How to Verify the Prescriber and Pharmacy Information on Your Medication Label
 Dec, 25 2025
Dec, 25 2025
Why Checking Your Medication Label Matters More Than You Think
Every year, over 1.3 million people in the U.S. are injured because of medication errors. About 12% of those errors happen because the prescriber or pharmacy info on the label doesn’t match what it should. That’s not a small risk-it’s a preventable one. Your medication label isn’t just a piece of paper with instructions. It’s your first and most reliable line of defense against getting the wrong drug, the wrong dose, or a drug that shouldn’t be taken with something else you’re on.
Many people assume if the pill looks right and the instructions seem clear, everything’s fine. But that’s where things go wrong. A 2023 study found that 68% of patients who actually checked their labels caught an error they didn’t even know was there. One person noticed the prescriber’s name was misspelled. Another saw the pharmacy listed was different from the one they used. Both cases prevented serious harm.
What You Need to Look for on Every Label
Before you even open the bottle, pause. Take 30 to 60 seconds. Look at the label like you’re reading a receipt for something expensive-because it is. Your life depends on it.
Here’s what must be clearly printed:
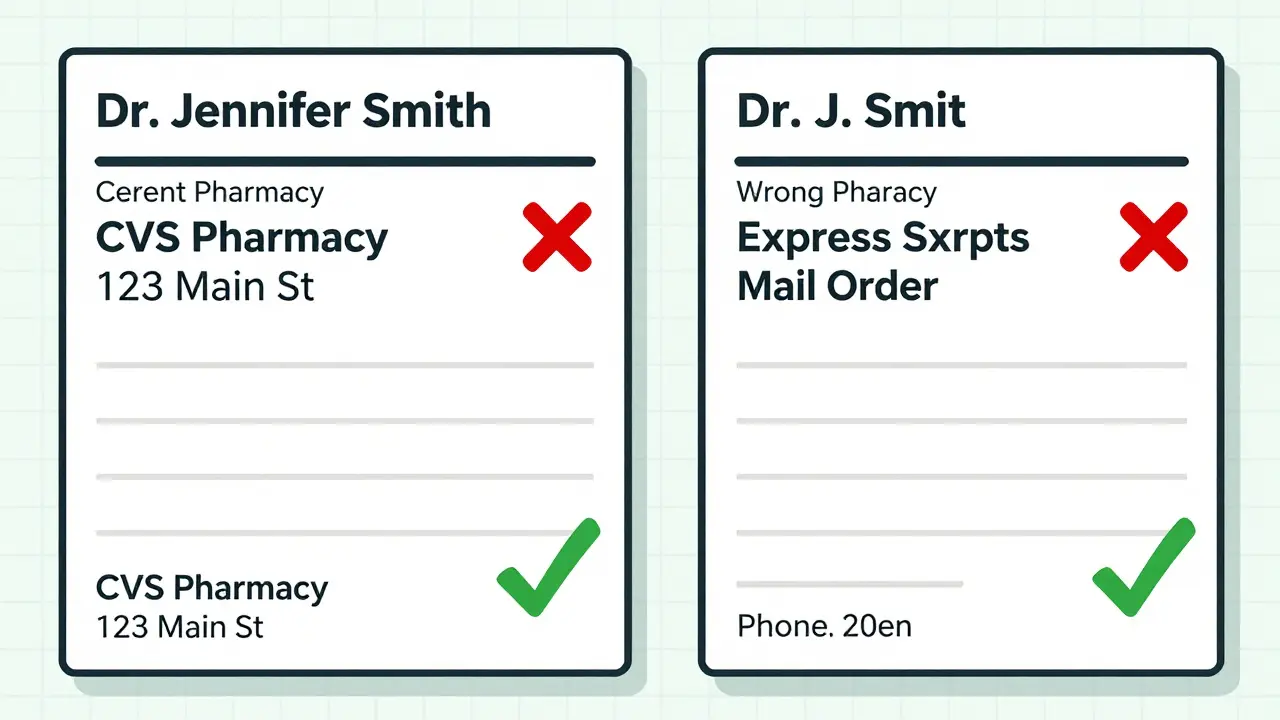
- Prescriber’s full name - This should match exactly who you saw. Not “Dr. J. Smith” if your doctor is “Dr. Jennifer Smith.”
- National Provider Identifier (NPI) - A 10-digit number assigned to every licensed provider. It’s not always visible on small labels, but if it’s there, cross-check it with your provider’s info.
- Pharmacy name and address - Should be the exact legal name of the pharmacy. Not “CVS Pharmacy” if you picked it up at “CVS on 5th.”
- Pharmacy phone number - This is your direct line to a pharmacist. If it’s missing, that’s a red flag.
- Prescription number - Usually starts with a letter and ends in numbers. Use this when calling for refills.
- Pharmacist’s name - Required in 42 states. If you’re unsure, ask the pharmacist to confirm they filled it.
These aren’t suggestions. They’re federal and state requirements. If any of these are missing, blurred, or wrong, don’t take the medication. Call the pharmacy right away.
How to Spot the Most Common Errors
Most mistakes aren’t random. They follow patterns. Knowing them helps you catch them fast.
Misspelled prescriber names - This is the #1 issue. A dentist’s name printed as “Dr. J. Brown” when it should be “Dr. James Brown.” A typo like “Dr. Smit” instead of “Dr. Smith.” These aren’t just clerical errors-they mean the wrong provider’s prescription was filled.
Wrong prescriber specialty - You saw your cardiologist for high blood pressure, but the label says “prescribed by Dr. Lisa Chen, Dermatologist.” That’s not just odd-it’s dangerous. Dermatologists don’t prescribe heart meds without coordination.
Electronic prescription glitches - About 18% of label errors come from e-prescribing systems auto-filling the wrong provider. If your doctor switched clinics or retired, the system might still send it to their old address.
Mail-order mix-ups - Mail-order pharmacies have a 23% higher error rate than local ones. They handle more complex meds, and labels sometimes get mixed up in bulk processing. If you get a new bottle from your mail-order pharmacy, compare it to your last one.
One real case from 2023: A patient got a Schedule II opioid prescribed by a dentist-but the label listed their primary care doctor. The patient noticed the mismatch, called the pharmacy, and found out someone else’s prescription had been filled for them. That’s not a rare glitch. It’s a system failure you can stop.
When to Check Your Label (It’s Not Just Once)
Don’t wait until you’re ready to take your pill. Check it three times:
- When you pick it up - Right at the counter. Don’t let the pharmacy rush you. Ask: “Can you confirm the prescriber and pharmacy info?”
- Before your first dose - Even if you’ve taken this drug before, the prescriber or pharmacy might have changed. Always double-check.
- When you refill - If the label looks different from last time, pause. Is the pharmacy name the same? Is the prescriber spelled the same? If not, call before you take it.
Studies show people who check at all three points reduce their risk of medication errors by 32%. That’s not magic. It’s attention.
What to Do If Something’s Wrong
If you spot a mistake, don’t guess. Don’t assume it’s “just a typo.”
Call the pharmacy immediately using the number on the label. Say: “I’m checking my prescription. The prescriber listed here doesn’t match who I saw. Can you confirm this was filled correctly?”
Most pharmacies will recheck the original e-prescription and fix it on the spot. If they say it’s “correct” but you still feel off, ask to speak to the pharmacist on duty-not just the technician. Pharmacists are trained to catch these issues. They’re your ally.
If the pharmacy won’t fix it or brushes you off, call your prescriber’s office. Ask them to confirm they sent the prescription to that pharmacy. If needed, go to another pharmacy. You have the right to a safe, accurate prescription.
Tools That Help (And the Ones That Don’t)
Some apps and digital tools claim to verify your meds. But here’s the truth: physical label verification is still the most accurate method.
A 2023 study in the Journal of the American Pharmacists Association found that apps had a 7.2% error rate. Physical labels? Just 2.1%. Why? Apps can misread text, show outdated info, or fail to sync. A printed label doesn’t glitch.
That said, there are useful tools:
- Magnifying tools - 82% of pharmacies offer free magnifiers. Ask for one if the print is too small.
- Personal Medication Record (PMR) - Keep a list of all your meds, dosages, prescribers, and pharmacies. Most major chains offer free digital PMRs in their apps. Update it every time you get a new script.
- QR codes on new labels - The FDA is testing QR codes that link to digital verification pages. Early results show a 19% improvement in accuracy. But don’t rely on them yet-still check the printed info.
Don’t trust apps to replace your eyes. Use them to support your checks-not replace them.

Why This Is Especially Important for Seniors and Complex Meds
If you’re over 65, taking multiple medications, or on high-risk drugs like blood thinners, opioids, or insulin-this step is non-negotiable.
One in three seniors has trouble reading small print. That’s why 37% of people over 65 miss label errors simply because they can’t see them. Pharmacies are required to help. Ask for large-print labels. Ask for a verbal confirmation. Ask them to read it out loud.
Specialty meds-like those for cancer, MS, or rare diseases-are more likely to have labeling errors. If you’re on one of these, make a habit of comparing each new bottle to the last. Take a photo of the label when you first get it. Use it as a reference next time.
What You Can Do Today to Stay Safe
You don’t need a degree in pharmacy to protect yourself. You just need to be consistent.
- Always check the label before you take any new prescription.
- Keep a written or digital list of your meds and who prescribed them.
- Ask pharmacists to spell out unfamiliar names.
- Use the free magnifier if you need it.
- If something feels off-trust it. Call.
People who verify their labels report 27% fewer medication errors and 31% better adherence to their treatment plans. That’s not a small gain. That’s life-changing.
Final Thought: You’re the Last Line of Defense
Doctors make mistakes. Pharmacies make mistakes. Systems fail. But you? You’re the one holding the bottle. You’re the one who sees the name. You’re the one who notices the difference.
No app, no system, no pharmacist can replace that. The FDA says prescriber verification is a “critical patient action.” That means it’s not optional. It’s essential.
Next time you pick up your prescription, don’t rush. Look. Read. Confirm. It might just save your life.
What if the prescriber name on my label doesn’t match who I saw?
Stop. Don’t take the medication. Call the pharmacy immediately using the number on the label. Ask them to verify the original prescription with your provider’s office. If they can’t confirm it’s correct, contact your doctor directly. This mismatch could mean you received someone else’s prescription, which can be life-threatening.
Is it normal for the pharmacy name to be different from where I picked it up?
No. The pharmacy name on the label should match the legal name of the location where you received the medication. If you picked it up at CVS but the label says “Express Scripts Mail Order,” you may have received a mail-order prescription by mistake. Call the pharmacy to confirm. This is especially dangerous if you’re on a controlled substance or high-risk medication.
Can I trust the barcode or QR code on the label instead of reading the text?
No. While QR codes are being tested by the FDA and may help, they’re still new and not fully reliable. A 2023 study showed physical label verification is more accurate than digital tools. Always read the printed text. Use QR codes as a supplement, not a replacement.
Why do some labels have an NPI number and others don’t?
The NPI (National Provider Identifier) is required by federal law for all prescriptions, but it’s not always printed on small retail labels due to space limits. If you don’t see it, it’s not necessarily an error-but you should still verify the prescriber’s full name matches who you saw. If you’re unsure, call the pharmacy and ask for the NPI number.
How often should I update my personal medication record?
Update your personal medication record every time you get a new prescription, stop a medication, or change a dose. Many pharmacies offer free digital tools in their apps to help you track this. Keeping an up-to-date list helps you verify labels faster and gives you accurate info to share with any new provider.
Are mail-order pharmacies less safe than local ones?
Mail-order pharmacies have a 23% higher error rate than local pharmacies, mainly because they handle more complex prescriptions and process large volumes. That doesn’t mean they’re unsafe-but it does mean you need to be extra careful. Always compare your new bottle to your last one. If anything looks different, call them before taking it.
What if I’m visually impaired and can’t read the label?
You have the right to accessible medication information. Ask the pharmacy for large-print labels, audio labels, or verbal confirmation from a pharmacist. Most pharmacies provide free magnifiers and will read the label to you. If they refuse, contact your state’s pharmacy board. Patient safety includes accessibility.
Jay Ara
December 25, 2025 AT 23:31Dan Alatepe
December 26, 2025 AT 19:59Angela Spagnolo
December 28, 2025 AT 05:13Sarah Holmes
December 28, 2025 AT 09:25SHAKTI BHARDWAJ
December 29, 2025 AT 09:48Jody Kennedy
December 30, 2025 AT 02:59christian ebongue
December 31, 2025 AT 02:50jesse chen
December 31, 2025 AT 20:56Prasanthi Kontemukkala
January 2, 2026 AT 13:09Alex Ragen
January 4, 2026 AT 10:46Lori Anne Franklin
January 5, 2026 AT 10:08