How to Time Your Medications to Avoid Dangerous Drug Interactions
 Nov, 22 2025
Nov, 22 2025
Getting your meds right isn’t just about taking them-it’s about when you take them. Many people don’t realize that taking two pills at the same time can make one of them useless-or worse, cause serious harm. The difference between a safe day and a hospital trip can come down to a simple 2-hour gap.
Why Timing Matters More Than You Think
Not all drug interactions are created equal. Some happen because drugs compete for the same liver enzyme. Others happen because one pill sticks to another in your stomach like glue. The second kind? That’s where timing saves lives.
Take fluoroquinolone antibiotics like ciprofloxacin. If you swallow them with an antacid-say, Tums or Maalox-you’re basically throwing away the antibiotic. Studies show absorption drops by up to 90% when they’re taken together. But if you wait just 2 hours after the antacid, the antibiotic works like it’s supposed to. Same goes for tetracycline antibiotics: calcium in dairy, supplements, or even fortified orange juice can block absorption. Separate them by 2-3 hours, and you get full benefit.
This isn’t theory. It’s documented in FDA guidelines and backed by real-world data from hospitals. The Dutch healthcare system started tracking these timing issues back in 2006 and built them into their national drug database. Today, about 20-30% of all documented drug interactions can be avoided just by spacing out doses.
Top 5 Medications That Need Space
Some drugs are especially picky about when they’re taken. Here are the big five that demand attention:
- Levothyroxine (thyroid medicine): Needs 4 full hours before any iron, calcium, or multivitamin. Even a 1-hour gap isn’t enough. Studies in the Journal of Clinical Endocrinology & Metabolism show 95% absorption only happens with 4+ hours separation.
- Bisphosphonates (like alendronate for osteoporosis): Must be taken on an empty stomach with plain water. Wait at least 30 minutes before eating, drinking anything else, or taking other meds. These drugs absorb only in the upper part of your small intestine-and anything else in your gut blocks them.
- Proton pump inhibitors (PPIs like omeprazole): Often taken with iron supplements. PPIs reduce stomach acid, which iron needs to absorb properly. Spacing them 2-4 hours apart cuts the risk of iron deficiency by over 30%, according to a 2021 study at UCSF Medical Center.
- Statins (like atorvastatin): Grapefruit juice can cause dangerous buildup of these drugs. But timing won’t fix this. This is a metabolic interaction-so avoid grapefruit entirely. Timing only helps with absorption issues, not enzyme problems.
- Antibiotics (doxycycline, minocycline): Don’t take them with milk, antacids, or iron pills. Wait 2-3 hours before or after. These antibiotics bind to minerals and vanish before they can work.
When Timing Doesn’t Work (And What to Do Instead)
Not every interaction can be fixed by waiting. Some drugs mess with your liver’s enzymes-and no amount of spacing helps.
Warfarin (a blood thinner) and metronidazole (an antibiotic) are a dangerous pair. Metronidazole slows down how fast your body breaks down warfarin. The result? Too much warfarin in your blood. That raises bleeding risk dramatically. No matter when you take them, the interaction stays. The fix? Either switch to a different antibiotic or lower the warfarin dose under close monitoring.
Same goes for clarithromycin and colchicine. Clarithromycin blocks the enzyme that clears colchicine from your body. Even with timing, toxicity risk stays high. The FDA recommends a 2-hour gap-but that’s just a backup. The real solution is avoiding the combo entirely in high-risk patients.
If your meds are metabolized by CYP3A4 or CYP2C9 enzymes, timing won’t help. You need substitution, dose change, or close lab monitoring. Ask your pharmacist: “Is this a pharmacokinetic or pharmacodynamic interaction?” If they say “metabolic,” don’t rely on timing.

How to Actually Make It Work in Real Life
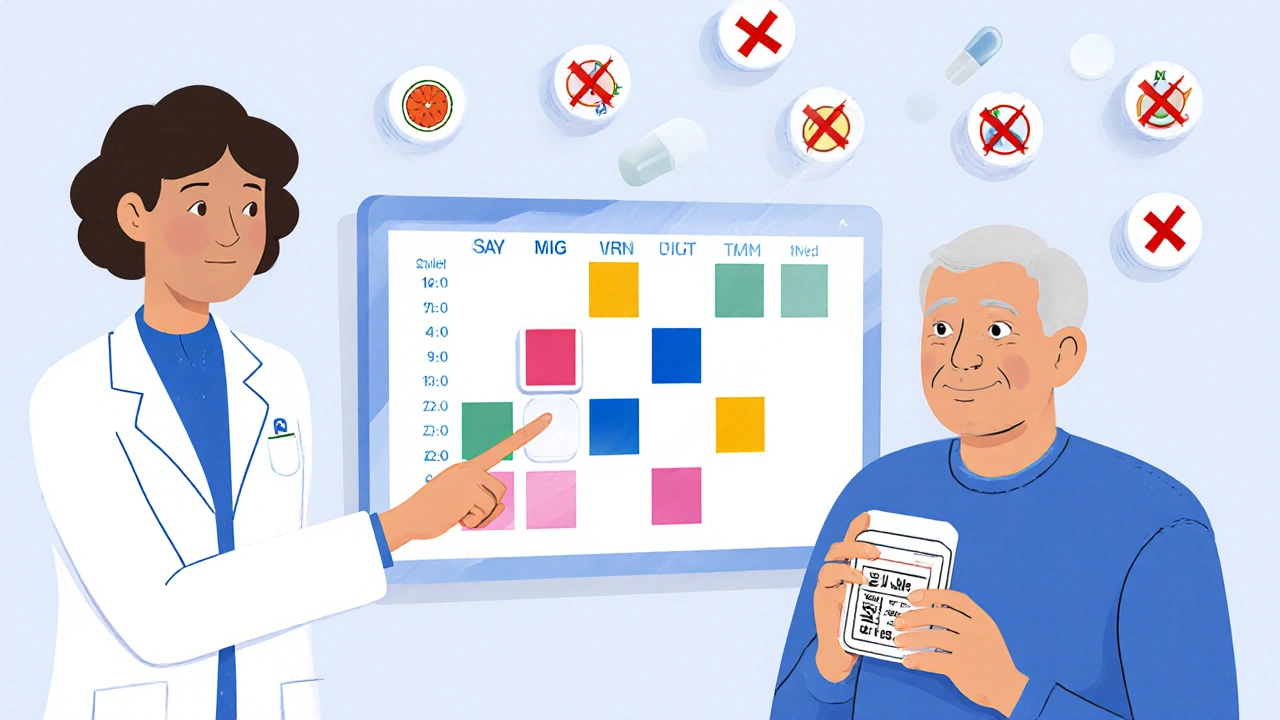
Knowing what to do is one thing. Doing it every day with 10 different pills? That’s another story.
Most people on 5+ medications struggle. A 2022 survey found 40% of patients forget or misunderstand their timing rules. Common complaints: “I don’t know which ones need space,” or “I skipped a dose because I got confused.”
Here’s how to make it stick:
- Use a pill organizer with time slots. Buy one with 4-6 compartments per day. Label them: “Morning,” “Afternoon,” “Evening,” “Night.” Put meds that need spacing in separate slots.
- Set phone alarms. Use apps like Medisafe or MyTherapy. They let you set custom alerts for “Take X, then wait 2 hours before Y.” A 2021 trial showed these apps improved timing adherence by 57%.
- Write it down. Keep a simple chart: “Levothyroxine at 7 AM, wait 4 hours. Iron at 11 AM. Calcium at 6 PM.” Tape it to your bathroom mirror.
- Ask for help. Pharmacists can print a personalized schedule. Many hospitals offer free medication reviews. Use them.
One nurse in a geriatric ward started using color-coded pill boxes-red for morning meds, blue for afternoon-and saw a 43% drop in timing errors. Simple tools, big results.
What Doctors and Pharmacies Are Doing Now
Hospitals have caught on. Eighty-two percent now use electronic systems that flag timing conflicts when a doctor writes a prescription. These systems pull from national databases like Lexicomp and show alerts like: “Ciprofloxacin and calcium-separate by 2 hours.”
But here’s the catch: these systems are noisy. About 45% of alerts are false positives-meaning they warn you even when the patient takes the drugs at the right time. That leads to alert fatigue. Doctors start ignoring them.
That’s why new AI tools are rolling out. Epic Systems’ 2023 update considers individual factors-like kidney function, age, and even stomach pH-to reduce false alarms by 38%. The FDA is also pushing for personalized timing based on genetics. In the future, your pill schedule might adjust based on your DNA.
For now, the best defense is still a well-informed patient and a pharmacist who checks your full list every time you refill.
Who Needs This the Most?
If you’re over 65 and take 5 or more medications, you’re at highest risk. The CDC says this group has three times the rate of time-dependent interactions compared to younger adults. Why? More meds. Slower metabolism. More chronic conditions. More supplements.
But it’s not just seniors. Anyone on chronic meds-like diabetes, high blood pressure, or autoimmune drugs-is at risk. Especially if they’re also taking OTC stuff: antacids, iron, calcium, or even herbal supplements like St. John’s Wort.
One study found that 18% of preventable drug errors in Europe came from poor timing-not wrong doses, not wrong pills. Just wrong timing.
Start Here: Your 3-Step Action Plan
You don’t need to memorize 50 drug interactions. Just follow this:
- Make a full list. Write down every pill, patch, liquid, and supplement you take-including vitamins and OTC meds. Don’t skip the “I don’t think it matters” stuff.
- Check for timing risks. Use a free tool like the FDA’s Drug Interaction Checker or ask your pharmacist. Look for: antacids, calcium, iron, dairy, grapefruit, or other meds taken at the same time.
- Build your schedule. Use a pill organizer, set alarms, and write a simple chart. Test it for a week. If you’re confused, go back to your pharmacist. Don’t guess.
Timing your meds isn’t about being perfect. It’s about being smart. One small gap can mean the difference between your drug working-or failing silently, with no warning.
Can I take all my pills together if I’m in a hurry?
No. Taking everything at once increases the risk of drug interactions, especially with medications like antibiotics, thyroid pills, or iron supplements. Even if you feel fine, the drugs may not be working as they should. Spacing them out by 2-4 hours is often necessary for effectiveness and safety.
What if I forget to wait the recommended time between meds?
If you accidentally take two interacting drugs close together, don’t double up on the next dose. Skip the next scheduled dose if it’s too soon, and return to your normal schedule. Call your pharmacist or doctor for advice-they can tell you if you need to monitor for side effects or adjust your plan.
Do I need to time my vitamins and supplements too?
Yes. Many supplements interfere with medications. Calcium, iron, magnesium, and zinc can block antibiotics and thyroid drugs. Multivitamins often contain these minerals. Always check with your pharmacist before combining supplements with prescription meds.
Can I use a pill organizer to help with timing?
Absolutely. Pill organizers with separate compartments for morning, afternoon, evening, and night help prevent mix-ups. Choose one with labeled slots and use it with alarms or written instructions. Studies show this reduces timing errors by up to 43%.
Why don’t my doctors always tell me about timing?
Many doctors focus on the right dose and drug, not the timing. Time-dependent interactions are still under-discussed in medical training. Only 28% of outpatient clinics consistently document timing instructions. It’s up to you to ask: “Do any of these meds need to be spaced apart?”
Are there apps that help with medication timing?
Yes. Apps like Medisafe, MyTherapy, and Mango Health let you set custom alerts for medication spacing. They can remind you to wait 2 hours before your next pill. In clinical trials, these apps improved timing adherence by over 50%.
Final Thought: Small Gaps, Big Results
You don’t need to be a pharmacist to keep your meds safe. You just need to know that timing matters. A 2-hour gap between your antibiotic and your antacid. A 4-hour wait before your iron after your thyroid pill. These aren’t just rules-they’re your safety net.
Every year, tens of thousands of hospital visits happen because someone took two pills too close together. You can avoid being one of them. Start today. Make your list. Ask your pharmacist. Set your alarms. Your body will thank you.
Patrick Marsh
November 22, 2025 AT 17:57Antacids and antibiotics? 2-hour gap. Done. No drama.
Danny Nicholls
November 22, 2025 AT 22:01OMG this is LIFE-CHANGING 😭 I’ve been taking my levothyroxine with my multivitamin for YEARS… no wonder I felt like a zombie. Just set up Medisafe with 4-hour alerts. My thyroid is gonna thank me 🙏
Robin Johnson
November 24, 2025 AT 09:53Most people don’t realize this isn’t about being ‘perfect’-it’s about being intentional. If you’re on 5+ meds, your body isn’t a soup pot. You’re not mixing ingredients-you’re managing chemical pathways. Skip the ‘I’m in a hurry’ excuse. Your liver doesn’t care how busy you are.
Latonya Elarms-Radford
November 25, 2025 AT 02:34Let’s be real-this isn’t just about pharmacokinetics. It’s about the modern human condition: we’ve outsourced our bodily autonomy to corporate pill schedules and algorithmic health apps. We’ve forgotten that medicine, at its core, is a ritual. A sacred pause between ingestion and effect. The 2-hour gap? It’s not a rule-it’s a meditation. A silent rebellion against the tyranny of convenience. When I take my levothyroxine at 6:58 AM, and wait until 11:02 AM for my iron, I’m not just avoiding drug interactions-I’m reclaiming my sovereignty over my own biology. The FDA doesn’t understand this. But I do.
Mark Williams
November 26, 2025 AT 00:04Key distinction: pharmacokinetic vs. pharmacodynamic. Timing fixes absorption (PK), not metabolism (PD). CYP3A4 inhibition? No amount of spacing helps. Clarithromycin + colchicine? Avoid. Full stop. That’s why AI systems now integrate CYP phenotyping data-future-proofing adherence. Pharmacies need to start flagging metabolic risks at dispensing, not just absorption.
Ravi Kumar Gupta
November 26, 2025 AT 23:10In India, we take 10 pills with chai and breakfast and call it ‘jugaad.’ But this? This is real. My uncle died from bleeding because he took warfarin with metronidazole-doctor never warned him. This post saved lives. Share it with every auntie and uncle on WhatsApp. We need this in Hindi too.
Rahul Kanakarajan
November 27, 2025 AT 08:41Wow. Another ‘you’re doing it wrong’ article. Did you even check if these guidelines apply to people with GERD or gastroparesis? Or just rich Americans with pill organizers? My grandma takes everything together because her stomach can’t handle 8 alarms a day. Your ‘perfect timing’ is a luxury. Not everyone has a $30 pill box or a pharmacist on speed dial.
New Yorkers
November 27, 2025 AT 18:42So let me get this straight-you’re telling me I can’t take my omeprazole with my iron because of ‘stomach acid’? In New York, we don’t wait-we hustle. You think your 2-hour gap is gonna stop the city? Nah. We take it all, then go to the ER when we bleed. That’s the American way.
David Cunningham
November 28, 2025 AT 02:17Yeah, I’ve been doing this for years-separate my thyroid from the calcium, skip grapefruit, use alarms. Simple. But honestly? The biggest win was just asking my pharmacist to print a chart. No apps, no fuss. Just paper and a pen. Works better than any tech.
luke young
November 29, 2025 AT 12:27Thanks for writing this. I showed it to my mom-she’s 72, on 8 meds, and thought all pills were ‘the same.’ Now she uses a color-coded box and actually asks her doctor about timing. Small change. Huge difference. Keep sharing stuff like this.