Insurance Coverage of Authorized Generics: How Formulary Placement Affects Costs and Access
 Nov, 27 2025
Nov, 27 2025
When you fill a prescription for a brand-name drug like Protonix or Ocella, you might be surprised to get a pill that looks different but works exactly the same. That’s an authorized generic-a version of the brand drug made by the same company, sold under a different label, and priced like a regular generic. For insurers, this isn’t just a cost-saving trick; it’s a strategic tool to control spending without risking patient outcomes. But getting it covered isn’t automatic. Formulary placement decides whether your insurance will pay for it at the same low cost as a traditional generic-or if you’ll be stuck paying brand prices.
What Exactly Is an Authorized Generic?
An authorized generic isn’t a knockoff. It’s the exact same drug, made in the same factory, with the same active ingredients, same fillers, same everything. The only difference? No brand name on the bottle. You’re getting Pfizer’s Protonix, but labeled as “pantoprazole sodium” with a different color and shape. The FDA allows this under the original New Drug Application (NDA), meaning it skips the usual generic approval process. That’s why it’s not listed in the Orange Book with other generics-it’s not a separate product. It’s the brand drug wearing a disguise. This matters because traditional generics have to prove they’re bioequivalent. Authorized generics don’t. They’re already proven. That makes them safer for patients with narrow therapeutic windows-like those on thyroid meds, seizure drugs, or blood thinners-where even tiny differences can cause problems. For insurers, that means less risk of adverse events, fewer doctor visits, and lower overall costs.Why Formulary Placement Matters
Formularies are insurance companies’ lists of covered drugs, grouped into tiers. Tier 1 is cheapest (usually basic generics), Tier 2 is mid-range, Tier 3 and 4 are brand-name or specialty drugs. Where a drug lands determines your copay. If your insurer puts an authorized generic on Tier 3, you pay $50. If it’s on Tier 1, you pay $10. The difference isn’t just money-it’s whether you can afford to keep taking your medication. Here’s the reality: 87% of Medicare Part D plans treat authorized generics the same as traditional generics, placing them in Tier 1 or 2. But 12% still treat them like brand drugs. Why? Some PBMs don’t have the right codes in their systems. Others are slow to update. And a few, intentionally or not, keep them on higher tiers to protect brand revenue streams. A 2022 study of 1,247 Medicare plans found that those with clear policies for authorized generics saved 7.3% per member per month on prescriptions. That’s not a small number. For a plan with 100,000 members, that’s tens of millions in savings over a year.Authorized Generics vs. Traditional Generics: The Real Difference
Many people think all generics are the same. They’re not. Traditional generics are made by different companies. They have to go through ANDA approval. They might use different fillers or coatings. That’s why some patients report feeling different after switching-even if the active ingredient is identical. Authorized generics don’t have that issue. They’re identical from the inside out. For insurers, this means fewer complaints, fewer claims for side effects, and fewer appeals. But here’s the catch: authorized generics aren’t available for most drugs. Only about 15-20% of brand-name medications have an authorized version. That’s why you might see one for Synthroid but not for your asthma inhaler. The manufacturers who make the most authorized generics? Greenstone (Pfizer), Prasco, and Patriot Pharmaceuticals. Together, they control 63% of the market. That’s not competition-it’s a controlled rollout. And that’s why some experts warn they’re used to delay true generic competition. In 22% of cases studied, the arrival of an authorized generic slowed down other generic entrants.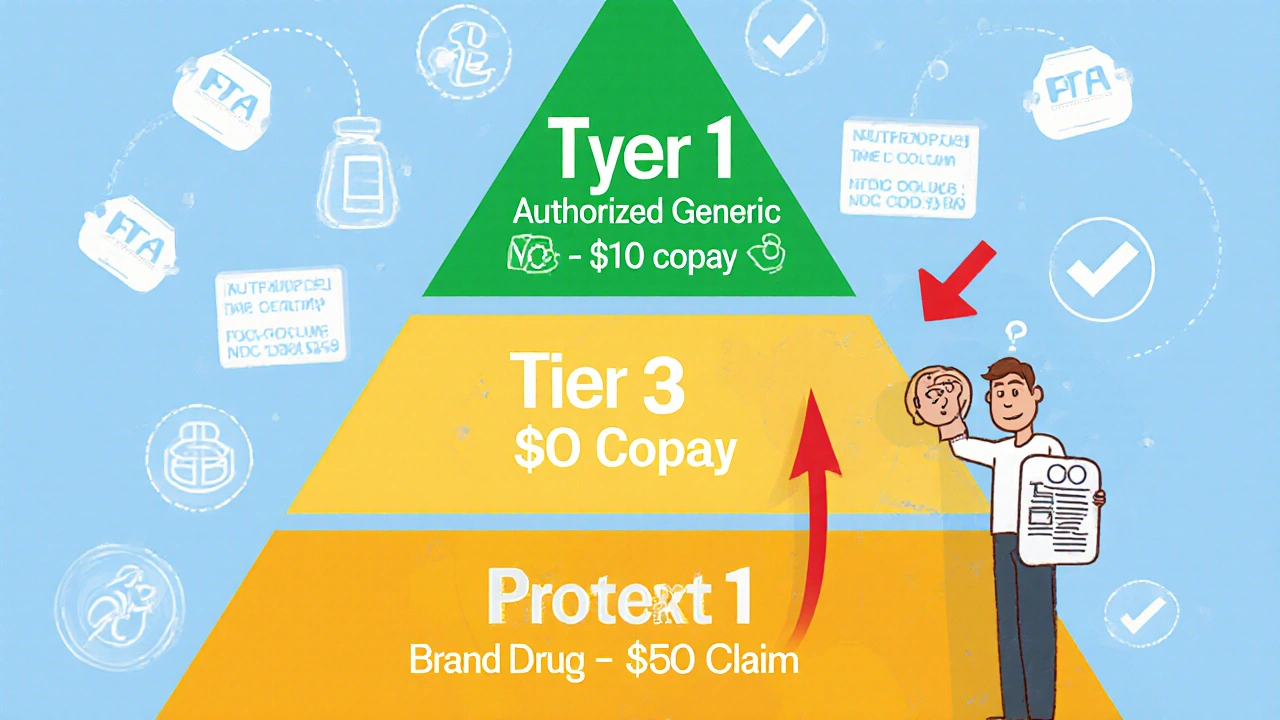
How Insurers Handle Coverage
Most large insurers and PBMs now have systems to track authorized generics. CVS Caremark, Express Scripts, and OptumRx all updated their formulary databases between 2022 and 2023. OptumRx even launched an “Authorized Generic First” policy for 47 high-cost drugs in early 2023. That means if an authorized generic exists, it’s the default covered option. But implementation isn’t perfect. Walgreens reported a 12% error rate in processing authorized generic claims before they added special verification steps. Why? Because these drugs don’t show up in standard generic databases. Pharmacists need to cross-check the FDA’s official list-currently 147 products as of October 2023-and match NDC codes manually. If they don’t, the claim gets denied. That’s where patients get stuck. A 2022 GoodRx survey found 34% of people were confused when their pharmacy switched them to an authorized generic without warning. 18% had claims denied because the system didn’t recognize the drug as covered. One Reddit user shared: “My insurance denied Synthroid brand, but approved the authorized generic with a $10 copay. Took three calls to get them to fix it.”What You Can Do as a Patient
You don’t have to wait for your insurer to catch up. Here’s how to take control:- Ask your pharmacist: “Is there an authorized generic for this drug?”
- Check the FDA’s official list of authorized generics-available online for free.
- If your claim is denied, ask for a manual override using the NDC code from the bottle.
- Call your insurer’s pharmacy line and ask: “Is this authorized generic covered at the generic tier?”
- If you’re on a high-cost drug like Ocella or Yasmin, ask your doctor to write “Dispense as Written” or “Do Not Substitute” if you’ve had bad reactions to other versions.

Jake Ruhl
November 27, 2025 AT 20:29so like... are we just letting big pharma play us like pawns? authorized generics? more like authorized manipulation. they make the exact same pill but slap a new label on it and suddenly it's 'cheaper'-but only if your insurer feels nice that day. meanwhile, the company that made Protonix is still raking in billions. they're not saving you money, they're just hiding the price hike in plain sight. and don't get me started on how they use these to block real generics. it's not healthcare-it's corporate theater with a side of hives.
Chuckie Parker
November 29, 2025 AT 08:52Stop the drama. Authorized generics are FDA approved identical copies. They're not a loophole. They're a feature. If your plan covers them at generic tier you're getting the same drug for less. That's not conspiracy that's capitalism working. Stop crying about Big Pharma and start using your pharmacy benefit correctly.
George Hook
November 30, 2025 AT 03:29I've been on Synthroid for over a decade and switched to the authorized generic after my insurer pushed it. No side effects no weird reactions no anxiety about whether the pill was 'right'. I think people underestimate how much the inactive ingredients matter. I used to break out in rashes with every generic switch. The authorized version? Zero issues. It's not magic. It's just consistency. And honestly if your insurer doesn't cover it at Tier 1 you should call them. They're not doing their job.
Katrina Sofiya
November 30, 2025 AT 12:21Thank you for writing this with such clarity and care. This is exactly the kind of information patients need but rarely receive. Many people feel powerless when it comes to prescription costs-but knowing that authorized generics exist and how to advocate for them is truly empowering. I encourage everyone reading this to ask their pharmacist about their medication's origin. Knowledge is not just power-it's peace of mind. Keep sharing these insights.
kaushik dutta
December 1, 2025 AT 10:50Interesting how the U.S. system allows this regulatory arbitrage while countries like India and Germany have transparent generic pricing models. Here we have a two-tiered system where the same molecule is priced differently based on label color. The PBM oligopoly is the real villain. They control formulary placement, NDC coding, and rebate structures-all while pretending to be cost-saving intermediaries. This isn't innovation. It's rent extraction disguised as efficiency. The FDA needs to mandate unified coding for authorized generics across all systems. Otherwise we're just gaming the game.
doug schlenker
December 1, 2025 AT 22:07I appreciate how you broke this down. I had no idea authorized generics existed until my pharmacist mentioned it last month. I was confused because the pill looked different but the name was the same. I called my insurer and they said it was covered at $10. I was skeptical at first but after two weeks I felt exactly the same. No side effects no weirdness. Honestly I think more people should know this. It’s not just about saving money-it’s about stability. If your body reacts to fillers or dyes this could be a game changer.
Olivia Gracelynn Starsmith
December 3, 2025 AT 15:38For those confused about why their claim got denied-check the NDC code on the bottle. That’s the key. Most pharmacy systems still don’t auto-recognize authorized generics because they’re not in the standard generic database. I work in billing and we had to manually update 400+ drug codes last year. If your claim gets denied ask for a manual override using the exact NDC. It works. Also ask your doctor to write DAW 1 if you’ve had bad reactions. It’s not a big ask but it saves lives.
Skye Hamilton
December 4, 2025 AT 11:41soooo... the real question is who benefits from this? not the patient. not the pharmacist. definitely not the doctor. it’s the insurance company and the pharma giant who secretly own both the brand and the ‘generic’. it’s like they made a clone of their own product just to trick you into thinking you’re getting a deal. and the FDA lets them? i mean... what even is regulation anymore? i’m not mad. i’m just disappointed.
Maria Romina Aguilar
December 5, 2025 AT 05:28It’s worth noting, however, that-despite the apparent benefits-there is still no standardized labeling protocol for authorized generics, which leads to inconsistent patient education, and, in some cases, confusion among pharmacists who are not trained to distinguish between true generics and authorized generics; furthermore, the FDA’s list, while publicly accessible, is not integrated into most EHR systems, which creates a systemic gap in care coordination, and, if you’re not a medical professional or a policy wonk, you’re likely unaware of this, which is, frankly, alarming.
Brandon Trevino
December 6, 2025 AT 04:00Let’s cut through the fluff. The 15-20% market penetration of authorized generics isn’t accidental. It’s engineered. The top three manufacturers control 63% of the market. That’s not competition. That’s collusion disguised as compliance. The FTC should be investigating this as an anti-competitive tactic. When a brand manufacturer releases an authorized generic to delay true generic entry, they’re not lowering prices-they’re rigging the market. And the fact that PBMs still don’t have updated coding systems? That’s not incompetence. That’s complicity. This isn’t healthcare innovation. It’s regulatory capture with a side of placebo pricing.
Denise Wiley
December 7, 2025 AT 02:46Just had my first experience with an authorized generic for Ocella. I was terrified I’d get the same mood swings I had with the other generic. But the pill looked different and the pharmacy said it was the same stuff. I took it. No issues. No drama. My anxiety went down. I actually felt… normal. I wish I’d known this sooner. Seriously, if you’re on a med that’s causing weird side effects, ask your pharmacist. It might not be the drug-it might be the filler. And if your insurance denies it? Don’t give up. Call them. Keep calling. You’ve got a right to the best version of your medicine.