How Pancreatic Duct Blockage Affects Diabetes Risk
 Oct, 22 2025
Oct, 22 2025
Pancreatic Duct Blockage Risk Calculator
Calculate Your Diabetes Risk
Based on the cause of pancreatic duct blockage, estimate your 5-year risk of developing diabetes.
Your Estimated Risk
Based on current medical research, your estimated 5-year risk of developing diabetes.
When the Pancreatic Duct Blockage occurs, the flow of digestive enzymes from the pancreas to the small intestine is disrupted, the organ’s balance can tip in ways that reach far beyond digestion. One surprising outcome is a direct impact on Diabetes a chronic condition characterized by elevated blood‑glucose levels due to insufficient insulin activity. Understanding why a clogged duct can lead to blood‑sugar problems helps patients and clinicians catch issues early and choose better treatment paths.
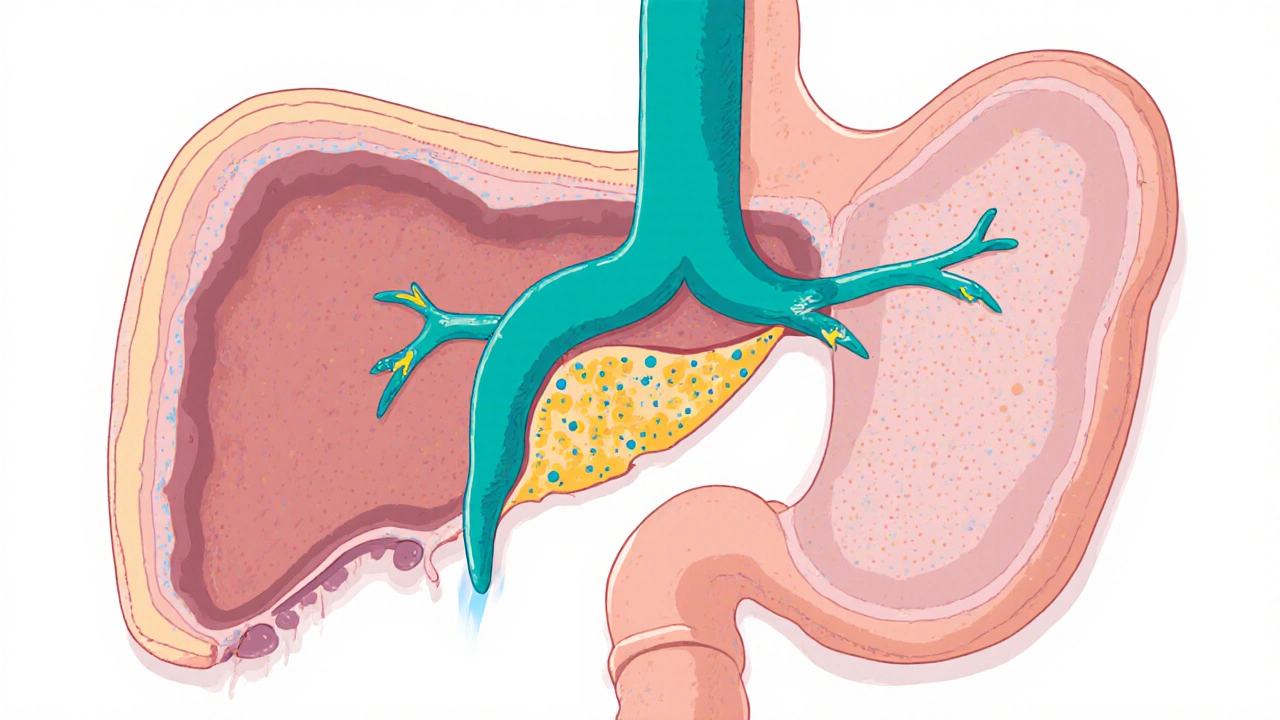
What the pancreatic ducts normally do
The pancreas has two functional sides. The exocrine part releases enzymes like amylase, lipase, and proteases through a network of ducts that empty into the duodenum. These enzymes break down carbs, fats, and proteins so nutrients can be absorbed. The main highway is the pancreatic duct, which joins the common bile duct before entering the duodenum at the ampulla of Vater.
Meanwhile, the endocrine side houses the islets of Langerhans, which secrete insulin, glucagon, and other hormones straight into the bloodstream. Though the two sides have separate jobs, they share the same tissue and blood supply, so a problem in one area can spill over to the other.
How a blockage disrupts normal flow
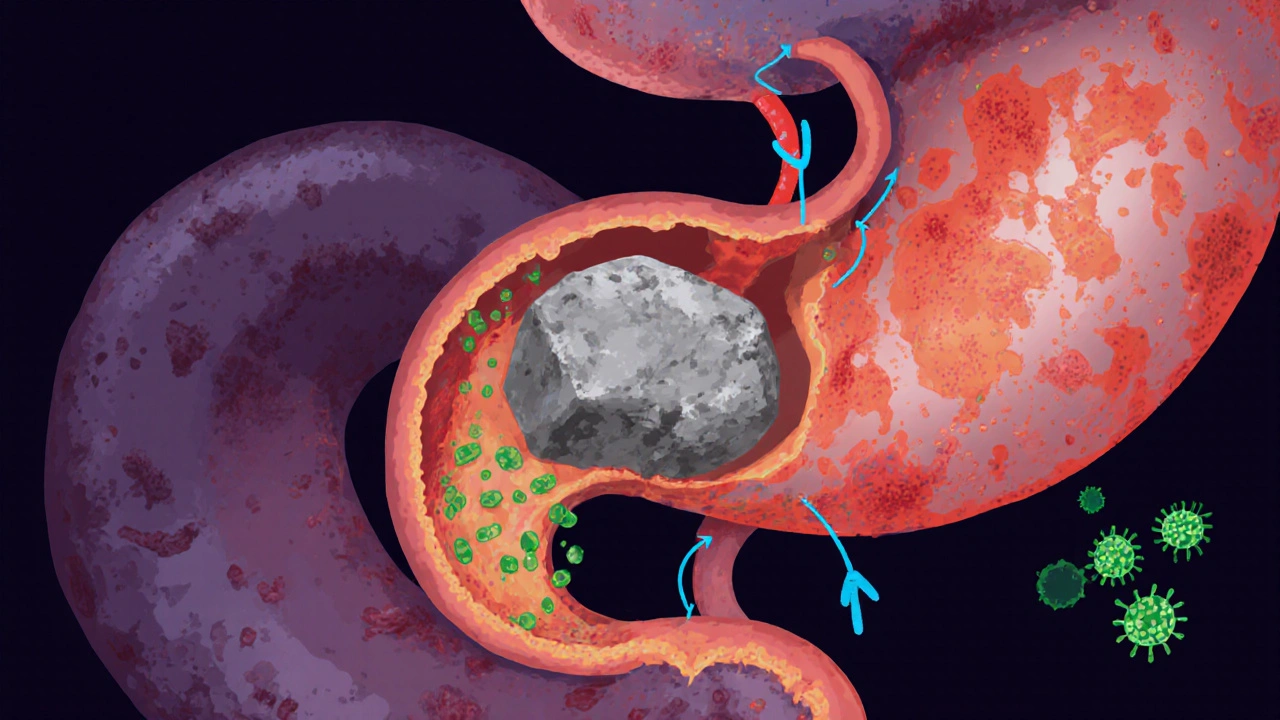
Blockage can happen for a few reasons:
- Calcium or protein stones (pancreatic calculi) that form in chronic inflammation.
- Scarring from repeated bouts of pancreatitis, which narrows the duct.
- Benign or malignant tumors pressing on the duct.
- Congenital anomalies, such as an abnormal duct angle.
When the duct is obstructed, pancreatic enzymes back up, causing swelling, pain, and sometimes autodigestion of the pancreas itself. Over time, the inflamed tissue can scar, reducing the organ’s ability to produce both digestive enzymes and hormones.
Why a blocked duct can trigger diabetes
The link isn’t just coincidence; several mechanisms connect the two:
- Islet damage from inflammation: Chronic inflammation leaks cytokines that damage beta‑cells, the insulin‑making cells.
- Reduced blood flow: Fibrotic tissue compresses tiny blood vessels, starving islets of oxygen and nutrients.
- Autoimmune cross‑reaction: In some patients, the immune system attacks both ductal cells and beta‑cells, a pattern seen in type 1‑like pancreatogenic diabetes (often called type 3c diabetes).
- Hormonal imbalance: The pancreas also releases somatostatin and pancreatic polypeptide, which help regulate insulin release. Blockage can throw these hormones off‑balance, leading to erratic glucose control.
Studies published in 2023‑2024 show that up to 40 % of patients with chronic pancreatic duct obstruction develop impaired glucose tolerance within five years, compared with just 7 % in matched controls. The risk jumps to 65 % when obstruction is caused by a tumor.
Key risk factors and warning signs
| Cause | Typical Onset | Effect on Insulin Production | Diabetes Risk |
|---|---|---|---|
| Pancreatic stones | Years of chronic pancreatitis | Gradual decline | Moderate (30‑40 %) |
| Fibrotic scarring | Long‑term inflammation | Reduced beta‑cell mass | High (45‑55 %) |
| Benign tumors (IPMN) | Often asymptomatic until obstruction | Variable, may stay normal | Low‑moderate (15‑25 %) |
| Malignant tumors | Rapid progression | Severe loss | Very high (≈70 %) |
Patients usually notice dull upper‑abdominal pain, unexplained weight loss, greasy stools (steatorrhea), and occasional episodes of high blood sugar. If you have any of these symptoms combined with a history of pancreatitis or gallstone disease, it’s worth getting a check‑up.
Diagnostic tools doctors rely on
- Magnetic Resonance Cholangiopancreatography (MRCP): Non‑invasive imaging that visualizes the ductal system in detail.
- Endoscopic Retrograde Cholangiopancreatography (ERCP): Allows both diagnosis and therapeutic stenting, but carries a small risk of inducing pancreatitis.
- Serum enzyme panel: Elevated amylase or lipase may point to acute blockage, while low C‑peptide levels hint at reduced insulin output.
- Oral glucose tolerance test (OGTT): Detects early dysglycemia even before fasting glucose rises.
Combining imaging with blood‑sugar testing gives clinicians a clear picture of how the duct problem is affecting endocrine function.
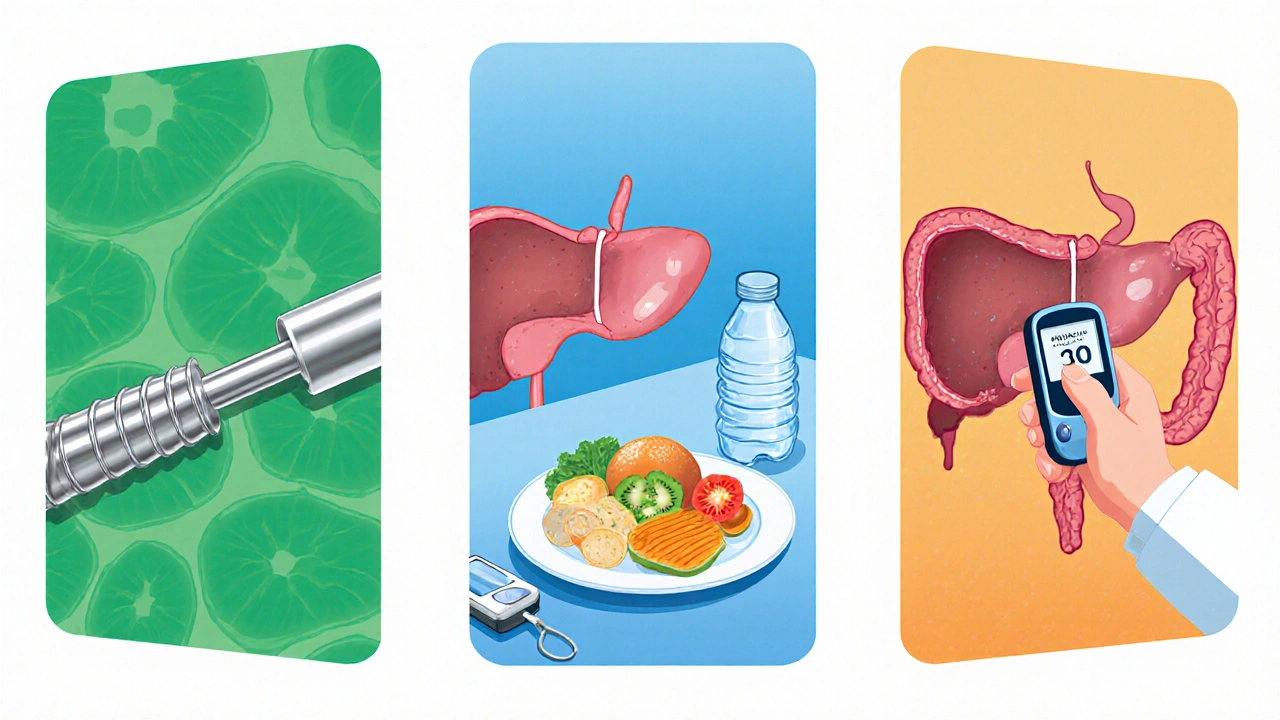
Treatment options that protect both digestion and glucose control
Therapy aims to restore duct patency, reduce inflammation, and preserve beta‑cell health.
- Endoscopic stenting: A tiny tube keeps the duct open, relieving back‑pressure and allowing enzymes to flow.
- Enzyme replacement therapy (ERT): Helps digestion while reducing the stimulus for the pancreas to overproduce enzymes.
- Anti‑inflammatory meds: Low‑dose steroids or immune‑modulators can curb chronic inflammation that harms islets.
- Nutrition tweaks: Low‑fat, high‑protein diets lower the workload on the exocrine pancreas and improve insulin sensitivity.
- Blood‑sugar monitoring: Early detection of rising glucose lets doctors start metformin or other agents before full‑blown diabetes sets in.
In severe cases, surgical options like a pancreaticojejunostomy (Puestow procedure) or even partial pancreatectomy may be necessary. The key is timely intervention-once beta‑cells are destroyed, they don’t regenerate.
Preventive habits for long‑term health
Even if you’ve never had a duct issue, adopting these habits can reduce future risk:
- Maintain a healthy weight; obesity raises both pancreatitis and diabetes chances.
- Avoid excessive alcohol; chronic drinking is a leading cause of pancreatitis and duct scarring.
- Limit high‑fat, processed meals that stimulate excess enzyme production.
- Stay hydrated and incorporate fiber‑rich foods to keep the digestive tract moving.
- Get regular check‑ups if you have a family history of pancreatic disease.
When prevention works, you protect both the exocrine and endocrine sides of the pancreas-keeping digestion smooth and blood sugar stable.
Key takeaways
- Blockage of the pancreatic duct can damage insulin‑producing cells through inflammation, reduced blood flow, and hormonal imbalances.
- Up to 40 % of people with chronic duct obstruction develop glucose intolerance; the figure climbs higher with tumor‑related blockages.
- Early imaging (MRCP or ERCP) combined with glucose testing catches the problem before diabetes fully sets in.
- Therapies that restore duct flow, reduce inflammation, and monitor blood sugar can halt progression.
- Lifestyle choices-weight control, moderate alcohol, low‑fat diet-cut the odds of both duct blockage and diabetes.
Can a single episode of pancreatitis cause diabetes?
A single mild attack usually doesn’t destroy enough beta‑cells to trigger diabetes, but severe or recurrent episodes can scar the pancreas and raise the risk substantially.
Is type 3c diabetes the same as type 2?
Type 3c (pancreatogenic) diabetes stems from pancreatic disease, whereas type 2 usually originates from insulin resistance. Treatment overlaps but addressing the underlying pancreas issue is essential for type 3c.
What imaging test is best for spotting a duct blockage?
MRCP offers detailed, non‑invasive images of the ductal tree and is often the first choice. ERCP adds therapeutic capabilities but carries a higher complication rate.
Can enzyme replacement therapy help prevent diabetes?
ERT reduces the pancreas’s workload, which can lessen inflammation and protect beta‑cells, indirectly lowering diabetes risk, especially in chronic blockage cases.
Are there any natural supplements that aid duct health?
Compounds like curcumin and omega‑3 fatty acids have anti‑inflammatory properties and may help reduce chronic pancreatitis severity, but they should complement, not replace, medical treatment.
Ritik Chaurasia
October 22, 2025 AT 15:37In India we see a lot of spicy, fried foods that can stress the pancreas, so a blocked duct is practically a recipe for trouble. The inflammation you described often shows up in people who binge on oil‑heavy curries, and that directly bites into insulin production. If you’re already prone to diabetes, keeping the duct clear should be on your priority list. Regular check‑ups and early imaging can catch the problem before the beta‑cells surrender.
Gary Marks
November 7, 2025 AT 21:44Wow, this article really blows the lid off a hidden villain in our bodies, and I’m not just saying that because I love a good drama. The pancreatic duct blockage is like a clogged highway in a megacity, traffic jams of enzymes backing up, causing chaos everywhere. Imagine trying to drive a delivery truck full of vital cargo only to hit a massive roadblock – that’s exactly what the exocrine side suffers, and the endocrine side gets hit too. The author nailed the connection between the swelling and the beta‑cell death, turning a boring fact into a full‑blown thriller. It’s crazy how chronic inflammation can bleed cytokines right into the insulin factories, effectively sabotaging the whole operation. Then there’s the blood‑flow issue, where fibrotic scar tissue crushes tiny vessels like a bulldozer, leaving the islets starved of oxygen, which is basically a slow‑motion murder. And let’s not forget the autoimmune cross‑reaction, where the immune system goes berserk, mistaking duct cells for invaders and taking beta cells down with them. The statistics are terrifying – up to 40 % of chronic blockage patients develop glucose intolerance, and that number skyrockets to 65 % when a tumor is involved. That’s a clear signal that we need to intervene early, not sit around waiting for the sugars to rise. Imaging like MRCP and ERCP are the detectives in this story, giving us a front‑row seat to the drama inside the pancreas. And the therapeutic options read like a superhero squad – stents, enzyme replacement, anti‑inflammatory meds, and even surgical bypasses ready to swoop in. Nutrition tweaks are the sidekick, quietly doing the work by lowering the pancreas’s workload, which is a smart move. The article also drops the bomb that once beta‑cells are gone, they don’t grow back, so prevention is the only real hope. It’s a call to action for doctors and patients alike to monitor blood sugar as soon as they spot a duct issue. Bottom line: if you ignore the signs, you’re basically signing a death warrant for your own insulin production, and that’s a fate nobody wants.
Vandermolen Willis
November 24, 2025 AT 04:50Sounds like a solid breakdown! 🌟 The way the duct blockage can ripple into diabetes risk is eye‑opening, especially for folks who think the pancreas only handles digestion. Keeping an eye on symptoms and getting imaging early can make a huge difference. Also, staying on top of diet and low‑fat choices helps both sides of the organ. 👍
Steven Young
December 10, 2025 AT 11:57They dont tell you that the pharma industry thrives on chronic duct issues
Kelli Benedik
December 26, 2025 AT 19:04Oh my god, this is literally the apocalypse for anyone with a blocked duct! 😱 The swelling, the scar tissue, the looming specter of diabetes – it’s like a horror movie playing out inside your own body. And the fact that tumors can push that risk up to 70%? That’s insane! We need to wake up and demand better screening before it’s too late! 💥
cariletta jones
January 12, 2026 AT 02:10Exactly, early detection can turn this nightmare around.
Kevin Hylant
January 28, 2026 AT 09:17Anyone with chronic pancreatitis should get regular glucose tests to catch problems early.