High-Risk Medications for Seniors: What to Review Now
 Jan, 10 2026
Jan, 10 2026
Every year, tens of thousands of seniors end up in the hospital-not from falls, heart attacks, or infections-but from medications meant to help them. It’s not that these drugs are dangerous for everyone. It’s that aging changes how the body handles them. Kidneys slow down. Liver function dips. Brain sensitivity increases. What was safe at 50 can become risky at 75. And too often, doctors don’t catch it until it’s too late.
What Makes a Medication High-Risk for Seniors?
A medication isn’t high-risk just because it has side effects. It’s high-risk when the danger outweighs the benefit for older adults. The American Geriatrics Society’s Beers Criteria is the gold standard for identifying these drugs. Updated in May 2023, it lists 30 classes of medications and 14 individual drugs that should generally be avoided in people over 65. These aren’t random picks. Each one has solid evidence showing it causes more harm than good in aging bodies.
Think about it this way: a drug that clears through the kidneys might build up in someone with reduced kidney function. A medication that causes drowsiness might make a senior fall. One that blocks acetylcholine-a brain chemical-might blur memory or speed up dementia. These aren’t theoretical risks. They’re real, measurable, and common.
According to the CDC, 40% of seniors take five or more medications daily. That’s polypharmacy-and it’s the biggest driver of bad outcomes. Each extra pill increases the chance of a bad interaction, a side effect, or a mistake. The result? Over $177 billion in preventable hospital costs every year, mostly from drug-related problems.
Top 5 High-Risk Medications Seniors Should Review
Here are five of the most dangerous drugs still commonly prescribed to older adults-and what to ask your doctor instead.
1. Zolpidem (Ambien®)
This sleep aid is everywhere. But for seniors, it’s a fall waiting to happen. Studies show it increases the risk of hip fractures by 2.5 times. Why? The drug lingers in the body longer as we age. Residual drowsiness can last up to 11 hours. That means stumbling in the bathroom at 3 a.m. isn’t bad luck-it’s a side effect.
Patients on zolpidem report sleepwalking, confusion, and memory gaps the next day. Humana members who reported side effects said 68% experienced morning confusion. Over 20% had falls requiring medical care.
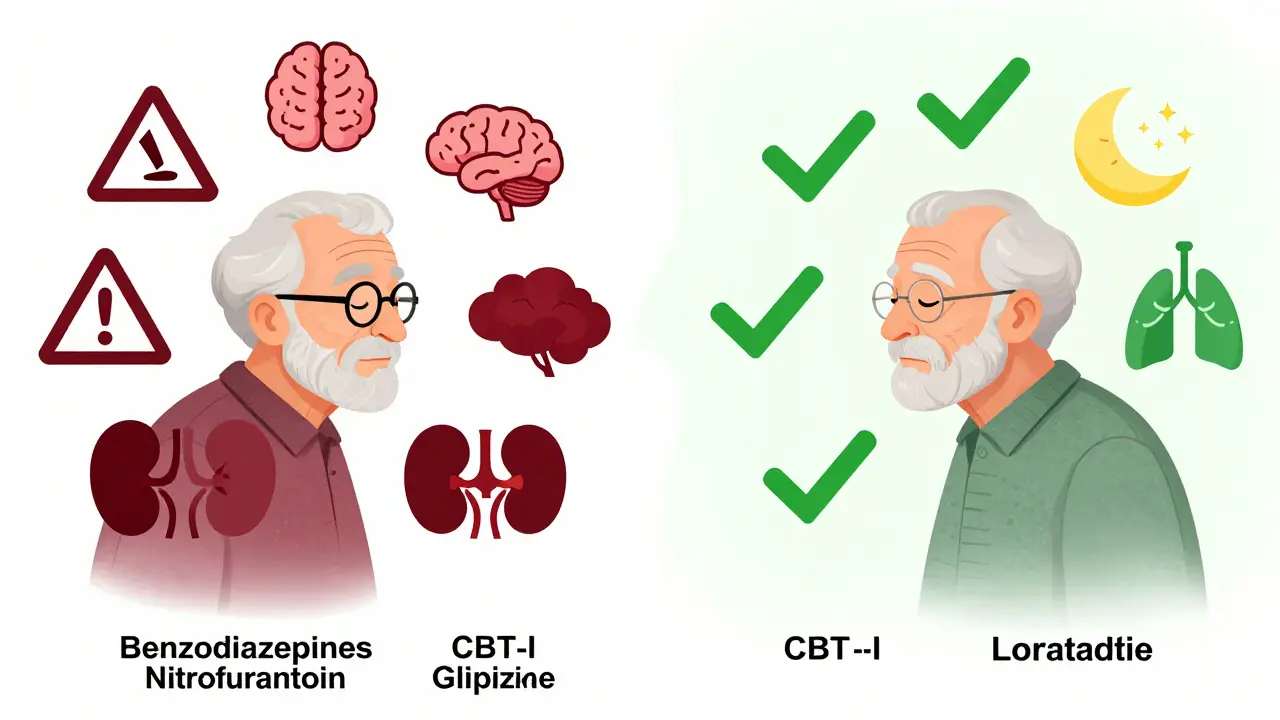
Better alternatives: Trazodone (low dose), cognitive behavioral therapy for insomnia (CBT-I), or melatonin. CBT-I works as well as pills-and lasts longer without the risks.
2. Glyburide (Diabeta®)
It’s an old diabetes drug. Cheap. Easy to prescribe. And deadly for seniors. Glyburide causes low blood sugar more often than other sulfonylureas. In older adults, it triggers hypoglycemia in nearly 30% of users-compared to just 13% with glipizide. That means fainting, confusion, seizures, or even coma.
CMS data shows glyburide leads to 4.2 emergency visits per 100 patients every year. The FDA added a boxed warning in 2023. That’s the strongest warning they give.
Better alternatives: Glipizide, metformin, or GLP-1 agonists like semaglutide. These are safer, more predictable, and even help with weight loss.
3. Diphenhydramine (Benadryl®)
This antihistamine is in every cold medicine, sleep aid, and allergy pill. But it’s also a powerful anticholinergic. That means it blocks a brain chemical essential for memory and focus. Cumulative use over a year increases dementia risk by 54%, according to a landmark JAMA study. A score of 3 on the Anticholinergic Cognitive Burden scale? That’s the highest risk level.
Seniors on diphenhydramine report dry mouth, constipation, blurred vision, and mental fogginess. One 78-year-old woman on it for neuropathy ended up hospitalized for severe constipation-until she switched to duloxetine.
Better alternatives: Loratadine (Claritin®), cetirizine (Zyrtec®), or non-sedating nasal sprays. For sleep, try melatonin or a warm bath instead.
4. Nitrofurantoin (Macrobid®)
This antibiotic is often used for urinary tract infections. But if kidney function drops below 60 mL/min-which is common in seniors-it becomes toxic. The body can’t clear it properly. That leads to lung damage: coughing, shortness of breath, even death. Mortality from acute reactions hits 18.3%.
Buckeye Health Plan’s data shows it’s 12.8 times more likely to cause lung injury in seniors with kidney disease than in younger patients. Yet, it’s still prescribed routinely.
Better alternatives: Nitrofurantoin should be avoided if eGFR is under 60. Use fosfomycin, cephalexin, or amoxicillin-clavulanate instead. Always check kidney function before prescribing.
5. Benzodiazepines (Lorazepam, Diazepam)
These are anti-anxiety and sleep meds. But they’re also sedatives that slow reaction time, impair balance, and increase fall risk by 82%. For seniors who drive, the crash risk jumps 48%. Long-term use is linked to a 50% higher death rate over five years.
Reddit threads from families caring for elderly relatives are full of stories: “Mom took Ativan and didn’t wake up for 24 hours.” “Dad got confused and wandered off.”
Better alternatives: SSRIs for anxiety, CBT-I for sleep, or non-drug approaches like mindfulness or light therapy. If you must use one, limit it to a few days-not weeks or months.
What You Can Do Right Now
You don’t need to wait for your next appointment. Start now.
- Do a “brown bag” review: Take every pill, supplement, and OTC med you take to your doctor or pharmacist. Include creams, patches, and eye drops.
- Ask: “Is this still necessary?” Many drugs are prescribed for short-term use but kept for years.
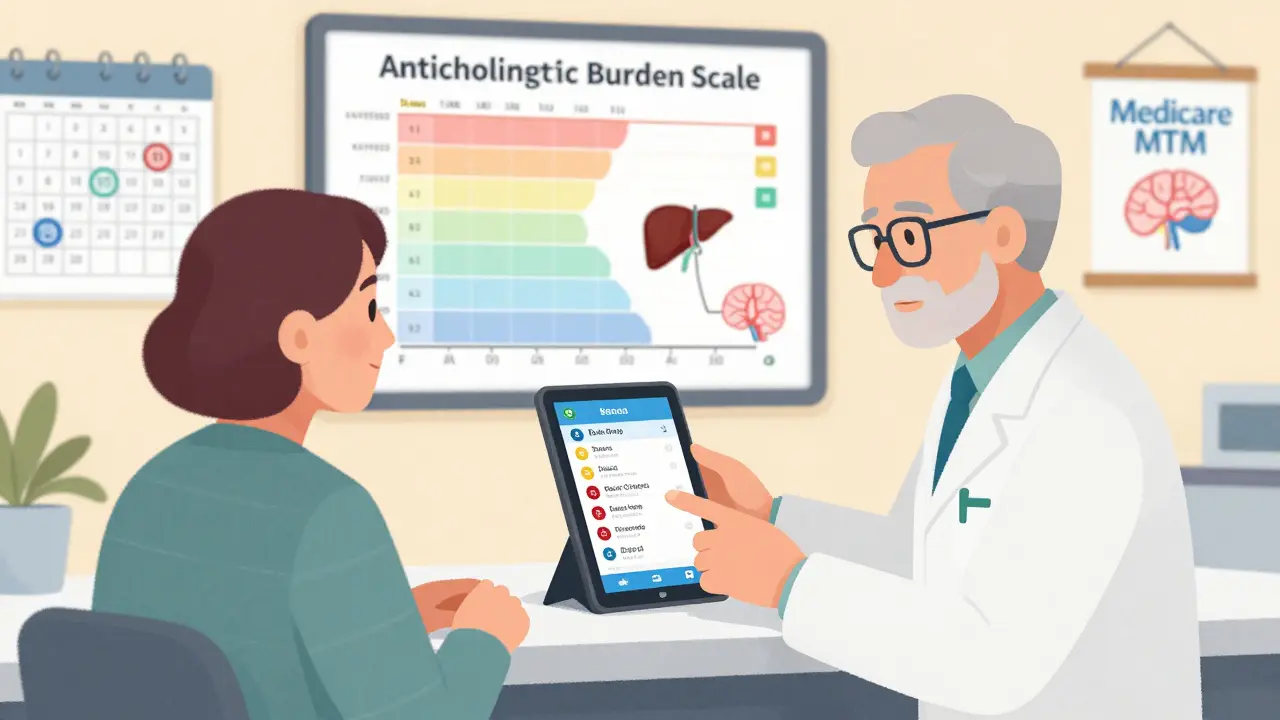
- Check the Anticholinergic Burden: If you’re taking more than one drug with anticholinergic effects (like diphenhydramine, oxybutynin, or amitriptyline), your risk is stacking up. Use the ACB scale to see your total score.
- Request a medication review: Medicare covers annual Medication Therapy Management (MTM) for people on multiple drugs. Ask your pharmacist if you qualify.
- Use the Beers Criteria checklist: Download the 2023 list from the American Geriatrics Society website and bring it to your visit.
Don’t stop any medication on your own. But do ask: “Is there a safer option?”
How Doctors Are Changing Their Approach
Things are shifting. In 2023, 87% of primary care physicians used electronic alerts in their systems to flag Beers Criteria drugs. Epic and Cerner now auto-flag high-risk prescriptions for seniors. Pharmacists are stepping into the role of medication safety managers.
Pharmacist-led reviews reduce high-risk drug use by over 34% within six months. Medicare Advantage plans now tie 5% of their quality bonuses to reducing these prescriptions. The system is finally catching up.
But change starts with you. If your doctor prescribes something new, ask: “Is this on the Beers list? Is there a better choice for someone my age?”
Common Myths About Senior Medications
- Myth: “If it’s over-the-counter, it’s safe.”
Truth: Diphenhydramine, ibuprofen, and even melatonin can be risky in seniors. OTC doesn’t mean harmless. - Myth: “I’ve been on this for years, so it must be fine.”
Truth: Aging changes your body. What worked at 60 might be dangerous at 75. - Myth: “My doctor knows best-I shouldn’t question them.”
Truth: Your doctor wants you to be safe. Asking questions shows you’re engaged, not difficult.
Medication safety isn’t about cutting pills. It’s about choosing the right ones. It’s about quality of life-not just survival.
When to Call for Help
Call your doctor immediately if you or a loved one experiences:
- Sudden confusion or memory loss
- Falls or dizziness without obvious cause
- Extreme fatigue or weakness
- Constipation or urinary retention
- Slurred speech or unsteady walking
These aren’t normal aging signs. They’re red flags for medication toxicity.
What is the Beers Criteria and why does it matter for seniors?
The Beers Criteria is a list of medications that are potentially inappropriate for older adults, updated every two years by the American Geriatrics Society. It’s based on clinical evidence showing which drugs increase fall risk, confusion, kidney stress, or other side effects in seniors. Over 98% of Medicare Advantage plans use it to shape their drug coverage. If a medication is on the list, it means the risks usually outweigh the benefits for people over 65.
Can I stop taking a high-risk medication on my own?
No. Stopping some medications suddenly-like benzodiazepines or certain antidepressants-can cause dangerous withdrawal symptoms. Always talk to your doctor or pharmacist first. They can help you taper off safely or switch to a better alternative.
Are natural supplements safer than prescription drugs for seniors?
Not necessarily. Supplements like kava, valerian, or high-dose melatonin can interact with medications or cause drowsiness and falls. Many aren’t tested for safety in older adults. Always tell your doctor what supplements you’re taking-even if you think they’re harmless.
How often should seniors have their medications reviewed?
At least once a year, but quarterly is better if you take five or more medications. Medicare offers free Medication Therapy Management (MTM) services for eligible beneficiaries. Ask your pharmacist or doctor if you qualify.
What should I bring to a medication review appointment?
Bring all your medications in their original bottles-including prescriptions, over-the-counter drugs, vitamins, and supplements. Include patches, eye drops, and inhalers. Write down when and why you take each one. This helps your provider spot duplicates, interactions, or unnecessary drugs.
Are there apps or tools to check if my meds are high-risk?
Yes. Apps like Medscape’s Beers Criteria Checker or the American Geriatrics Society’s mobile tool let you search drugs by name and see if they’re flagged for seniors. Many pharmacy apps now show Beers alerts when you fill a prescription. Ask your pharmacist to run a check during your next refill.
Final Thought: It’s Not About Taking Less-It’s About Taking Better
Seniors don’t need fewer pills. They need smarter ones. A single, well-chosen medication can do more than five risky ones. The goal isn’t to eliminate all drugs-it’s to remove the ones that do more harm than good. And that starts with asking questions, doing a brown bag review, and trusting your instincts when something feels off.
Medication safety isn’t a one-time checkup. It’s an ongoing conversation-with your doctor, your pharmacist, and yourself. Because when you’re older, every pill matters more than ever.
Alfred Schmidt
January 11, 2026 AT 13:50Why is this even a discussion? I’ve seen 80-year-olds on Ambien, Benadryl, and Ativan like it’s candy-and then wonder why they’re falling, confused, or in the ER. This isn’t ‘risk management’-it’s medical negligence dressed up as guidelines. The Beers Criteria? It’s a joke if doctors aren’t forced to follow it. My dad died because his ‘care team’ refused to wean him off glyburide. They said ‘it’s working.’ Working? He was in a coma for three days. No one’s accountable. Fix the system, not just the list.
Sean Feng
January 13, 2026 AT 07:03Most of these drugs are outdated. Doctors just prescribe them because they’re cheap and easy. No one wants to do the work of finding alternatives.
Priscilla Kraft
January 14, 2026 AT 10:02This is so important 🙏 I just helped my 79-year-old neighbor do a brown bag review last week-she was on 11 meds, including diphenhydramine for sleep and nitrofurantoin despite her eGFR being 48. We switched her to melatonin, loratadine, and cephalexin. She’s been sleeping better, walking steadier, and even started gardening again. It’s not magic-it’s just listening to the body. Pharmacist-led reviews should be standard, not optional. Seriously, if you’re over 65 and on 5+ meds, don’t wait for your annual visit-go now. You deserve to feel like yourself again 💛
Christian Basel
January 15, 2026 AT 17:42The pharmacokinetic and pharmacodynamic alterations associated with geriatric physiology necessitate a reevaluation of polypharmacy paradigms. The Beers Criteria, while empirically derived, lacks granular stratification for frailty indices and comorbidities. Consequently, blanket avoidance of Class II anticholinergics may inadvertently deprive patients of clinically beneficial agents in the absence of individualized risk-benefit analysis. Furthermore, the economic incentive structure within Medicare Advantage creates perverse alignment with deprescribing metrics, potentially compromising therapeutic continuity.
Priya Patel
January 16, 2026 AT 07:49OMG I just realized my mom’s been taking Benadryl every night for years because she said it "helps her relax"-and now she’s always foggy and constipated 😭 I’m taking her to the pharmacist tomorrow. This post saved me from being one of those kids who just lets it slide. Thank you so much for this 🙌 I’m sharing it with everyone in my family group chat!
Jason Shriner
January 17, 2026 AT 03:12So let me get this straight… we’re gonna stop giving old people meds because they might fall? Next they’ll ban stairs and coffee. Next thing you know, we’ll be giving them oatmeal and rocking chairs and calling it "healthcare." At least the drugs made them feel something. Now they’ll just sit there, confused and bored, wondering why their grandkids won’t visit. Progress.
Sam Davies
January 18, 2026 AT 06:30How quaint. The Beers Criteria, a product of American geriatric bureaucracy, now masquerades as moral authority. In Europe, we don’t infantilize the elderly with checklist-driven deprescribing. We trust their autonomy-even if they choose to take diphenhydramine with their whisky. Perhaps the real issue isn’t the drugs, but the cultural fear of aging. Let them sleep. Let them stumble. Let them be human.
Michael Patterson
January 19, 2026 AT 13:44Look, I get it, but people don’t just wake up one day and say "I’m gonna start taking 10 meds." It’s a slow creep. Doctor says "try this for your joint pain," then "this for your anxiety," then "this for the insomnia," then "this for the reflux," then "this for the dry eyes," then "this for the constipation from the last med." And suddenly you’re on 12 pills. And now you’re told to stop half of them? Good luck. Half of these seniors don’t even know what half their meds are for. Their kids don’t know. Their doctors don’t know. And now you want them to audit their own pharmacy? It’s not laziness-it’s systemic collapse. We need a national medication navigator program. Like a tax guy, but for pills. Someone who just sits down with you, checks everything, and says "this one’s trash, this one’s fine, this one’s a bomb." Until then? We’re just yelling into the void.
Matthew Miller
January 20, 2026 AT 00:57Stop pretending this is about safety. This is about cost-cutting disguised as compassion. Medicare saves billions by pushing seniors off glyburide and nitrofurantoin-not because those drugs are dangerous, but because the alternatives are expensive. GLP-1 agonists cost $1,000/month. Trazodone? $4. Who benefits? The pharmaceutical industry. The patients? They’re collateral damage. The Beers Criteria is corporate policy dressed in white coats. And you’re all just nodding along like good little sheep.
Madhav Malhotra
January 20, 2026 AT 10:01As someone from India, I’ve seen how families here handle elder care-no one takes 10 pills alone. Someone’s always there: a daughter, a grandson, a neighbor. They check the bottles, remind when to take it, notice if someone’s dizzy. Here in the U.S., elders are left alone with a pharmacy bag full of mystery pills. Maybe the real solution isn’t just changing meds-it’s changing how we care. We need community. We need people who notice. Not just algorithms and checklists.
Jennifer Littler
January 22, 2026 AT 09:58As a clinical pharmacist who runs MTM sessions for Medicare Advantage patients, I see this daily. Last week, I identified 4 patients on nitrofurantoin with eGFR < 45. One had interstitial lung fibrosis confirmed by CT. All were prescribed by PCPs who didn’t check labs in 2 years. The system is broken. But here’s the good news: when you sit down with a patient and say "Let’s look at this together," 90% are relieved. They’ve been scared to ask. We replaced 23 high-risk meds in one month. Not because we’re heroes-we just took the time. MTM is free. Ask for it. Seriously. It’s there. You just have to say "I want a med review."
Vincent Clarizio
January 23, 2026 AT 23:47Let’s not pretend this is about medicine. This is about control. The Beers Criteria is a tool of institutional paternalism-telling seniors what they can and can’t take because they’re too "fragile" to decide. But here’s the irony: the people who need these meds most are often the ones who’ve lived through wars, raised kids, buried spouses, and kept going. Now we tell them: "You’re too old for this. We know better." Meanwhile, we’re fine giving 25-year-olds opioids for back pain and antidepressants for existential dread. Why? Because youth is sacred. Age is a liability. We don’t want to see the truth: that aging isn’t a disease to be managed-it’s a life to be honored. And sometimes, that means letting someone take their Ambien. Let them sleep. Let them be. Not because it’s safe-but because it’s theirs.