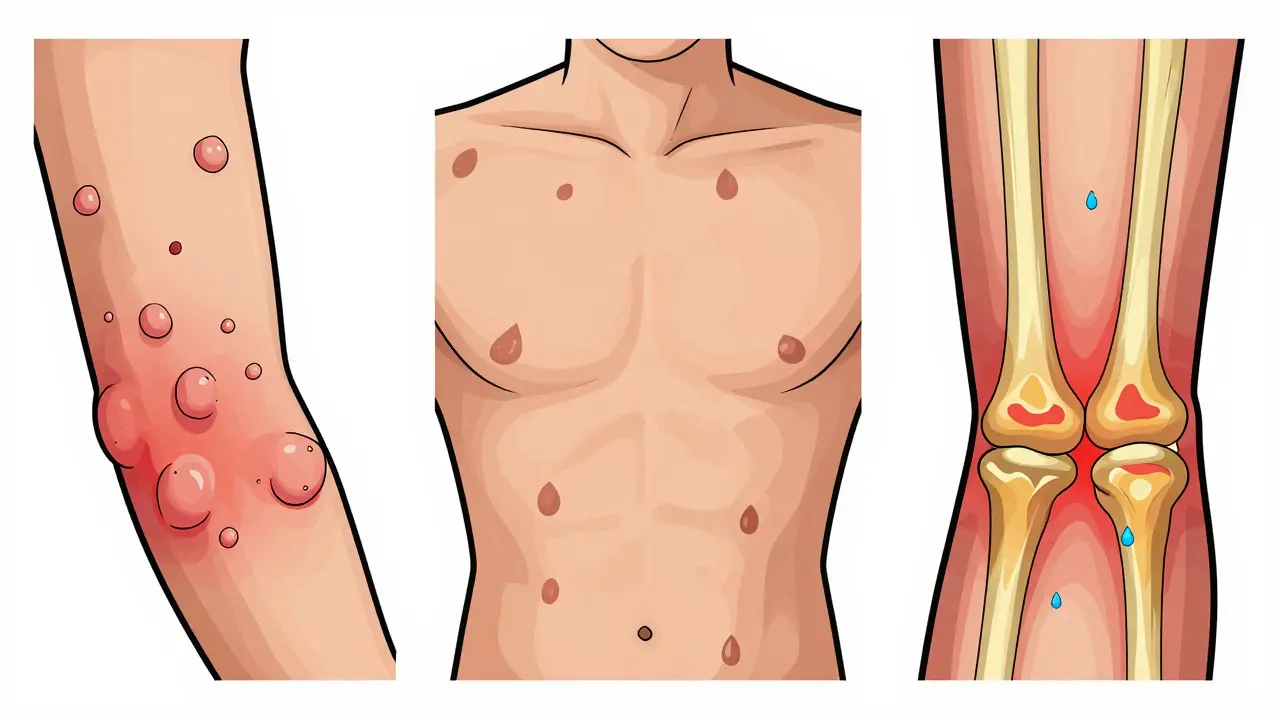
Biologics: The Game Changers
If pills don’t work, or if your psoriasis is severe, biologics are where things get powerful. These are injectable or IV drugs that target specific parts of your immune system. TNF-alpha blockers like adalimumab (Humira) were the first biologics. They help 78% of users reach 75% skin clearance. But they can increase infection risk, and some people lose response over time. IL-17 inhibitors - like secukinumab (Cosentyx) - are faster. Many see improvement in 2-4 weeks. About 79% hit 90% clearance at 16 weeks. But if you have Crohn’s disease or ulcerative colitis, these can make it worse. Avoid them if you have inflammatory bowel disease. IL-23 inhibitors - guselkumab (Tremfya), risankizumab (Skyrizi), tildrakizumab (Ilumya) - are now the gold standard. Why? Because they target a more upstream part of the inflammation chain. In studies, 84-90% of users hit 90% skin clearance. And they’re dosed less often - every 8 to 12 weeks after the initial doses. That means fewer injections, better adherence. Real-world data from 31,521 patients shows risankizumab has the highest persistence rate - 78% are still on it after a year. Guselkumab isn’t far behind at 75%. These drugs also work better on scalp and nail psoriasis than older biologics. A new player, ebdarokimab, is showing promise in trials. In one study, 80% of users hit 75% clearance in a year. It’s still under review, but early results suggest it could be a strong option for hard-to-treat cases.Choosing the Right Treatment
There’s no one-size-fits-all. Your treatment depends on more than just how bad your skin looks. If you have joint pain - start with a biologic that treats both psoriasis and psoriatic arthritis. Methotrexate, adalimumab, or IL-23 inhibitors are good choices. If you have IBD - avoid IL-17 inhibitors. Go with IL-23 blockers. They’re safer for your gut. If you hate needles - try deucravacitinib or apremilast. Oral options are improving fast. If you’re young and want long-term control - IL-23 inhibitors may be your best bet. Studies show 85-90% of people stay clear for years with quarterly dosing. Some even stop treatment after 2-3 years and stay clear. If cost is a concern - biologics are expensive. Guselkumab can cost $34,200 a year. But 85% of insured patients pay $0-$150 out of pocket thanks to manufacturer assistance programs. Always ask your dermatologist about patient support.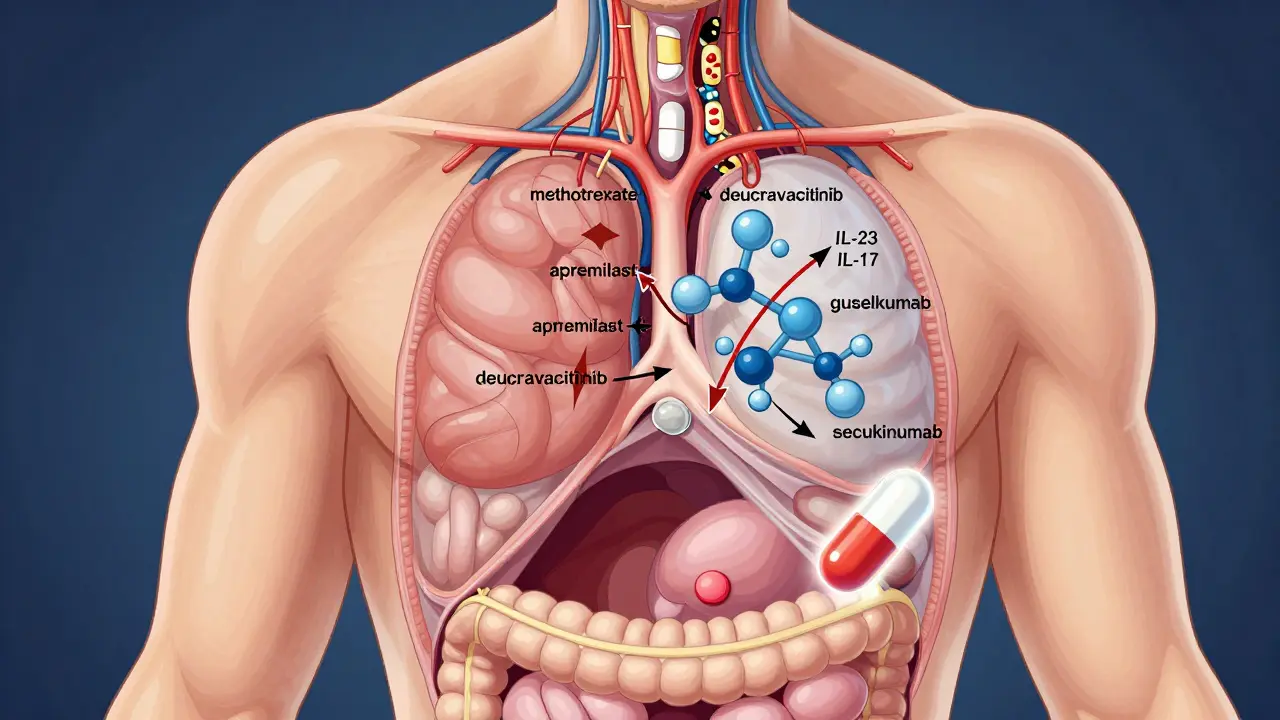
What’s Coming Next
The future of psoriasis treatment is heading toward precision and convenience. Researchers are now classifying psoriasis into subtypes - not just plaque or guttate, but by immune signatures. About 20-25% of patients don’t respond to IL-17 or IL-23 drugs because their psoriasis is driven by a different pathway - type I interferon. That means future treatments might be chosen based on a blood test, not trial and error. Oral peptides that mimic biologics are in phase 3 trials. These would be pills that block IL-23 - with the same power as injections, but no needles. One showed 82% clearance in trials. If approved, this could be a game-changer for people who avoid shots. Topical JAK inhibitors are also on the horizon. Early data shows they could clear 50-60% of plaque psoriasis without systemic side effects. That means you might not need pills or injections for moderate cases. And the biggest shift? Doctors are now considering whether to stop treatment entirely in people who achieve complete clearance. Early data from the GUIDE trial suggests some patients can stay clear for months - even years - after stopping guselkumab. We might be moving toward a functional cure, not just management.What Patients Are Saying
Reddit user u/PsoriasisWarrior shared: "After failing methotrexate and adalimumab, guselkumab cleared 95% of my plaques in 3 months. Quarterly injections? Life-changing. Still cost $500/month with insurance." On Drugs.com, 68% of guselkumab users rated it "excellent." But 18% reported injection site reactions - a small price for many. Others say: "It took 4 months for secukinumab to work. I needed faster relief for a job interview." Timing matters. IL-17 inhibitors work faster than IL-23 or TNF blockers. And a common tip? Use a humidifier in winter. Dry air makes plaques worse. Apply moisturizer right after showering. Occlude stubborn patches with plastic wrap overnight - it helps topicals penetrate deeper.How to Get Started
Talk to a dermatologist who specializes in psoriasis. Don’t wait until it’s severe. Early treatment reduces joint damage and heart risk. Ask about:- Your PASI score (how much skin is affected)
- Your DLQI score (how it impacts your life)
- Whether you have joint symptoms
- Your insurance coverage for biologics
- Patient assistance programs