How to Measure Children’s Medication Doses Correctly at Home
 Jan, 13 2026
Jan, 13 2026
Getting the right dose of medicine for your child isn’t just important-it can be life-saving. A tiny mistake, like mixing up milliliters and teaspoons, can mean the difference between healing and harm. Every year, thousands of children end up in emergency rooms because of dosing errors with liquid medications. And most of these mistakes happen at home, not in hospitals. The good news? You don’t need to be a doctor to get it right. With the right tools and a few simple habits, you can protect your child from dangerous mistakes.
Why Measuring Medicine Wrong Is So Dangerous
Children aren’t small adults. Their bodies process medicine differently, and even a small overdose can cause serious harm. For example, giving 5 mL of a medication when the dose is actually 0.5 mL is a tenfold error. That’s not a typo-it’s a medical emergency. Certain drugs, like acetaminophen or antibiotics, are especially risky if given in the wrong amount. Too little won’t treat the infection. Too much can damage the liver or cause seizures.The biggest problem? People use the wrong tools. Kitchen spoons, dosing cups with unclear markings, and confusing labels all add up to mistakes. Studies show that about 7 out of 10 parents measure liquid medicine incorrectly. And it’s not because they’re careless-it’s because the system is confusing.
Only Use Milliliters (mL)-Never Teaspoons or Tablespoons
The American Academy of Pediatrics and the CDC agree: never use teaspoons or tablespoons to measure children’s medicine. A household teaspoon can hold anywhere from 3.9 to 7.3 mL-way off from the standard 5 mL. That’s a 30% error right there. Even worse, some parents think “one teaspoon” means the spoon they use for coffee. That’s not safe.All pediatric liquid medications should be measured in milliliters (mL) only. Look at the prescription label. If it says “1 tsp” or “½ tbsp,” ask the pharmacist to rewrite it in mL. Most pharmacies now do this automatically, but not all. If you’re unsure, call them. It takes 30 seconds, and it could save your child’s life.
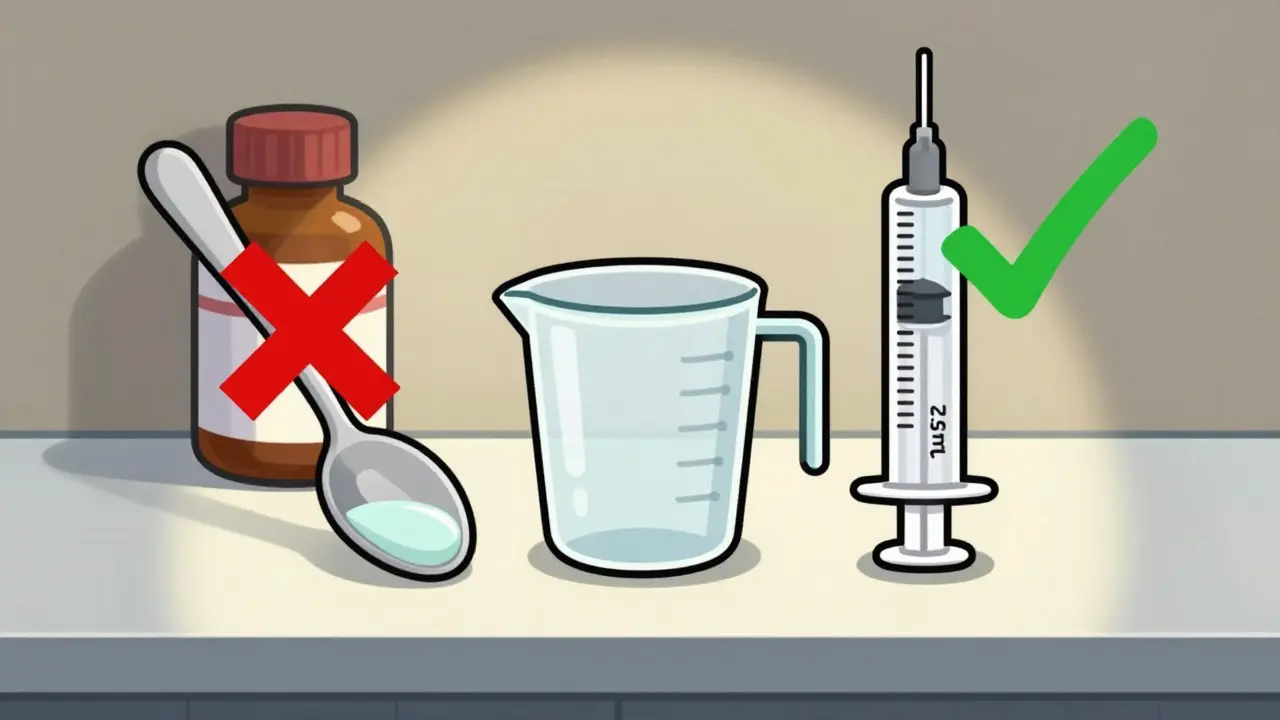
Use the Right Tool: Oral Syringes Are Best
Not all measuring tools are created equal. Here’s what works best:- Oral syringes (1-10 mL): The gold standard. They’re accurate, easy to use, and let you give the exact dose. For doses under 5 mL, they’re the only tool you should use. One study found they’re 94% accurate compared to just 76% for dosing cups.
- Dosing cups (5-30 mL): Fine for older kids who can drink from a cup, but risky for small doses. Error rates jump to nearly 70% when measuring 2.5 mL in a cup.
- Droppers: Good for babies or tiny doses, but hard to read accurately. Stick with syringes if possible.
- Medication spoons: Only use ones labeled in mL. Never use regular kitchen spoons.
Most pharmacies give you a syringe or dropper with the medicine. Keep it. Don’t throw it away. If you lose it, ask for a new one. Some pharmacies even sell affordable, accurate syringes for under $5. Look for ones with clear mL markings and a plunger that doesn’t stick.
How to Measure With an Oral Syringe
Using a syringe isn’t hard-but you have to do it right. Here’s how:- Shake the bottle first. Liquid medicines often settle. If you don’t shake, you might give a dose that’s too weak. Shake for at least 10 seconds.
- Draw the medicine slowly. Insert the syringe into the bottle, turn it upside down, and pull the plunger to the right line. Don’t rush.
- Check the meniscus. The liquid curves slightly at the top. Read the measurement at the bottom of that curve, not the top. Hold the syringe at eye level.
- Don’t trust the markings on the bottle. Only trust the syringe. The bottle might say “5 mL,” but if your syringe says 4.8 mL, go with the syringe.
- Give it slowly. Put the tip of the syringe inside your child’s cheek, not at the front of the mouth. Gently push the plunger. This helps avoid spitting or choking.
Pro tip: Use a permanent marker to mark the syringe with your child’s common doses. For example, if your child always gets 3 mL of amoxicillin, draw a line at 3 mL. That way, you won’t have to read the numbers every time.
Weight-Based Dosing: How to Calculate Correctly
Many pediatric doses are based on weight: mg per kilogram (kg). That means you need to convert pounds to kilograms.Use this simple formula: Weight in kg = Weight in pounds ÷ 2.2
Example: Your child weighs 33 pounds.
- 33 ÷ 2.2 = 15 kg
If the doctor prescribes 15 mg/kg of amoxicillin, then:
- 15 mg × 15 kg = 225 mg total per day
If it’s given twice a day, each dose is 112.5 mg. If the medicine is 250 mg per 5 mL:
- 112.5 mg ÷ 250 mg = 0.45
- 0.45 × 5 mL = 2.25 mL per dose
Always double-check with your pharmacist. Don’t guess. Even small math errors can lead to big problems.
Common Mistakes and How to Avoid Them
Here are the most frequent errors-and how to stop them:- Using kitchen spoons: Never. Even if you’ve done it before. Kitchen spoons vary too much.
- Confusing mg and mL: “20 mg” is not “20 mL.” One is a weight, one is a volume. Always read the label twice.
- Not shaking the bottle: This is the #1 reason kids get under-dosed with antibiotics. Shake before every dose.
- Using multiple caregivers without a plan: If Grandma, Dad, and Mom all give medicine, make sure everyone uses the same tool and writes down the time and dose. A simple chart on the fridge helps.
- Assuming “one teaspoon” is safe: Even if the label says it, ask for mL instead. Most doctors will change it.

What to Do If You Make a Mistake
If you accidentally give too much or too little:- Don’t panic. Most small errors won’t cause harm, but don’t ignore them.
- Call your pediatrician or poison control. In the U.S., call 1-800-222-1222. They’re free, confidential, and available 24/7.
- Write down what happened. How much did you give? What time? What medicine? This helps the doctor decide if action is needed.
- Don’t give another dose unless instructed. Overcompensating can make things worse.
Tools and Resources That Help
There are smart tools now that make dosing easier:- Color-coded syringes like NurtureShot reduce errors by 61% by matching the syringe color to the medication.
- Apps like MedSafety use your phone’s camera to scan the bottle and show you the right dose with step-by-step video instructions.
- Smart dosing cups (coming in 2025) will have built-in sensors to confirm the right amount before you give it.
Many children’s hospitals now give out free oral syringes at discharge. Ask for one. If your pharmacy doesn’t offer one, ask for a recommendation. You can buy them at most pharmacies or online for under $10.
Final Tip: Make a Dosing Chart
Create a simple chart for your child. Write down:- Medicine name
- Strength (e.g., 250 mg/5 mL)
- Weight in kg
- Each dose in mL
- How often (every 6 hours? twice daily?)
- When to stop
Put it on the fridge. Show it to babysitters, grandparents, and daycare staff. When everyone’s on the same page, mistakes drop dramatically.
Measuring children’s medicine correctly isn’t about being perfect. It’s about being careful. It’s about asking questions. It’s about using the right tool every single time. One small habit-reaching for the syringe instead of the spoon-can change everything.
Can I use a kitchen teaspoon if I don’t have a syringe?
No. A kitchen teaspoon can hold anywhere from 3.9 to 7.3 milliliters, which is far from the standard 5 mL. This variation can lead to under- or overdosing. Always use an oral syringe or dosing cup labeled in mL. If you don’t have one, call your pharmacy-they’ll give you one for free.
What’s the difference between mg and mL?
Milligrams (mg) measure weight-how much active ingredient is in the medicine. Milliliters (mL) measure volume-how much liquid you’re giving. For example, a medicine might be labeled 250 mg per 5 mL. That means each 5 mL contains 250 mg of the drug. Confusing the two can lead to dangerous mistakes. Always check both numbers on the label.
Why do I need to shake the medicine bottle before giving it?
Many liquid medicines are suspensions, meaning the active ingredient settles at the bottom. If you don’t shake it, the first dose might be too weak, and later doses might be too strong. Shake for at least 10 seconds before every dose to make sure the medicine is evenly mixed.
How do I convert my child’s weight from pounds to kilograms?
Divide the weight in pounds by 2.2. For example, if your child weighs 22 pounds, divide 22 by 2.2 to get 10 kg. Most pediatric doses are based on mg per kg, so this conversion is essential. Always double-check your math with your pharmacist.
What should I do if my child spits out the medicine?
Don’t automatically give another full dose. Wait 15-20 minutes. If your child spit out most of it, call your pediatrician. If only a little came out, it’s likely enough was absorbed. Giving a second full dose could lead to an overdose. Always check with a professional before redosing.
Lance Nickie
January 15, 2026 AT 06:59why do u need a syringe? just use a spoon. i’ve been giving my kid meds for 5 years n never died.
Milla Masliy
January 16, 2026 AT 08:45My mom used to use a kitchen spoon for everything-antibiotics, fever meds, even cough syrup. We never had an issue. But now I use a syringe because I know better. Thanks for the reminder that not everyone grew up with this info. Simple fix, huge impact.
Damario Brown
January 18, 2026 AT 00:08lol the ‘shaking the bottle’ thing is a myth. most pediatric suspensions are designed to be stable. unless it’s amoxicillin or something with visible particulates, you’re just wasting time. also, the 94% accuracy stat for syringes? source? i’ve seen studies that say it’s closer to 87% when you account for user error in drawing the dose. also, why are we assuming parents can read mL markings? literacy rates aren’t 100%. this post feels like a lecture from someone who’s never held a crying toddler at 3am.
sam abas
January 18, 2026 AT 20:20Okay, so let me get this straight-you’re telling me I need to buy a $5 syringe, shake the bottle for 10 seconds, read the meniscus at eye level, convert pounds to kilograms using a 2.2 divisor, and then mark my syringe with a permanent marker? Meanwhile, my kid’s pediatrician just says ‘give a teaspoon.’ And you’re acting like I’m a criminal for trusting them? Let’s be real. The system is broken. Pharmacies don’t give syringes unless you ask. Labels are printed in tsp and mL side by side. Doctors write prescriptions in mg/kg but don’t do the math for you. This isn’t about ‘habits’-it’s about lazy infrastructure. I shouldn’t have to be a pharmacist to give my kid Tylenol. And don’t even get me started on the ‘color-coded syringes’-that’s a marketing gimmick for people who think their child’s medicine is a LEGO set.
John Pope
January 19, 2026 AT 13:18We’ve turned parenting into a performance art. You don’t need a syringe. You need presence. You need to stop treating your child like a lab rat and start trusting your instincts. The body knows how to heal. The medicine is just a placeholder for attention. Shake the bottle? That’s not chemistry-it’s ritual. The real danger isn’t the 0.3 mL error-it’s the anxiety you’re teaching your child to associate with care. What if the real overdose is fear?
Clay .Haeber
January 21, 2026 AT 02:52Oh wow. A 15-page essay on how to not kill your kid with a dropper. Next up: ‘How to Breathe Without Suffocating Your Infant with the Air of Modernity.’ I’m sure the CDC and AAP are just thrilled you’ve unlocked the secret that ‘teaspoons are not medical devices.’ Congrats. You’ve joined the elite club of people who know the difference between mg and mL. Now go take a nap. You’ve earned it.
Priyanka Kumari
January 22, 2026 AT 18:17This is so helpful! In India, many families still use spoons because syringes aren’t always available or affordable. I’ve started sharing this with my neighbors-especially the part about calling the pharmacy. One aunt didn’t know she could ask for a syringe for free. Now she has three. Small changes, big difference. Thank you for writing this with clarity, not judgment.
Avneet Singh
January 24, 2026 AT 01:10The entire premise is flawed. Pediatric dosing should be standardized at the pharmaceutical level, not left to parental interpretation. Why are we burdening caregivers with conversion math and meniscus reading? This is a systemic failure masked as personal responsibility. Also, ‘oral syringes are the gold standard’? That’s a 2012 guideline. Newer devices like micro-dose pumps and AI-assisted dispensers are already in trials. This post is outdated.
Adam Vella
January 25, 2026 AT 02:14While the intent of this post is commendable, the pedagogical approach lacks epistemological rigor. The conflation of empirical accuracy (e.g., syringe precision) with behavioral compliance (e.g., shaking duration) introduces a normative bias that assumes universal cognitive capacity and access to resources. Furthermore, the recommendation to ‘mark the syringe’ introduces a confounding variable: the permanence of ink may degrade, leading to misinterpretation. A more robust framework would involve digital integration-QR codes linked to dosage algorithms embedded in the packaging. This is not a parenting issue. It is a public health infrastructure failure.
Nelly Oruko
January 26, 2026 AT 17:12i use a spoon. i dont care what the doc says. my kid is fine. also, i think the meniscus thing is overkill. just eyeball it. we’re not launching a rocket.
vishnu priyanka
January 28, 2026 AT 16:12Man, I used to use a spoon till my cousin’s kid got sick from overdosing. Now I keep a syringe in my bag like a flashlight. Funny how one bad story changes everything. Also, shaking the bottle? Yeah, I do that now. Turns out, medicine isn’t soda. Who knew?
Diana Campos Ortiz
January 28, 2026 AT 18:17Thank you for this. I was so nervous the first time I had to give my daughter antibiotics. I didn’t know what a meniscus was. I thought ‘mL’ meant ‘milligrams.’ I cried reading this. You made me feel less alone.
Jesse Ibarra
January 30, 2026 AT 07:50Of course you’re telling parents to use syringes. Meanwhile, the pharmaceutical industry is raking in billions selling $10 syringes and ‘smart cups’ while the same companies charge $800 for a bottle of liquid ibuprofen. This isn’t safety-it’s profit. You want to save kids? Make meds cheaper. Stop making parents beg for tools. Stop turning healthcare into a consumer product.
Acacia Hendrix
February 1, 2026 AT 05:40While the article demonstrates commendable adherence to evidence-based pediatric guidelines, it conspicuously omits any discussion of pharmacokinetic variability across developmental stages, particularly regarding cytochrome P450 enzyme maturation in infants under 6 months. Additionally, the assertion that ‘shaking for 10 seconds’ ensures homogeneity lacks validation against viscosity-dependent suspension dynamics. Without referencing ASTM F2764-20 or the WHO’s 2023 dosing tool validation study, this remains anecdotal pedagogy masquerading as clinical authority.
mike swinchoski
February 1, 2026 AT 10:03Wow, you’re really going to make every parent feel like a monster for using a spoon? I’m sorry, but I’ve been giving my kid medicine since he was 3 months old with a regular spoon and he’s now 7 and doesn’t have liver failure. Maybe your problem isn’t the spoon-it’s your anxiety. Also, who even has time to shake bottles for 10 seconds while a kid screams? Get a grip.