Pregnancy and Lactation Labeling Rule (PLLR): How to Read FDA Drug Safety Info
 Dec, 7 2025
Dec, 7 2025
PLLR Label Comparison Tool
Old Pregnancy Risk System
Simple letter categories (A, B, C, D, X) without context or details.
"Category C: Use with caution during pregnancy. Animal studies show risk but human data is limited."
Key limitations:
- No context or real-world data
- Risk categories often misleading
- No guidance for patients
- Misinterpreted as safety rankings
New PLLR Structure
Three detailed sections with actionable information.
"Risk Summary: Use during pregnancy may cause oligohydramnios... Discontinuing the drug often restores fluid levels."
Key advantages:
- Plain-language summaries
- Clinical guidance
- Evidence-based data
- Specific recommendations
Real-World Examples
Lithium Example
Risk Summary:
Lithium use during pregnancy is associated with a 0.05% to 0.1% risk of Ebstein's anomaly, a rare heart defect. Risk is highest during the first trimester.
Clinical Considerations:
Maternal serum levels should be monitored closely, and dose adjustments may be needed. Consider pregnancy exposure registry.
Data:
Human studies showing increased risk of cardiac abnormalities in first-trimester exposure. No adequate animal studies.
ACE Inhibitors Example
Risk Summary:
Use after the first trimester can cause kidney damage, low amniotic fluid, and even fetal death.
Clinical Considerations:
Discontinuation of the drug often leads to improvement in fetal outcomes. Avoid use after the first trimester.
Data:
47 women exposed in the first trimester: 2 had minor limb malformations. 80% of cases showed fetal kidney abnormalities resolved after discontinuation.
For years, if you were pregnant or breastfeeding and your doctor prescribed a medication, you’d see a simple letter on the label: A, B, C, D, or X. That was it. No context. No details. Just a letter that meant little to no one outside of a pharmacy. But in 2014, the FDA changed all that. The Pregnancy and Lactation Labeling Rule (PLLR) replaced those outdated letters with real, readable, and meaningful information. Now, instead of guessing what a ‘C’ means, you get a clear breakdown of what the drug might do to you, your baby, or your breast milk.
Why the Old System Failed
The old pregnancy letter categories-A through X-were never meant to be used as safety rankings. But that’s exactly how doctors and patients started treating them. A drug labeled ‘B’ was assumed safe. A ‘C’ was seen as risky. A ‘D’? Probably avoid. And ‘X’? Don’t even think about it. The problem? Those letters didn’t reflect real-world data. A drug with no human studies got a ‘B’ just because animal tests showed no harm. Meanwhile, a drug with clear evidence of risk in humans-like one that caused birth defects in 5% of cases-got a ‘C’ because animal data was mixed. That created a dangerous illusion: untested drugs looked safer than tested ones. That’s why the FDA scrapped the system. They knew doctors needed more than a letter. They needed facts. Numbers. Context. Especially since over 6 million pregnancies happen in the U.S. every year, and most pregnant women take three to five prescription medications during that time.The New PLLR Structure: Three Clear Sections
The PLLR doesn’t just tweak the old labels-it rebuilds them. Now, all prescription drug labels include three new subsections under Section 8: Pregnancy, Lactation, and Females and Males of Reproductive Potential. Each one follows the same simple format: Risk Summary, Clinical Considerations, and Data. Let’s break them down.8.1 Pregnancy: What Happens to the Baby?
This section answers the most urgent question: Will this drug hurt my baby?- Risk Summary: This isn’t a letter. It’s a plain-language summary. For example: “Use during pregnancy may cause oligohydramnios, a condition where amniotic fluid levels drop dangerously low. Discontinuing the drug often restores fluid levels.”
- Clinical Considerations: This tells you what to do. Does the drug need a dose change during pregnancy? Does timing matter? Should you stop it in the third trimester? Is there a pregnancy registry you can join to help track outcomes?
- Data: Here’s the evidence. Human studies. Animal studies. Case reports. You’ll see how many women were studied, what outcomes occurred, and whether the data is strong or limited.
8.2 Lactation: What Goes Into the Milk?
Breastfeeding mothers need to know: Will my baby get this drug? And if so, will it hurt them? The Lactation section gives you:- How much of the drug ends up in breast milk-measured as a percentage of the mother’s dose.
- Whether the drug affects milk production.
- Any known effects on the infant, like drowsiness, poor feeding, or changes in heart rate.
- Whether there are alternatives that are safer for breastfeeding.
8.3 Females and Males of Reproductive Potential: Planning Ahead
This section is often overlooked, but it’s critical. It answers questions like:- Do I need a pregnancy test before starting this drug?
- What kind of birth control should I use while taking it?
- Can this drug affect my fertility?
What’s Missing? Why That’s a Good Thing
The FDA didn’t just add new sections-they removed old ones. No more “Nursing Mothers” or “Labor and Delivery” as separate headings. Why? Because those details belong where they matter: inside the Pregnancy and Lactation sections. They also removed standardized risk phrases like “may cause fetal harm.” That phrase was used on 90% of labels. It meant nothing. Now, every risk description is specific to the drug. And they eliminated the “inadvertent exposure” section. Why? Because if you accidentally took a drug during pregnancy, the risk doesn’t change just because it was unplanned. The data stays the same. So why repeat it?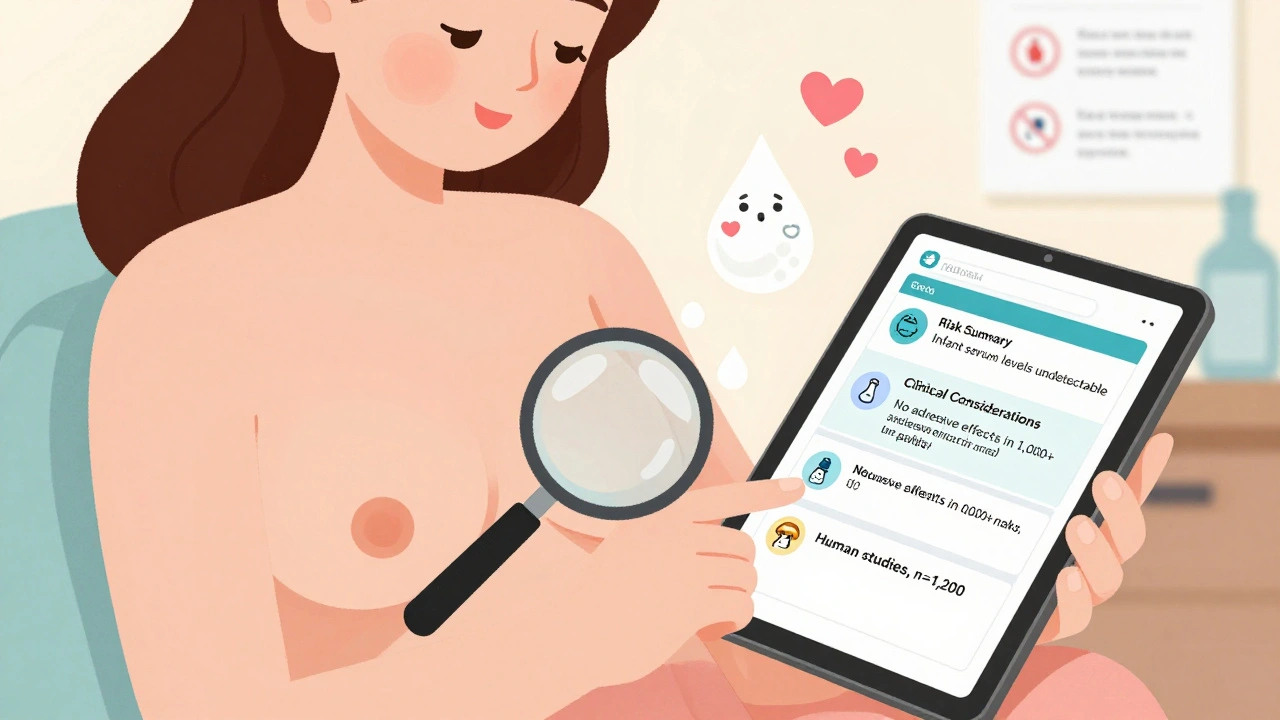
How This Helps Real People
Imagine you’re a nurse practitioner in Boise, and a 32-year-old woman comes in at 10 weeks pregnant. She’s been on lithium for bipolar disorder for five years. She doesn’t want to stop it-but she’s terrified of harming her baby. Before PLLR, the label said “Category C.” That’s it. No guidance. No data. Just fear. Now, the label says: “Lithium use during pregnancy is associated with a 0.05% to 0.1% risk of Ebstein’s anomaly, a rare heart defect. Risk is highest during the first trimester. Maternal serum levels should be monitored closely, and dose adjustments may be needed. Consider pregnancy exposure registry.” Suddenly, you have a conversation. You can say: “The risk is very low, but we’ll check your levels every two weeks. We’ll also connect you with the registry so we can learn from your experience.” That’s not just labeling. That’s care.What’s Changed Since 2014?
The PLLR didn’t stop evolving. Since its launch, the FDA has pushed for more detailed data. Labels now often include:- Specific numbers: “In 47 women exposed in the first trimester, 2 had minor limb malformations.”
- Timing: “Risk increases after 20 weeks of gestation.”
- Withdrawal effects: “Discontinuing the drug led to resolution of fetal kidney abnormalities in 80% of cases.”

How to Use PLLR Labels as a Patient
You don’t need to be a doctor to read these labels. Here’s how:- Find the “Use in Specific Populations” section (Section 8).
- Read the Risk Summary first. That’s the bottom line.
- Look for phrases like “may cause,” “associated with,” or “risk appears low.”
- Check if there’s a pregnancy registry. If so, ask your doctor how to join.
- Don’t ignore the Clinical Considerations. They tell you what to do next.
What About Other Countries?
The U.S. isn’t alone in this. The European Medicines Agency (EMA) also has pregnancy labeling rules. But here’s the catch: a 2023 study found that in 68% of cases, the FDA and EMA used completely different language to describe the same drug’s risks. One might say “risk of fetal harm is low.” The other says “potential for serious adverse effects.” That’s confusing. And it’s why some doctors in the U.S. still check European labels. But the PLLR is still the gold standard for clarity and detail.Final Thought: Better Labels, Better Outcomes
The PLLR didn’t just change how drugs are labeled. It changed how we think about pregnancy and medication. It stopped treating pregnant women as a risk group to avoid-and started treating them as people who need honest, detailed information to make their own choices. It’s not perfect. Some labels still feel too technical. Some data is still limited. But the shift is real. And for the millions of women who take medications during pregnancy or while breastfeeding, it’s made all the difference.What does a PLLR label look like compared to the old one?
The old label used a single letter-A, B, C, D, or X-to summarize risk. The PLLR label uses three detailed subsections: Pregnancy, Lactation, and Reproductive Potential. Each includes a Risk Summary, Clinical Considerations, and Data section with real-world evidence, not just categories.
Are all drugs required to follow the PLLR?
Yes. All prescription drugs and biological products approved since June 30, 2001, must follow PLLR. Older drugs were required to remove the old letter categories by December 2017 and update their labels to the new format. Over-the-counter drugs and supplements are not covered by PLLR.
Can I trust the data in PLLR labels?
The data comes from human studies, animal studies, case reports, and pregnancy registries. While not all data is perfect-some is limited by small sample sizes-the FDA requires manufacturers to cite sources and be transparent about gaps. The goal isn’t to hide uncertainty; it’s to make it clear.
What if my drug’s label still has the old letter categories?
If your drug was approved before June 30, 2001, and hasn’t been updated since, it might still show the old letters. But by law, those letters must be removed. If you see them, contact your pharmacist or the manufacturer. The updated PLLR version should be available. Always ask for the most recent label.
Does PLLR apply to breastfeeding medications too?
Yes. The Lactation section (8.2) is mandatory for all drugs that may pass into breast milk. It includes how much of the drug enters milk, potential effects on the infant, and whether breastfeeding is advised. This section is just as detailed as the Pregnancy section.
Richard Eite
December 9, 2025 AT 07:55Katherine Chan
December 11, 2025 AT 01:38Philippa Barraclough
December 12, 2025 AT 21:14Tim Tinh
December 13, 2025 AT 11:02Olivia Portier
December 14, 2025 AT 13:20Rich Paul
December 15, 2025 AT 00:17Lauren Dare
December 15, 2025 AT 14:38Gilbert Lacasandile
December 17, 2025 AT 08:47William Umstattd
December 19, 2025 AT 05:35Simran Chettiar
December 20, 2025 AT 16:50Anna Roh
December 21, 2025 AT 07:02om guru
December 23, 2025 AT 03:51Tiffany Sowby
December 23, 2025 AT 23:30