Legionnaire's Disease Risks in Dental Offices - Essential Guide
 Oct, 17 2025
Oct, 17 2025
Dental Water Temperature Checker
Water Temperature Safety Calculator
Check if your dental unit water temperature meets CDC/ADA safety guidelines for Legionella prevention.
When you sit in a dental chair, you probably think about clean instruments and bright lights, not airborne bacteria. Yet a stealthy microbe called Legionella can turn a routine visit into a serious health risk.
Key Takeaways
- Legionella thrives in warm, stagnant water - a common condition in dental unit waterlines.
- Both patients and staff can inhale contaminated aerosols generated by handpieces and ultrasonic scalers.
- Regular water testing, disinfection, and temperature control are the backbone of prevention.
- CDC and ADA guidelines provide clear, actionable steps for dental practices.
- If an outbreak is suspected, swift investigation and communication are critical.
What Is Legionnaire's Disease?
Legionnaire's disease is a severe form of pneumonia caused by inhaling waterborne bacteria of the species Legionella pneumophila. The illness was first identified after a 1976 conference of the American Legion, which is how it got its name. Symptoms typically appear 2‑10 days after exposure and include high fever, chills, cough, and muscle aches. Without prompt treatment, mortality can reach 10‑15%, especially in older adults or those with weakened immune systems.
How Does Legionella Spread in Dental Settings?
Legionella loves warm, moist environments. In a dental office, the culprits are often:
- Dental unit waterlines (DUWLs) that deliver water to handpieces, scalers, and syringes.
- Ultrasonic scalers and high‑speed handpieces that create fine aerosols during procedures.
- Stagnant water in sink basins, storage tanks, or decorative fountains.
When these devices are used, the aerosol can travel up to three feet from the mouth, making it easy for the bacteria to be inhaled by patients or clinicians.
Dental Facilities - Why They Are a Unique Risk Zone
Dental facilities are designed for precision, yet their water systems can unintentionally become breeding grounds for Legionella. The constant flow of water through narrow tubing, combined with intermittent use, creates perfect conditions for biofilm formation. Once a biofilm establishes, it protects Legionella from standard cleaning, allowing the bacteria to multiply.
Regulatory Guidance: CDC and ADA Recommendations
The Centers for Disease Control and Prevention (CDC) and the American Dental Association (ADA) have issued joint recommendations. Key points include:
- Test water monthly for Legionella spp. and total bacterial counts.
- Maintain waterline temperature above 20°C (68°F) and below 50°C (122°F) to discourage growth.
- Use chemical disinfectants (e.g., hydrogen peroxide, chlorhexidine) after each patient.
- Implement point‑of‑use filters on handpieces and ultrasonic scalers.
- Document all maintenance activities in a logbook.
Practical Prevention Strategies
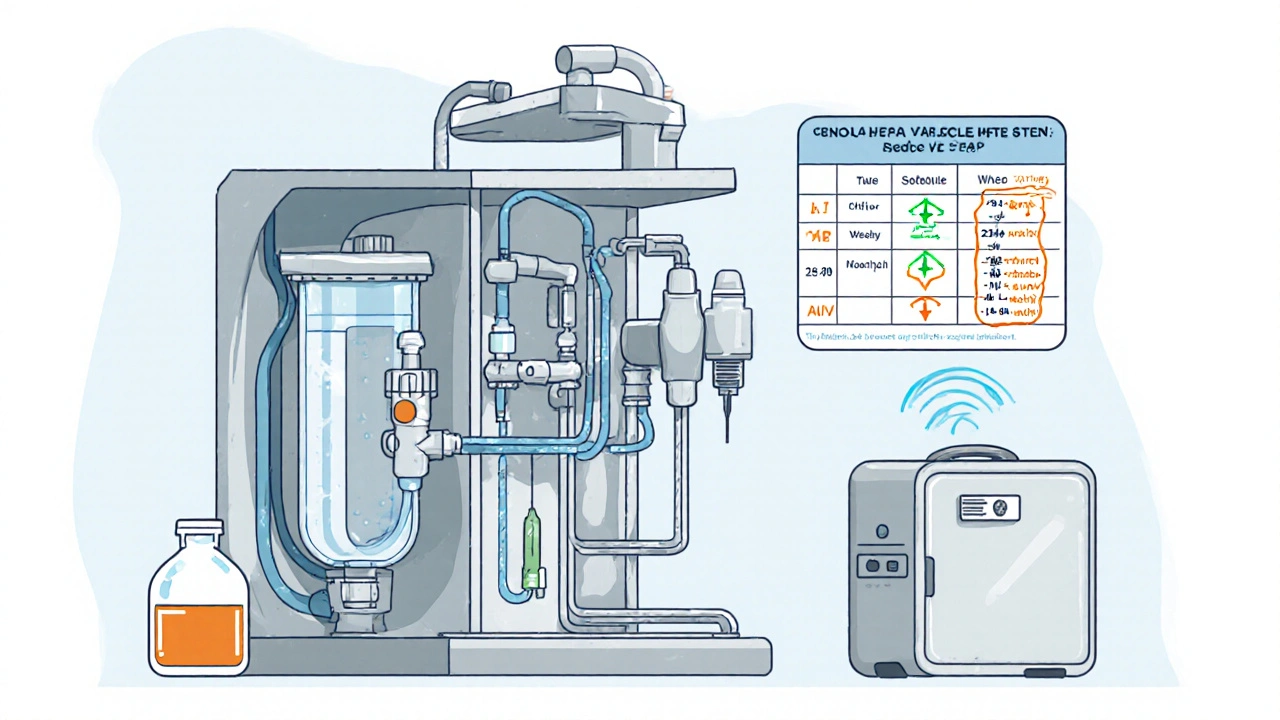
Below is a checklist most dental offices can adopt without major capital expense.
- Daily Flushing: Run water through each line for at least 2 minutes at the start of the day.
- Periodic Hyperchlorination: Treat the system with a 0.2% chlorine solution weekly, then flush thoroughly.
- Temperature Control: Install thermostatic valves to keep water within the safe range.
- HEPA Filtration: Place portable HEPA units near operatory chairs to capture lingering aerosols.
- Routine Monitoring: Use a certified lab or in‑house PCR kit to detect Legionella pneumophila in water samples.
What To Do If an Outbreak Is Suspected
Speed matters. Follow these steps:
- Notify Public Health Authorities: Report cases to the local health department immediately.
- Stop All Non‑Emergency Procedures: Prevent further aerosol generation.
- Conduct a Full System Flush: Use high‑dose disinfectant and replace water storage tanks if needed.
- Review Maintenance Logs: Identify gaps in testing or disinfection.
- Communicate With Patients: Offer testing and information about potential exposure.

Case Snapshot: A Small Practice’s Close Call
In 2023, a dental office in Ohio detected Legionella in its waterlines after a patient was hospitalized with pneumonia. The clinic had been using a low‑dose disinfectant but failed to test monthly. After a rapid hyperchlorination cycle and installing point‑of‑use filters, the practice cleared the contamination within two weeks and resumed normal operations. The incident underscored the value of consistent testing and documentation.
Quick Reference Checklist
| Task | Frequency | Responsible Person |
|---|---|---|
| Waterline flush (all units) | Daily (start of day) | Assistant |
| Disinfectant treatment | Weekly | Hygiene coordinator |
| Water sample testing | Monthly | Lab technician |
| Filter replacement | Every 6months | Equipment manager |
| Logbook audit | Quarterly | Practice manager |
Frequently Asked Questions
Can regular dental cleanings transmit Legionella?
Yes, if the waterlines are contaminated and the cleaning uses ultrasonic scalers that create aerosols. Proper disinfection and testing eliminate this risk.
How long does Legionella survive in dental waterlines?
The bacteria can persist for weeks to months in biofilm if waterlines are not regularly flushed or disinfected.
Are point‑of‑use filters enough on their own?
Filters are a strong barrier, but they must be combined with routine cleaning and temperature control for full protection.
What temperature range stops Legionella growth?
Keeping water between 20°C (68°F) and 50°C (122°F) reduces the chance of bacterial multiplication.
If I develop pneumonia after a dental visit, should I mention Legionella?
Absolutely. Inform your physician about the recent dental work so they can order the appropriate Legionella test.
Understanding Legionnaire's disease is crucial for anyone visiting a dental office. By staying informed and following the guidelines above, patients and dental teams can keep the risk low and focus on what matters most - healthy smiles.
alex montana
October 17, 2025 AT 19:26Wow!! This makes me think about the hidden microbes lurking in every faucet!!!
Wyatt Schwindt
October 19, 2025 AT 00:03The guide highlights daily flushing and weekly disinfection as key steps.
Lyle Mills
October 19, 2025 AT 01:26Implementing a systematic waterline maintenance protocol-incorporating biofilm mitigation, PCR surveillance, and point‑of‑use filtration-optimizes microbial control.
Barbara Grzegorzewska
October 19, 2025 AT 02:50Ugh, honestly, if you’re still using “old‑school” chlorhexidine without a proper logbook, you’re basically inviting Legionella to throw a party in your handpieces-so get with the program, lol.
Nis Hansen
October 19, 2025 AT 04:13Legionella in dental waterlines is more than a technical hiccup; it challenges our collective responsibility to safeguard health.
When we think about infection control, the mind wanders to sterilized instruments, yet the invisible water streams can harbor danger.
Every daily flush is a ritual of prevention, a small act that carries massive impact.
Weekly hyper‑chlorination serves as a chemical reset, disrupting biofilm resilience.
Temperature control is not a luxury but a scientific necessity, keeping water out of the microbial sweet spot.
Point‑of‑use filters act like guardians at the gate of each handpiece, catching what the waterline cannot eradicate.
HEPA filtration in the operatory air adds a protective veil against aerosolized particles.
Documentation, often overlooked, becomes the evidence of vigilance and the tool for continuous improvement.
Regular PCR testing offers precise detection, allowing swift corrective action before an outbreak escalates.
Leadership must champion these protocols, turning guidelines into daily habits rather than quarterly checks.
Staff education empowers dental teams to recognize early signs of contamination and respond confidently.
Patient communication builds trust; informing them of safety measures reassures and educates simultaneously.
In the event of a suspected case, immediate cessation of non‑essential procedures minimizes further exposure.
Rapid coordination with public health authorities ensures transparency and resource mobilization.
Finally, a culture of proactive maintenance transforms a potential crisis into a model of excellence for the entire healthcare community.
Fabian Märkl
October 19, 2025 AT 05:36Great reminder! 👍 Keeping those waterlines clean not only protects patients but also boosts staff confidence 😊
Avril Harrison
October 19, 2025 AT 07:00It’s wild how something as simple as a faucet can become a health hazard if ignored.
Nhasala Joshi
October 19, 2025 AT 08:23Did you know that some “official” guidelines might actually downplay the true risk, letting big water‑filter manufacturers profit while patients suffer? 😡💧
Grace Hada
October 19, 2025 AT 09:46Stop overlooking water testing; it’s non‑negotiable.
nitish sharma
October 19, 2025 AT 11:10It is imperative that dental practices adhere to the recommended monthly testing schedule, thereby ensuring both patient safety and regulatory compliance.
Rohit Sridhar
October 19, 2025 AT 12:33Staying ahead of Legionella is totally doable! Regular flushing, combined with periodic hyper‑chlorination, creates a hostile environment for the bacteria. Adding HEPA filters adds another layer of protection, especially during aerosol‑heavy procedures. Keep the momentum, and your clinic will set a benchmark for infection control.
Sarah Hanson
October 19, 2025 AT 13:56We should all document each disinfectant cycle; a tidy logbook is key for audits.
kendra mukhia
October 19, 2025 AT 15:20Seriously, if you think a quick rinse is enough, you’re living in the Dark Ages-modern dentistry demands rigorous protocols, not half‑measures.
Bethany Torkelson
October 19, 2025 AT 16:43Enough with the complacency; enforce strict waterline standards now!