How Stress Triggers a Cough: Causes, Mechanisms & Relief
 Sep, 17 2025
Sep, 17 2025
Stress-induced cough is a persistent throat irritation that originates from the body’s response to psychological stress rather than a direct infection or airway obstruction. It often shows up as a dry, bark‑like sound, worsens during anxious moments, and may disappear once the mind relaxes.
What exactly is a stress‑related cough?
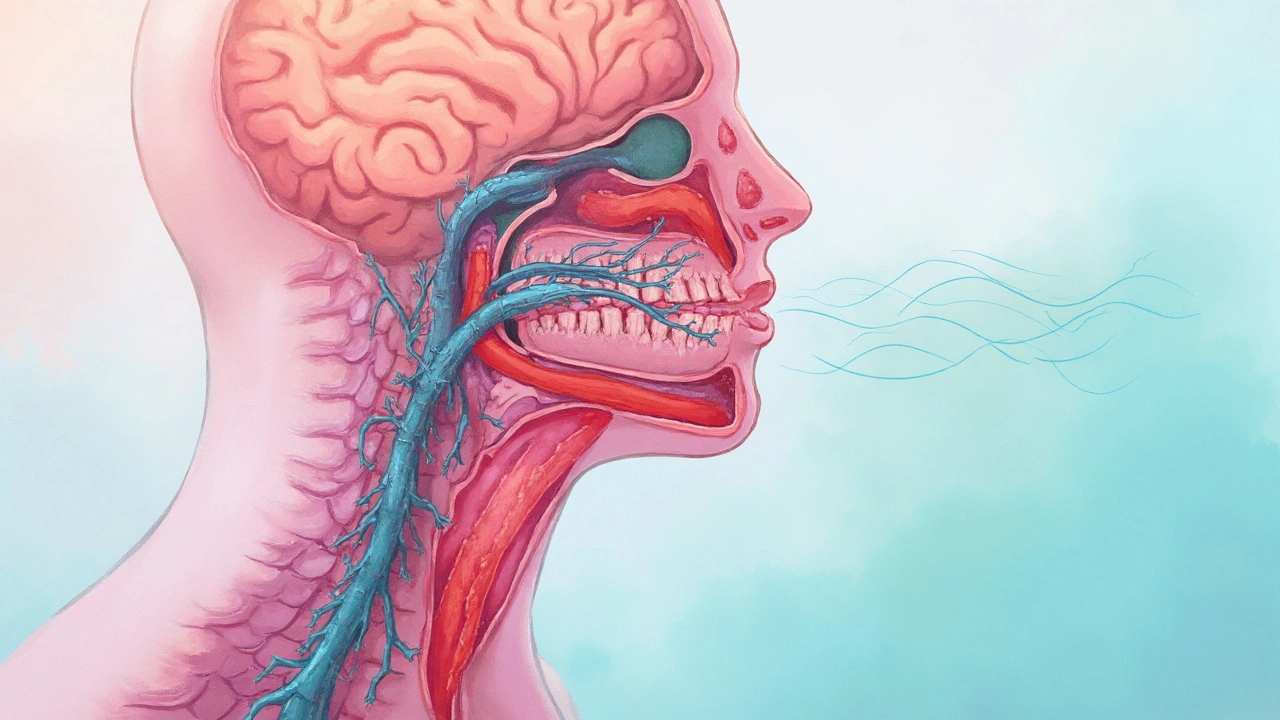
When you hear the word “cough,” you probably picture a cold or smoker’s irritation. In reality, the cough reflex is a complex network involving the vagus nerve, the brainstem, and the muscles of the throat. Stress throws a wrench into that network.
During a stressful episode, the body releases cortisol and adrenaline. These hormones boost heart rate, tighten airway muscles, and heighten sensitivity of the cough receptors. The result? A reflex that feels like a cough even though there’s no irritant in the lungs.
How stress messes with your breathing system
Three main pathways link stress to coughing:
- Neural hyper‑responsiveness: The autonomic nervous system (ANS) goes into “fight‑or‑flight” mode. The vagus nerve, part of the ANS, becomes over‑active, sending extra signals that trigger the cough reflex.
- Acid reflux amplification: Stress can relax the lower esophageal sphincter, allowing stomach acid to splash back into the throat (a condition known as gastro‑esophageal reflux disease, GERD). Acid irritation can provoke a cough that mimics a stress cough.
- Inflammatory cascade: Chronic stress raises systemic inflammation markers like C‑reactive protein (CRP). Inflammation in the airway lining makes it easier for even mild triggers to spark a cough.
These pathways often overlap, which is why it can be tricky to pin down the exact cause.
Common conditions that masquerade as a stress‑induced cough
Understanding the overlap helps you decide whether to treat the mind, the body, or both.
| Feature | Psychogenic (stress‑related) cough | GERD‑related cough | Asthma‑associated cough |
|---|---|---|---|
| Typical timing | Worsens during anxiety or after a stressful event | Often after meals or when lying down | Triggers by allergens, cold air, or exercise |
| Cough sound | Dry, bark‑like, sometimes “honking” | Dry or slightly productive with sour taste | Dry, may be wheezy |
| Response to antacids | Little to none | Often improves | None |
| Response to bronchodilators | None | None | Usually improves |
| Associated symptoms | Palpitations, muscle tension, sleep disturbances | Heartburn, sour taste | Shortness of breath, chest tightness |
Distinguishing a psychogenic cough from other types
Doctors often use a combination of history, physical exam, and simple tests. Here’s a quick checklist you can run through yourself:
- Do you notice the cough spikes when you’re nervous, giving a presentation, or watching a thriller?
- Does the cough disappear during deep, relaxed breathing or after a meditation session?
- Do you have frequent heartburn or a sour taste after meals?
- Is there a history of asthma, allergies, or recent respiratory infection?
If the first two points dominate, a stress‑related cough is likely. However, self‑diagnosis is never a substitute for a professional evaluation, especially if the cough lasts more than eight weeks.
Managing stress to calm the cough
Since the root cause is mental tension, tackling stress works directly on the cough reflex.
1. Controlled breathing exercises
Try the 4‑7‑8 technique: inhale through the nose for 4seconds, hold for 7seconds, exhale through the mouth for 8seconds. Repeat five times. This slows the ANS, reduces vagal hyper‑reactivity, and often stops the cough mid‑spasm.
2. Progressive muscle relaxation (PMR)
Starting at your toes, tense each muscle group for 5seconds, then release. Work up to the neck. PMR lowers cortisol levels and can lessen airway tightness.
3. Mind‑body therapies
Yoga, TaiChi, and guided imagery have been shown in several clinical trials to cut CRP by up to 30% and improve cough‑related quality of life scores.
4. Lifestyle tweaks
- Limit caffeine and nicotine - both spike adrenaline.
- Stay hydrated; warm herbal teas (e.g., ginger‑lemon) soothe the throat.
- Maintain a regular sleep schedule - sleep deprivation raises cortisol.
When stress‑focused methods don’t fully silence the cough, consider adjunct treatments like low‑dose antihistamines (for laryngeal irritation) or short courses of proton‑pump inhibitors if GERD is a contributor.
When to seek professional help
A cough that persists beyond 8weeks, produces blood, or is accompanied by fever, weight loss, or severe shortness of breath warrants a doctor’s visit. Specific red flags for stress‑related cough include:
- Sudden onset after a traumatic event.
- Interference with daily activities or sleep.
- Development of voice strain or hoarseness.
Clinicians may order a chest X‑ray, pulmonary function tests, or a 24‑hour pH study to rule out organic causes before labeling it “psychogenic.”
Related concepts and next steps
This article sits within a broader health cluster that includes:
- Stress and the immune system - how chronic tension weakens defense against infections.
- Mind‑body approaches for chronic cough - deeper dive into CBT and hypnotherapy.
- Nutrition and inflammation - foods that can lower CRP and support airway health.
After you’ve tried the stress‑relief techniques, you may want to explore those topics to get a full picture of how mental wellness impacts respiratory health.
Frequently Asked Questions
Can anxiety alone cause a cough?
Yes. Anxiety spikes the autonomic nervous system, which can over‑activate the vagus nerve and produce a dry, persistent cough even without any physical irritant.
How is a stress‑induced cough different from a post‑nasal drip cough?
Post‑nasal drip usually worsens when lying down and produces a “phlegmy” sensation. A stress cough is dry, peaks during moments of tension, and often improves with relaxation techniques.
Do over‑the‑counter cough suppressants work for stress coughs?
They may provide temporary relief, but they don’t address the underlying nervous‑system trigger. Long‑term relief comes from stress‑management strategies.
Can lifestyle changes reduce cortisol enough to stop the cough?
Regular exercise, adequate sleep, and mindfulness practices can lower baseline cortisol by 20‑30% in most adults, which often translates into fewer cough episodes.
When should I see a doctor for a chronic cough?
If the cough lasts more than eight weeks, produces blood, is accompanied by fever, weight loss, or severe breathlessness, or if it’s disrupting sleep and daily life, schedule a medical evaluation promptly.
vanessa parapar
September 24, 2025 AT 12:10Okay but have you ever tried just not being a stress magnet? Like, I get it, life’s hard, but your cough isn’t a personality trait. Stop giving your vagus nerve permission to throw tantrums. Try therapy, not just ginger tea.
Ben Wood
September 25, 2025 AT 02:49Actually, the vagus nerve doesn't 'throw tantrums'-it's a cranial nerve with parasympathetic fibers that modulate bronchial tone and laryngeal sensitivity via the cough reflex arc, which is hyperactivated under cortisol-induced sympathetic dominance. You're oversimplifying neurophysiology. Also, ginger tea has no proven antitussive mechanism beyond placebo.
Sakthi s
September 25, 2025 AT 03:31Simple truth: stress cough goes away when you breathe. Try it.
Rachel Nimmons
September 25, 2025 AT 19:41Did you know the FDA quietly approved a new class of neuro-modulating cough suppressants last year? But they’re only available to people who pass a psychological screening. That’s why your ‘stress cough’ never goes away-they’re hiding the real cure.
Abhi Yadav
September 26, 2025 AT 06:35We're all just carbon-based stress machines screaming into the void. Your cough? It's your soul trying to speak. The body doesn't lie. It just coughs louder when the mind refuses to listen. 🌌
Julia Jakob
September 26, 2025 AT 23:35LOL at people who think breathing exercises fix everything. I had a cough for 11 months. Turned out it was mold in my apartment. No one talks about mold. Everyone wants to fix your soul. Your cough isn't spiritual. It's toxic.
Robert Altmannshofer
September 27, 2025 AT 13:55Man, this is one of those posts that makes you realize how deeply our minds and bodies are wired together. I used to think coughs were just bugs or smoke. Then I started noticing mine spiked every time I had a work call. Now I do the 4-7-8 before Zoom. It’s not magic-it’s biology. And honestly? Kinda beautiful.
Kathleen Koopman
September 29, 2025 AT 05:494-7-8 breathing changed my life 😌✨ I used to cough during meetings, now I just chill. Also, yoga + chamomile = 🤍
Nancy M
September 30, 2025 AT 17:43It is noteworthy that the psychogenic cough, as a somatic manifestation of psychological distress, constitutes a diagnostic challenge within contemporary clinical practice. The interplay between autonomic dysregulation and laryngeal hypersensitivity warrants a multidisciplinary approach, integrating psychological evaluation with pulmonary diagnostics to ensure appropriate intervention.
gladys morante
September 30, 2025 AT 19:14I’ve had this cough for years. Everyone says ‘it’s stress.’ But what if it’s not? What if it’s something worse? What if they’re all lying to make you feel better? I don’t trust doctors. I don’t trust this post. I don’t trust you.
Precious Angel
October 1, 2025 AT 17:58Oh, so now it’s ‘stress’? That’s what they said about my chronic migraines too. Then they found the brain tumor. And the Lyme disease. And the mercury poisoning from my amalgam fillings. Everyone wants to blame your anxiety because it’s easier than admitting the medical system is broken. Your cough could be anything. They just don’t want to look. They want you to meditate and shut up.
Melania Dellavega
October 2, 2025 AT 15:46I used to think I needed to fix myself to stop the cough. Turns out, I just needed to stop fighting it. Letting go didn’t mean giving up-it meant listening. I started journaling, walking barefoot in the grass, and not checking my phone for an hour before bed. The cough didn’t vanish overnight. But it softened. Like a storm passing. I’m not cured. But I’m learning to breathe again.
Bethany Hosier
October 2, 2025 AT 19:26According to the 2023 WHO report on psychosomatic respiratory disorders, the rise in idiopathic cough cases correlates directly with increased social media usage and the normalization of ‘toxic positivity.’ The algorithmic pressure to appear calm while experiencing chronic anxiety creates a feedback loop of vagal dysregulation. This is not a medical issue-it is a systemic failure.
Krys Freeman
October 3, 2025 AT 06:30Stress cough? More like lazy cough. Just stop being soft. Americans need to toughen up. No one in my country coughs from stress. We have real problems.
Shawna B
October 3, 2025 AT 19:57i just cough when i get nervous. its weird. i never knew it was a thing.
Jerry Ray
October 4, 2025 AT 22:44Wait, so if I stop being stressed, my cough goes away? What if I don't want to stop being stressed? What if my stress is my identity? What if I like being anxious? Just saying.
David Ross
October 5, 2025 AT 02:29There is no such thing as a 'stress cough.' That’s a term invented by the pharmaceutical industry to sell mindfulness apps. The real cause? Glyphosate in your food. They’ve been poisoning the water supply since the 80s. You think this is about your nerves? No. It’s about control.
Sophia Lyateva
October 5, 2025 AT 10:04they dont want you to know that the cough is actually caused by 5g towers. i know because my neighbor’s cat started coughing too. and cats dont get stress. right?
AARON HERNANDEZ ZAVALA
October 6, 2025 AT 07:44Everyone’s got their own version of this. Mine’s a tight chest when I’m overwhelmed. I used to feel broken. Now I just say: ‘Hey, my body’s trying to tell me something.’ No judgment. No rush. Just presence. We’re all learning how to be human here.