Hydrophilic vs Lipophilic Statins: What You Need to Know About Side Effects
 Jan, 26 2026
Jan, 26 2026
Statins Side Effect Risk Calculator
Personal Risk Assessment
Answer the questions below to get personalized recommendations for your statin treatment.
When doctors prescribe statins, they don’t just pick a name off a list. The chemical makeup of the drug - whether it’s hydrophilic or lipophilic - can make a real difference in how your body reacts. You might not hear this talked about in the waiting room, but it matters. Especially if you’ve ever felt unexplained muscle soreness, fatigue, or brain fog after starting a statin. The difference between water-loving and fat-loving statins isn’t just chemistry class trivia. It’s a practical tool for avoiding side effects without giving up heart protection.
What Does Hydrophilic vs Lipophilic Even Mean?
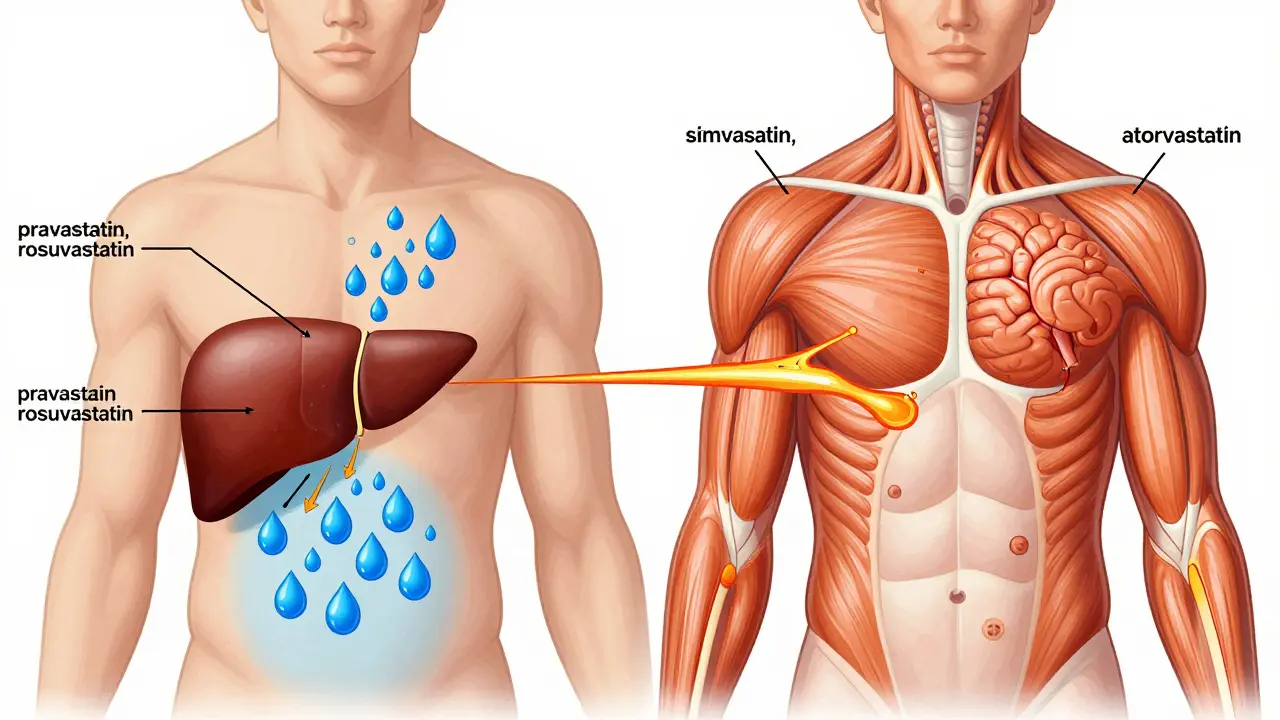
Think of your body like a house. Some drugs are like water - they stay mostly in the bloodstream and can’t easily slip through walls. These are hydrophilic statins. Others are like oil - they slip right through cell membranes and go everywhere. Those are lipophilic statins. Lipophilic statins - like simvastatin, atorvastatin, lovastatin, fluvastatin, and pitavastatin - dissolve in fat. That lets them passively drift into muscle tissue, the brain, and other organs. Hydrophilic statins - pravastatin and rosuvastatin - need special doors (called OATP transporters) to get into cells. Those doors are mostly in the liver. So these drugs stay put, doing their job lowering cholesterol where it counts, and avoiding places they shouldn’t. This isn’t just theory. Studies show lipophilic statins reach 3 to 5 times higher concentrations in muscle tissue than hydrophilic ones. That’s why, for years, doctors assumed lipophilic statins caused more muscle problems. But the real world doesn’t always follow the theory.Do Lipophilic Statins Cause More Muscle Pain?
It’s tempting to say yes. After all, if a drug gets into your muscles more easily, shouldn’t it cause more damage? Many patients report exactly that. On patient forums, people say they had no issues with pravastatin, then switched to simvastatin and suddenly couldn’t climb stairs without aching. One Reddit thread with over 140 responses showed 78% of users linked muscle pain to lipophilic statins. But here’s the twist. A massive 2021 study of 15 million people in the UK found something surprising. When comparing rosuvastatin (hydrophilic) to atorvastatin (lipophilic), the hydrophilic drug actually had a slightly higher risk of muscle problems - 17% higher. Another comparison showed simvastatin (lipophilic) had a 33% higher risk than atorvastatin (also lipophilic), not hydrophilic ones. That’s not a typo. Hydrophilic statins aren’t automatically safer. Rosuvastatin, despite being water-soluble, is extremely potent. It’s designed to work hard in the liver, and that intensity might cause problems on its own. One patient on HealthUnlocked reported severe muscle pain on low-dose rosuvastatin, but zero issues on higher-dose simvastatin. Another switched from simvastatin to pravastatin - both were hydrophilic - and still had pain. That’s the reality: it’s not just about solubility. It’s about dose, genetics, age, and other meds.What About Other Side Effects?
Muscle pain gets all the attention, but it’s not the only thing to watch for. Lipophilic statins can cross the blood-brain barrier. That’s why some people report memory fuzziness, confusion, or even depression after starting simvastatin or atorvastatin. The FDA even added a warning about cognitive side effects in 2012. Hydrophilic statins? They mostly stay out of the brain. That’s a quiet advantage. Then there’s drug interactions. Lipophilic statins like simvastatin and atorvastatin are broken down by the liver enzyme CYP3A4. That means they clash with common drugs - grapefruit juice, certain antibiotics, antifungals, even some heart meds. A single interaction can spike statin levels and trigger muscle damage. Pravastatin and rosuvastatin barely use CYP3A4. That makes them safer if you’re on multiple medications. Kidney function matters too. If your kidneys are weak (eGFR under 60), hydrophilic statins are preferred. They’re cleared more safely through urine. Lipophilic statins can build up, increasing risk. One 2021 study found hydrophilic statins reduced major heart events by 31% more than lipophilic ones in patients with kidney disease.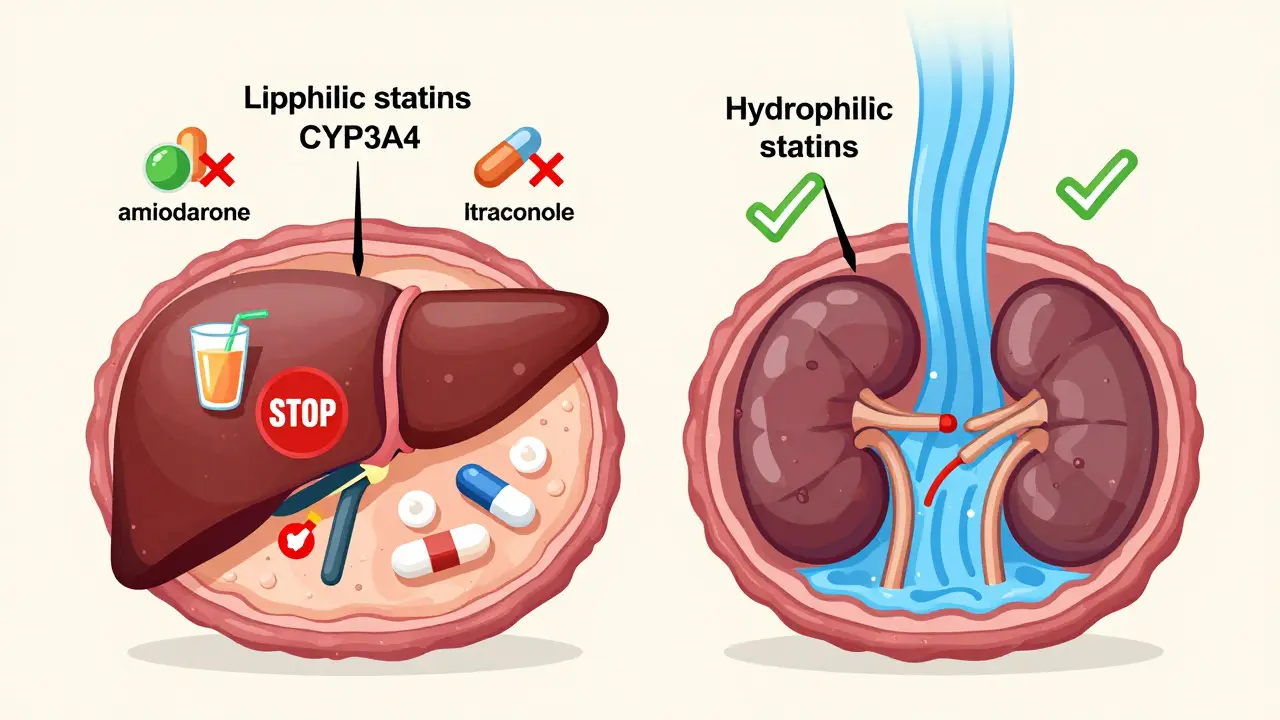
Who Should Switch - and When?
You don’t need to switch just because your statin is lipophilic. But if you’re experiencing muscle pain, fatigue, or brain fog - especially if you’re over 65, female, underweight, or on other meds - it’s worth talking to your doctor. Here’s what to consider:- If you’re on simvastatin and have muscle pain, try switching to pravastatin. Many people feel better.
- If you’re on rosuvastatin and have side effects, switching to pravastatin (both hydrophilic) might help - not because of solubility, but because rosuvastatin is stronger and more likely to cause issues at higher doses.
- If you’re on a lipophilic statin and take amiodarone, itraconazole, or other CYP3A4 blockers, switching to pravastatin or rosuvastatin cuts interaction risk dramatically.
- If you have kidney disease, hydrophilic statins are the safer bet.
What About Effectiveness?
A lot of people worry: if I switch to a hydrophilic statin, will it still work? Yes - but potency varies. Rosuvastatin at 20 mg lowers LDL by 52%. Pravastatin at the same dose? Only 34%. So if you need aggressive cholesterol control, rosuvastatin wins. But if you’re on a low dose and just need to stay in range, pravastatin might be enough - and gentler. Lipophilic statins like atorvastatin and simvastatin are more potent than pravastatin. That’s why they dominate prescriptions. But potency isn’t always better. Sometimes, less is more - especially if you’re sensitive.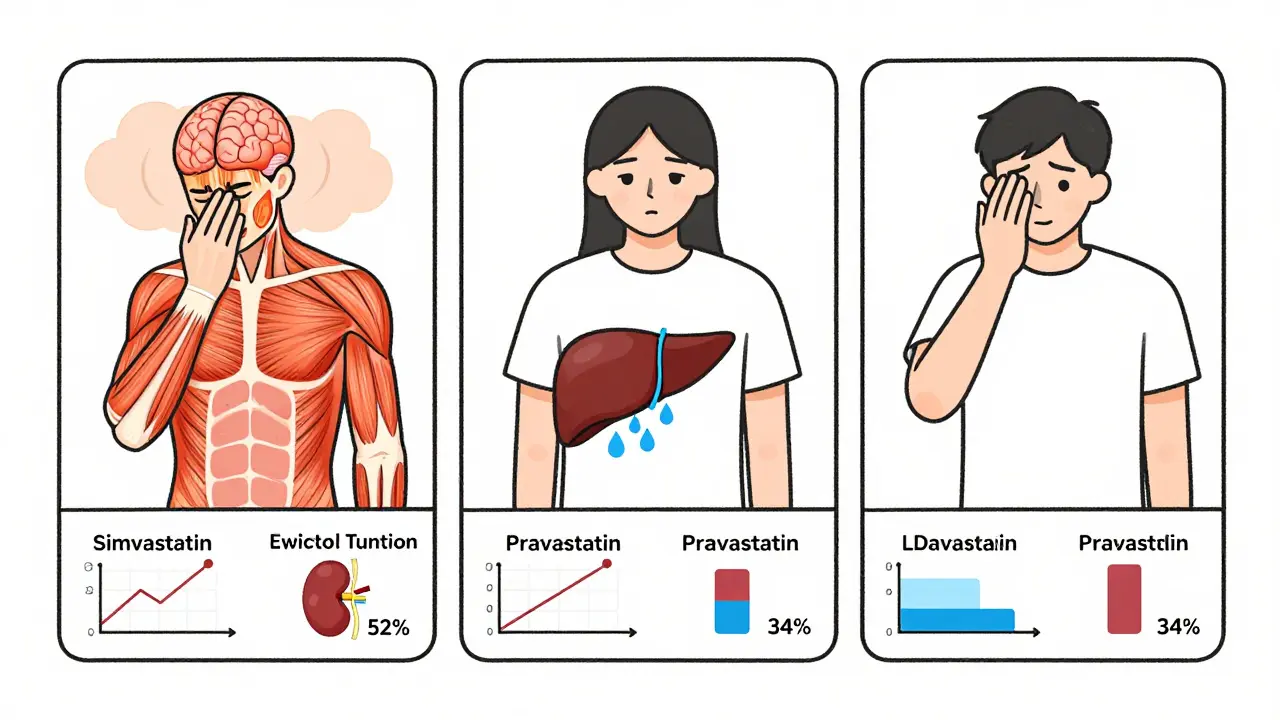
What’s the Bottom Line?
The old rule - hydrophilic statins are safer - is outdated. The truth is messier. Lipophilic statins aren’t automatically dangerous. Hydrophilic ones aren’t magic bullets. The best choice depends on your body, your meds, your kidney health, and your symptoms. Here’s what to do:- If you’re starting a statin and have risk factors (age, low weight, other meds), ask for pravastatin or rosuvastatin first.
- If you’re already on a statin and have muscle pain, don’t just quit. Talk to your doctor about switching - even within the same group. Try pravastatin instead of rosuvastatin, or vice versa.
- If you’re on a lipophilic statin and take grapefruit juice, antibiotics, or heart meds, switch to a hydrophilic one to avoid dangerous interactions.
- Don’t fear hydrophilic statins because they’re "weaker." Rosuvastatin is one of the strongest statins on the market.
What’s Next?
The future of statins isn’t about lipophilicity. It’s about genetics. Researchers are already testing polygenic risk scores to predict who’ll respond to which statin - and who’s likely to have side effects. By 2025, your DNA might tell your doctor which statin to pick, not your liver’s solubility rules. For now, though, the best advice is simple: pay attention to how your body feels. Track your symptoms. Don’t accept muscle pain as "normal." And know that switching statins isn’t failure - it’s smart management.Are hydrophilic statins always safer than lipophilic ones?
No. While hydrophilic statins like pravastatin and rosuvastatin are more liver-focused and have fewer drug interactions, they’re not automatically safer. Rosuvastatin, despite being hydrophilic, has been linked to muscle pain in some patients at higher doses. Studies show the risk of muscle side effects isn’t consistently lower with hydrophilic statins - it depends on the individual, the dose, and other health factors.
Can statins cause memory problems?
Yes, especially lipophilic statins like simvastatin and atorvastatin. Because they dissolve in fat, they can cross the blood-brain barrier and may affect brain function in some people. Symptoms like brain fog, forgetfulness, or confusion are rare but real. Hydrophilic statins like pravastatin and rosuvastatin are less likely to enter the brain, making them a better choice if cognitive side effects are a concern.
Should I switch statins if I have muscle pain?
It’s worth trying. About 57% of patients who switched from lipophilic to hydrophilic statins reported improved muscle symptoms. But switching within the same group can help too - for example, going from rosuvastatin to pravastatin (both hydrophilic) might reduce side effects if the issue is dose intensity, not solubility. Always consult your doctor before switching - never stop statins abruptly.
Do hydrophilic statins work as well as lipophilic ones?
It depends on the drug. Rosuvastatin (hydrophilic) is one of the most potent statins available, lowering LDL by up to 52% at 20 mg. Pravastatin (also hydrophilic) is less potent, lowering LDL by about 34% at the same dose. Lipophilic statins like atorvastatin and simvastatin are generally more potent than pravastatin but similar to rosuvastatin. Effectiveness isn’t tied to solubility - it’s tied to the specific drug and dose.
Can I take grapefruit juice with any statin?
Only with hydrophilic statins like pravastatin and rosuvastatin. Grapefruit juice blocks the CYP3A4 enzyme, which breaks down lipophilic statins like simvastatin and atorvastatin. This can cause dangerous buildup in your blood, increasing muscle damage risk. Even a small amount of grapefruit juice can have this effect. If you like grapefruit, stick to pravastatin or rosuvastatin.
Is kidney disease a reason to choose a hydrophilic statin?
Yes. Hydrophilic statins are cleared more safely through the kidneys. For patients with reduced kidney function (eGFR under 60), hydrophilic statins like pravastatin and rosuvastatin are preferred because they reduce major heart events by 31% more than lipophilic statins in this group. Lipophilic statins can accumulate and raise side effect risks when kidneys aren’t working well.
Kipper Pickens
January 27, 2026 AT 22:07The hydrophilic/lipophilic dichotomy is fascinating from a pharmacokinetic standpoint, but clinically, it’s just one variable in a multivariate equation. OATP1B1 polymorphisms, CYP isoform expression, mitochondrial toxicity thresholds - these matter more than solubility coefficients in isolation. Rosuvastatin’s potency isn’t just about being water-soluble; it’s about high-affinity binding to HMG-CoA reductase and minimal first-pass metabolism. The 2021 UK study’s 17% higher muscle risk for rosuvastatin? Probably reflects its dose-dependent saturation of hepatic uptake transporters, not membrane permeability. Lipophilicity is a red herring if you’re not accounting for transporter genetics.
Also, the grapefruit interaction isn’t just about CYP3A4 inhibition - it’s about furanocoumarins irreversibly inactivating the enzyme. That’s why even a single glass can have 72-hour effects. Pravastatin’s renal clearance makes it the only statin where you can safely drink grapefruit juice if you’re on polypharmacy. Just don’t tell your cardiologist I said that.
Aurelie L.
January 28, 2026 AT 01:26I switched from atorvastatin to pravastatin and my brain fog vanished. No joke. It was like someone turned the lights back on.
Now I just feel tired all the time. Maybe it’s the statin. Maybe it’s life.