Myasthenia Gravis Treatment: How Modern Therapies Restore Muscle Strength
 Jan, 3 2026
Jan, 3 2026
Myasthenia gravis (MG) isn’t just muscle weakness. It’s a breakdown in communication between your nerves and muscles-like a broken wire in a light switch. You try to lift your arm, blink your eye, or swallow food, but the signal doesn’t get through. And it gets worse the more you use the muscle. This isn’t fatigue from a long day. This is myasthenia gravis, an autoimmune disorder where your immune system attacks the very place nerves meet muscles: the neuromuscular junction.
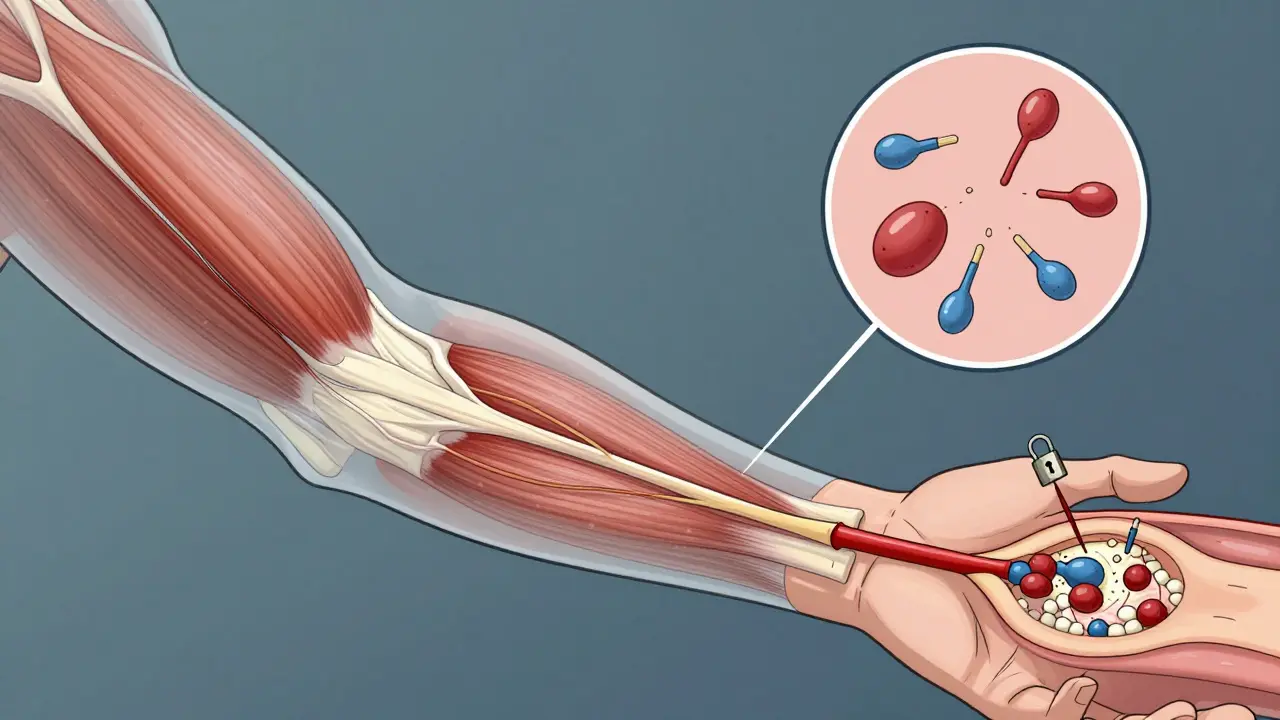
How Myasthenia Gravis Actually Works
Your body makes proteins called acetylcholine receptors (AChR) on muscle cells. These receptors are like locks that catch the key-acetylcholine-that nerves send to tell muscles to contract. In MG, your immune system produces antibodies that block or destroy those receptors. About 85% of people with generalized MG have these AChR antibodies. Another 5-8% have antibodies against MuSK, a different protein involved in the same process. The rest, about 1 in 10, test negative for any known antibody-but they still have MG. That doesn’t mean it’s not real. It just means we haven’t found the antibody yet. The result? Muscles tire quickly. Drooping eyelids. Double vision. Trouble speaking or chewing. Weak arms or legs. In severe cases, breathing muscles fail. That’s a myasthenic crisis-and it’s life-threatening. This isn’t new. Doctors noticed this pattern as far back as 1672. But it wasn’t until 1973 that scientists Patrick and Lindstrom proved it was autoimmune. That discovery changed everything. Suddenly, treatment wasn’t just about managing symptoms. It was about stopping the immune system from attacking.The Four Pillars of MG Treatment Today
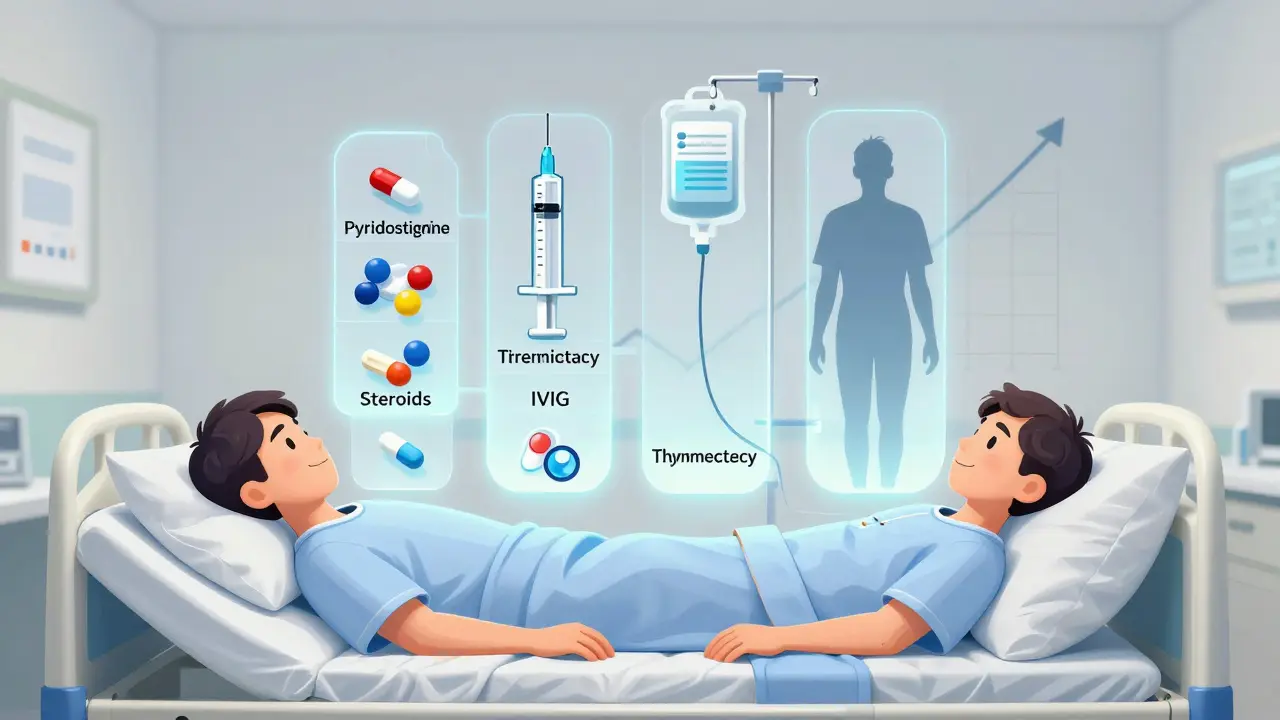
Modern MG care isn’t one-size-fits-all. It’s layered. Think of it like building a wall: you need a foundation, bricks, mortar, and a sealant. Each layer has a purpose. 1. Symptomatic relief: Acetylcholinesterase inhibitorsPyridostigmine (Mestinon) is the first drug most patients get. It doesn’t fix the immune problem. It just helps the signal get through longer by slowing down the breakdown of acetylcholine. Doses are usually 60-120 mg every 3-6 hours. It works fast-within minutes. But it doesn’t last long. And it has side effects: cramps, diarrhea, nausea. About 4 in 10 people can’t tolerate it well. Still, it’s the starting point for almost everyone. 2. Immunosuppression: Steroids and oral drugs
If pyridostigmine isn’t enough, doctors turn to immunosuppressants. Prednisone, a steroid, is often the next step. It shuts down the immune system broadly. About 70-80% of people improve. But the cost is high. Weight gain? Common. Bone loss? Happens in 1 in 4 after one year. Diabetes? Appears in 15-20%. Azathioprine and mycophenolate are slower-acting but safer long-term. They take 6-12 months to work fully, but they’re the backbone of maintenance therapy for many. 3. Fast-acting rescue: IVIG and plasmapheresis
When someone has a crisis-trouble breathing, swallowing, or moving-they need immediate help. IVIG (intravenous immunoglobulin) floods the body with healthy antibodies that confuse the bad ones. Plasmapheresis physically pulls antibodies out of the blood. Both work in days, not weeks. But their effect lasts only weeks. They’re not cures. They’re emergency brakes. 4. Surgery: Thymectomy
The thymus gland, tucked behind the breastbone, is a key player in MG. In many patients, it’s enlarged or contains tumors (thymomas). Removing it-thymectomy-can change the course of the disease. The MGTX trial in 2016 showed that AChR-positive patients who had thymectomy needed 56% less steroid over three years and were 67% less likely to be hospitalized. Complete remission rates jump to 35-40% at five years versus 15-20% with meds alone. Surgeons now use minimally invasive techniques, but long-term data on these methods is still being collected.
The New Wave: Targeted Biologics
Since 2017, the treatment landscape exploded. Seven FDA-approved drugs now target specific parts of the immune attack. These aren’t just new pills. They’re precision tools. Complement inhibitors: Eculizumab, Ravulizumab, ZilucoplanThese drugs block the final step of the immune attack-the complement system-that destroys the receptor. Eculizumab, approved in 2017, showed 88% of patients improved significantly in trials. But there’s a catch: you must get vaccinated against meningococcus before starting. These drugs cost $500,000-$600,000 a year. Insurance approvals can take 3-6 months. Still, for severe AChR-positive MG, they’re life-changing. FcRn inhibitors: Efgartigimod, Rozanolixizumab, Nipocalimab, Batoclimab
This is the biggest breakthrough. FcRn is the protein that keeps antibodies alive in your blood. Block it, and your bad antibodies get flushed out. Efgartigimod (Vyvgart) and rozanolixizumab (Rystiggo) reduce IgG antibodies by 60-75%. Effects show up in 1-2 weeks-faster than any other treatment. Nipocalimab, approved in April 2025, cuts IgG by 70-80%. Batoclimab’s phase 3 results in early 2025 showed 65% of patients reached minimal manifestation status versus 25% on placebo. These drugs work across antibody types-even in seronegative MG. The ADAPT SERON study in 2024 showed 68% of seronegative patients responded to efgartigimod. That’s huge. For the first time, we have a treatment that doesn’t depend on knowing the exact antibody. B-cell therapy: Rituximab
Rituximab wipes out B-cells, the factories that make antibodies. It’s especially powerful in MuSK-MG, with 80% response rates. But in AChR-MG, it’s only about 55% effective. It takes 8-16 weeks to work. It costs $10,000-$15,000 per course. Many doctors use it after steroids fail, especially in MuSK patients.
What Works Best? A Real-World Comparison
| Treatment Type | Onset | Duration | Best For | Annual Cost | Key Risks |
|---|---|---|---|---|---|
| Pyridostigmine | Minutes | 3-6 hours | Mild symptoms | $500-$1,000 | GI cramps, diarrhea |
| Prednisone | 1-4 weeks | Long-term | Initial control | $100-$500 | Weight gain, diabetes, osteoporosis |
| Azathioprine / Mycophenolate | 6-18 months | Long-term | Maintenance therapy | $500-$2,000 | Liver damage, GI issues |
| IVIG / Plasmapheresis | Days | Weeks | Crisis management | $10,000-$20,000 | Headache, infection risk |
| Complement inhibitors | 4-8 weeks | Indefinite | Severe AChR+ MG | $500,000-$600,000 | Meningitis risk (vaccine required) |
| FcRn inhibitors | 1-2 weeks | Weekly to monthly | All types, including seronegative | $300,000-$400,000 | Headache, infection |
| Rituximab | 8-16 weeks | 6-12 months | MuSK-MG, refractory cases | $10,000-$15,000 | Infusion reactions, low IgG |
| Thymectomy | 6-18 months | Years (remission) | AChR+, ages 18-65 | $20,000-$50,000 (one-time) | Surgical risks, persistent fatigue |
What Patients Are Really Saying
Behind the data are real people. A 2025 survey by the Myasthenia Gravis Foundation of America found that 78% of patients on FcRn inhibitors reported major improvement. Many prefer rozanolixizumab because it’s a weekly subcutaneous shot-no IV needed. But 45% deal with injection site reactions. On Reddit, users talk about the fight to get eculizumab approved. One wrote: “Took six months of appeals. I had to get a letter from my neurologist, three prior authorizations, and a letter from my insurance’s medical director. I was in a wheelchair during the wait.” Thymectomy patients often report feeling “like a new person” after a year-but 35% still struggle with fatigue. Cyclosporine? Many quit because of facial hair growth or high blood pressure. Long-term prednisone? 55% say it ruined their quality of life.
How Treatment Is Chosen: A Practical Path
There’s no single algorithm, but here’s what most neurologists follow:- Start with pyridostigmine. Add prednisone if symptoms persist.
- At 3-6 months, add azathioprine or mycophenolate if you’re not in minimal manifestation status.
- For severe disease, early-onset, or thymoma, plan thymectomy within 6-12 months.
- If you don’t respond to two immunosuppressants-or if you have a crisis-move to a biologic.
- For MuSK-MG, consider rituximab after steroids.
- For seronegative MG, FcRn inhibitors are now first-line biologics.
Terri Gladden
January 4, 2026 AT 01:44Jennifer Glass
January 4, 2026 AT 15:19Joseph Snow
January 5, 2026 AT 23:14Akshaya Gandra _ Student - EastCaryMS
January 6, 2026 AT 00:05en Max
January 6, 2026 AT 00:17Angie Rehe
January 6, 2026 AT 15:07Jacob Milano
January 7, 2026 AT 02:37saurabh singh
January 7, 2026 AT 06:21