How Alcohol Affects Open-Angle Glaucoma Risk
 Oct, 7 2025
Oct, 7 2025
Alcohol & Open-Angle Glaucoma Risk Calculator
This calculator estimates your risk of developing open-angle glaucoma based on your alcohol consumption and key personal factors. Results are for educational purposes only.
Your Estimated Risk Level
When you hear the term Open-Angle Glaucoma is a chronic eye disease that slowly damages the optic nerve, often linked to elevated intraocular pressure (IOP), you probably wonder if your nightly glass of wine matters. The short answer: drinking habits can shift the odds, but the relationship isn’t black‑and‑white. Below we break down the science, the numbers, and what you can do today to protect your vision.
Key Takeaways
- Heavy and binge drinking raise IOP and increase open‑angle glaucoma (OAG) risk.
- Moderate alcohol intake shows mixed results; some studies suggest a slight protective antioxidant effect, others see no benefit.
- Age, genetics, and other health conditions heavily influence how alcohol impacts eye health.
- Regular eye exams and lifestyle tweaks (weight control, exercise) are the most reliable safeguards.
What Is Open‑Angle Glaucoma?
OAG accounts for about 90% of glaucoma cases worldwide. It develops when the eye’s drainage system (the trabecular meshwork) fails to clear aqueous humor efficiently, leading to a gradual rise in IOP. Over time, the pressure compresses the optic nerve fibers, causing irreversible vision loss.
Key attributes of OAG:
- Typical onset after age 40
- Slow, painless progression
- Family history raises risk 2‑5×
- Associated with hypertension, diabetes, and certain medications
Alcohol Consumption: The Basics
Alcohol is a psychoactive substance found in drinks like beer, wine, and spirits, measured by its blood alcohol concentration (BAC). Public‑health guidelines categorize drinking as:
- None - no alcoholic drinks.
- Moderate - up to 1 drink per day for women, up to 2 for men (≈14g ethanol).
- Heavy/Binge - >3 drinks in a single occasion for women, >4 for men, or daily intake exceeding moderate limits.
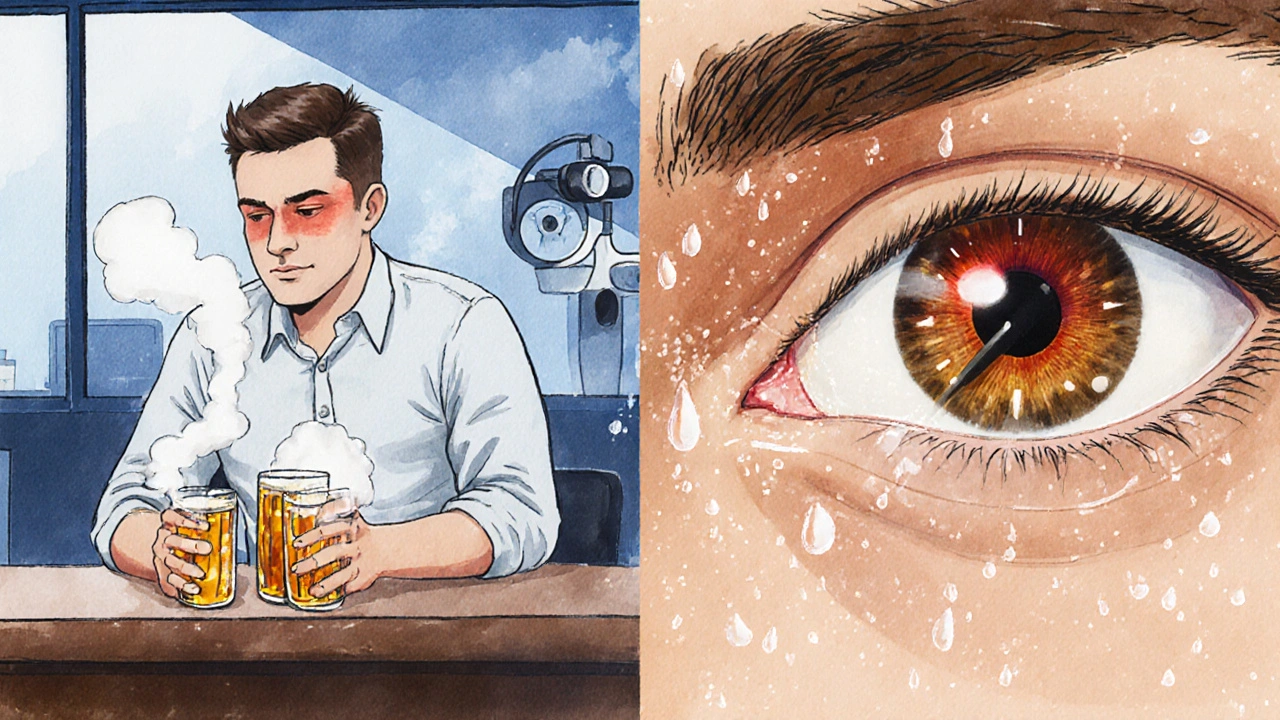
How Alcohol Affects Intraocular Pressure
Several mechanisms link alcohol to IOP changes:
- Vasodilation: Alcohol widens blood vessels, temporarily lowering systemic blood pressure, which can cause a fleeting drop in IOP.
- Fluid Retention: Chronic heavy drinking leads to dehydration followed by rebound fluid retention, raising IOP.
- Neurotoxicity: High BAC damages retinal ganglion cells, making them more vulnerable to pressure‑related injury.
- Oxidative Stress: Alcohol metabolism produces free radicals; excess oxidative stress can impair the trabecular meshwork.
What the Research Says
Evidence comes from large‑scale epidemiological studies, cohort analyses, and a handful of randomized trials. Below is a distilled view of the most cited findings.
| Study | Population | Drinking Category | Relative Risk (RR) for OAG | Key Note |
|---|---|---|---|---|
| Kang et al., 2022 (USA) | 45,000 adults, 10‑year follow‑up | Heavy (>14 drinks/week) | 1.68 | Statistically significant increase |
| Yuan et al., 2021 (Asia) | 30,000 seniors, cross‑sectional | Moderate (1‑7 drinks/week) | 0.92 | Non‑significant, slight protective trend |
| Green et al., 2020 (UK) | 12,000 patients, case‑control | Binge (≥5 drinks/occasion) | 1.45 | Higher odds in those with hypertension |
| Lee et al., 2023 (Meta‑analysis) | 8 studies, 250,000 participants | Any regular alcohol | 1.12 | Modest overall risk rise |
Takeaway: Heavy and binge drinking consistently show a 12‑68% higher risk of OAG, while moderate intake hovers around neutral or slightly protective, depending on the cohort.
Why Individual Differences Matter
Two people drinking the same amount can face different glaucoma outcomes because of:
- Age: The trabecular meshwork stiffens with age, making it less tolerant to pressure spikes.
- Genetics: Variants in the MYOC and OPTN genes amplify susceptibility to pressure‑related damage.
- Comorbidities: Hypertension, diabetes, and sleep apnea already push IOP upward; alcohol can exacerbate these effects.
- Medication Interactions: Some glaucoma meds (beta‑blockers) may interact with alcohol, altering systemic blood pressure and IOP.
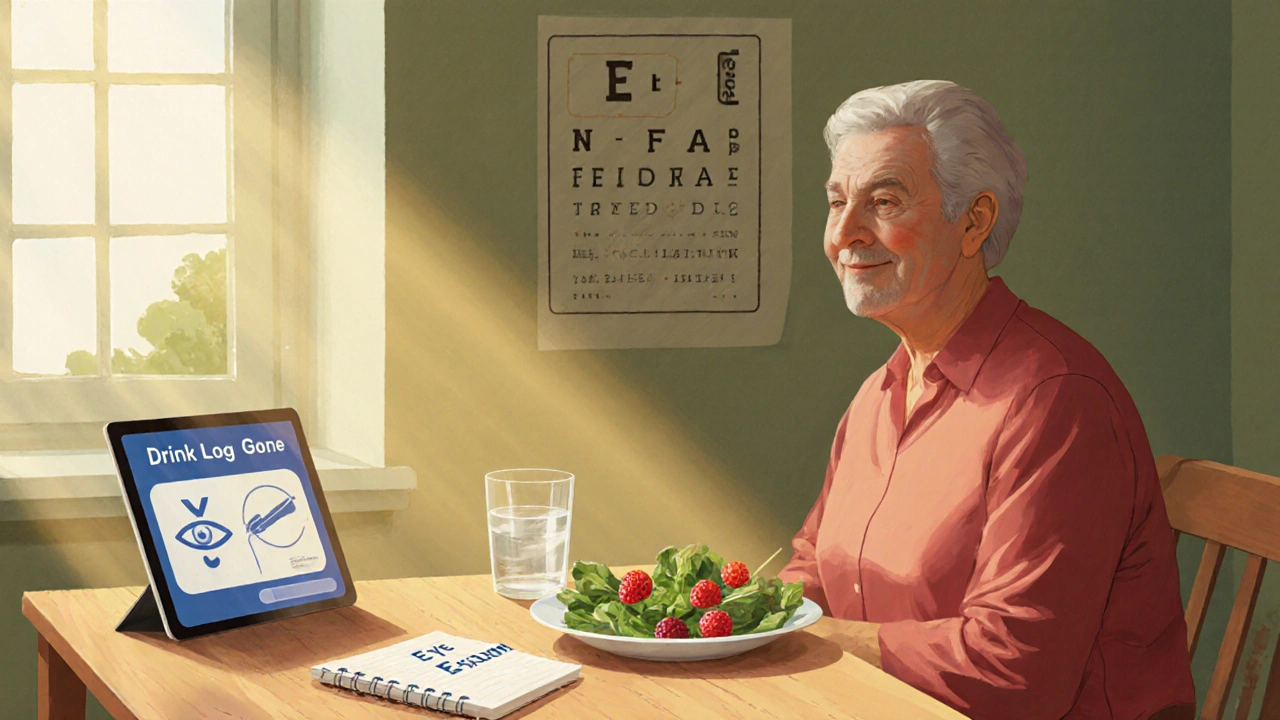
Practical Steps to Manage the Risk
- Know Your Baseline: Schedule a comprehensive eye exam that includes IOP measurement and optic‑nerve imaging.
- Track Your Drinks: Use a simple log or app; note type, amount, and frequency.
- Limit Heavy Binge Episodes: Aim for no more than 2 drinks per day for men, 1 for women, and avoid >4 drinks in a single sitting.
- Stay Hydrated: Alcohol dehydrates; replenish with water to reduce rebound fluid retention.
- Adopt a Heart‑Healthy Lifestyle: Regular aerobic exercise, balanced diet rich in antioxidants (leafy greens, berries), and weight control all help keep IOP in check.
- Discuss Medications: If you’re on glaucoma eye drops or systemic drugs, ask your ophthalmologist about safe alcohol limits.
Common Myths Debunked
Myth 1: “A glass of red wine protects my eyes because of antioxidants.”
Reality: While red wine contains resveratrol, the antioxidant dose is too low to offset the pressure‑raising effect of regular consumption, especially if you exceed moderate levels.
Myth 2: “If I have no family history, alcohol won’t affect me.”
Reality: Even without genetic predisposition, lifestyle factors like heavy drinking independently elevate IOP and can trigger OAG.
Myth 3: “Only people with glaucoma need to worry about alcohol.”
Reality: Preventing glaucoma is easier than treating it. Managing alcohol intake is part of broader ocular‑health prevention.
When to Seek Professional Help
If you notice any of the following, book an eye appointment ASAP:
- Gradual peripheral vision loss (tunnel vision)
- Frequent headaches with visual disturbance
- Sudden increase in eye pressure after heavy drinking episodes
- Family history of glaucoma plus any level of alcohol use
Early detection via visual‑field testing can preserve sight even if you continue to enjoy an occasional drink.
Future Directions in Research
Scientists are exploring whether specific alcohol types (e.g., low‑polyphenol beer vs. high‑polyphenol wine) have distinct effects on the trabecular meshwork. Large‑scale longitudinal studies using wearable IOP sensors may soon provide real‑time data on how drinking spikes pressure in everyday life.
Frequently Asked Questions
Does occasional binge drinking increase glaucoma risk?
Yes. Even infrequent binge episodes can cause short‑term IOP spikes that, over time, add to cumulative optic‑nerve stress. Studies show a 45% higher odds of OAG in people who binge at least once a month compared to non‑bingers.
Is there a safe amount of alcohol for glaucoma patients?
Guidelines suggest staying within moderate limits (≤1 drink/day for women, ≤2 for men) and avoiding binge patterns. Individual tolerance varies, so discuss personal limits with your ophthalmologist.
Can alcohol lower intraocular pressure?
Alcohol can cause a temporary dip in IOP due to vasodilation, but the effect usually lasts less than an hour and is followed by a rebound increase, especially after heavy intake.
Do certain drinks protect against glaucoma?
Current evidence does not support a protective role for any specific alcoholic beverage. The antioxidant content in wine is too low to offset pressure‑related damage, and spirits lack meaningful protective compounds.
How often should I get my eyes checked if I drink regularly?
Adults over 40 should have a full eye exam at least every two years. If you have a family history of glaucoma or consume alcohol heavily, annual checks are advisable.
Courtney Payton
October 7, 2025 AT 15:00We must recognize that choosing to sip daily is not just a casual habit but a moral crossroads. Every glass carries the weight of potential harm to our own eyes and to those who love us. While science offers statistics, the ethical duty to protect sight should outweigh fleeting pleasure. If you value future clarity, reconsider that nightly pour. Ignorance is never an excuse.
Muthukumaran Ramalingam
October 7, 2025 AT 17:13Look, I get that the article tries to be all scientific, but honestly it reads like a textbook written for robots. First off, the whole risk calculator feels like a gimmick that you can’t trust without a doctor. You plug numbers in and it spits out a color‑coded box, but real life isn’t that neat. I’ve known people who drink a couple of beers a week and still get diagnosed with glaucoma, so the “moderate is safe” line feels shaky. On the other hand, I’ve seen heavy drinkers who never get eye problems, which makes the whole correlation suspect. The studies cited are huge, but they also hide a lot of confounding variables like diet and genetics. It’s like saying “eat more carrots and you’ll see better” without mentioning sunlight. Also, the article never really explains why binge drinking spikes pressure, just throws a bullet point about “fluid retention”. That’s not enough detail for someone trying to make an informed decision. I feel the tone is too academic, not practical enough for the average Redditor who just wants a quick takeaway. And why does the calculator only ask for binge episodes per month? What about weekend warriors who binge only once a year? The risk factor might be different. The piece also forgets to mention that certain glaucoma meds can interact badly with alcohol, which is a huge oversight. If you’re on beta‑blockers, that could change everything. The recommendation to “stay within moderate limits” is vague; how does one measure a “drink” across different cultures? A pint of ale isn’t the same as a shot of whiskey. Lastly, while the antioxidant talk about red wine is cute, the dosage is negligible compared to the pressure‑raising effect. All in all, the article gives you a decent overview but leaves many practical gaps that need more real‑world context.
Garrett Williams
October 7, 2025 AT 19:26You can keep an eye on your health while still enjoying a drink or two. Small changes make a big difference.
joba alex
October 7, 2025 AT 21:40Contrary to the mainstream narrative, the data on ethanol’s impact on trabecular meshwork stiffness is inconclusive and often conflated with comorbid hypertension‑induced ocular hypertension. The article oversimplifies the mechanistic pathways, ignoring the role of nitric oxide modulation and peripheral vascular resistance that can actually transiently lower intra‑ocular pressure in certain phenotypes. Moreover, equating “binge” with a fixed numerical threshold disregards the pharmacokinetic variability across ethnicities and metabolic rates. So the blanket warning feels more sensational than evidence‑based.
Rene Lacey
October 7, 2025 AT 23:53When we contemplate the interplay between habit and physiology, we encounter a paradox of choice: the desire for immediate pleasure collides with the slow, inexorable march of degeneration. The eye, as a window to the soul, also serves as a barometer of systemic influences, and alcohol stands as a potent modulator of that delicate equilibrium. One might argue that the stochastic nature of disease emergence renders any single factor, including ethanol, merely a contributor among many. Yet, the cumulative weight of epidemiological evidence suggests that patterns of consumption do shape risk trajectories. It behooves us, therefore, to integrate behavioral prudence with medical vigilance. In practical terms, this translates to regular ophthalmic assessments intertwined with mindful drinking habits. The broader philosophical lesson lies in recognizing that liberty without responsibility can erode the very faculties we cherish. Thus, a balanced approach honors both autonomy and foresight.
johnson mose
October 8, 2025 AT 02:06That’s a beautiful synthesis, and it echoes what many clinicians observe in practice. While the science paints probabilities, the lived experience of patients adds layers of nuance-stress, diet, genetics, even socioeconomic factors. Adding a dash of color, think of the eye as a garden; alcohol can be both the rain that nourishes and the storm that floods. By staying hydrated, monitoring intake, and keeping up with check‑ups, you’re essentially tending that garden. The dramatic stakes are real, but the narrative isn’t doom; it’s empowerment through knowledge.
Charmaine De Castro
October 8, 2025 AT 04:20Hey folks! Just wanted to add a quick practical tip: when you log your drinks, try using a simple app that converts each beverage to standard units. This makes the calculator’s “drinks per week” field more accurate and helps you see patterns you might miss. Also, remember to schedule an eye exam if you’re over 40 or have a family history-early detection is key. Stay safe and keep those eyes healthy!
Mark Mendoza
October 8, 2025 AT 06:33👍👍 Absolutely! The app approach is 🔥🔥; it removes the guesswork and lets you focus on the bigger picture. Also, don’t forget that staying within the moderate limits (≤1 drink/day for women, ≤2 for men) 🎯🎯 can make a noticeable difference in long‑term ocular health. Keep an eye out! 👀👀
Dan Tourangeau
October 8, 2025 AT 08:46For anyone tracking intake, a spreadsheet with columns for date, type of drink, and volume works well. It’s quick to set up and can be reviewed before your eye doctor appointment.
Bernard Valentinetti
October 8, 2025 AT 11:00Indeed-however, one must acknowledge that the mere act of quantification does not magically confer wisdom; the epistemic leap from raw data to meaningful insight requires a nuanced interpretive framework, which, alas, many overlook!!! 📊📊 Moreover, the socio‑cultural context of alcohol consumption imbues each entry with symbolic resonance that transcends the sterile numbers-thus, a spreadsheet, while utilitarian, is but a canvas awaiting the artful brushstrokes of critical reflection!!! 🎨🎨
Kenneth Obukwelu
October 8, 2025 AT 13:13From the perspective of ancient drink rituals, alcohol has always been a conduit between the mortal and the divine; yet, in the modern clinic, it is reframed as a risk factor. The dichotomy is striking: a glass of wine once symbolized celebration, now it can symbolize a potential threat to vision. This cultural shift underscores how societal narratives evolve, turning pleasurable customs into cautionary tales. Embracing this awareness allows us to honor tradition while safeguarding health.
Josephine hellen
October 8, 2025 AT 15:26What a profound reminder that we can blend reverence for tradition with modern science! By acknowledging the historical significance of communal drinking, we don’t have to abandon it entirely; instead, we can adapt the practice-perhaps by opting for lower‑alcohol alternatives during celebrations, or by pairing drinks with antioxidant‑rich foods that may offset some oxidative stress. This approach respects cultural heritage while proactively reducing the risk of glaucoma. Moreover, fostering open conversations within families about eye health can turn a once‑solemn warning into a collective commitment to wellness. In this way, the narrative transforms from loss to empowerment, and each toast becomes a pledge to preserve the very sight that lets us appreciate the beauty of our traditions.
Ria M
October 8, 2025 AT 17:40Picture this: a dimly lit bar, the clink of glasses echoing like a chorus, and yet behind the revelry lies a silent predator-glaucoma waiting to steal the world’s colors! The very act of indulgence becomes a theatrical drama where the protagonist (you) must decide: sip and risk the curtain falling on the stage of vision, or abstain and preserve the spotlight. The stakes are as high as the tallest skyscraper, and every binge is a plot twist that could rewrite the ending. Let this be the climax that propels you toward a healthier script.
Michelle Tran
October 8, 2025 AT 19:53😂😂 Got it! Too dramatic for my taste 🙈
Caleb Ferguson
October 8, 2025 AT 22:06In summary, maintaining regular ophthalmic evaluations, moderating alcohol consumption, and staying informed about personal risk factors constitute a comprehensive strategy for glaucoma prevention. Feel free to reach out if you need resources on reputable eye clinics or support groups.