Hemochromatosis: How Iron Overload Damages Your Liver and How Phlebotomy Fixes It
 Nov, 29 2025
Nov, 29 2025
Most people think too much iron is a good thing - maybe you’ve heard that iron boosts energy or helps with fatigue. But when your body can’t get rid of excess iron, it starts poisoning your organs. That’s hemochromatosis. It’s not rare. In the U.S., about 1 in 200 people of Northern European descent carry two copies of the faulty HFE gene that causes it. And most don’t know they have it until their liver, heart, or pancreas is already damaged.
What Exactly Is Hemochromatosis?
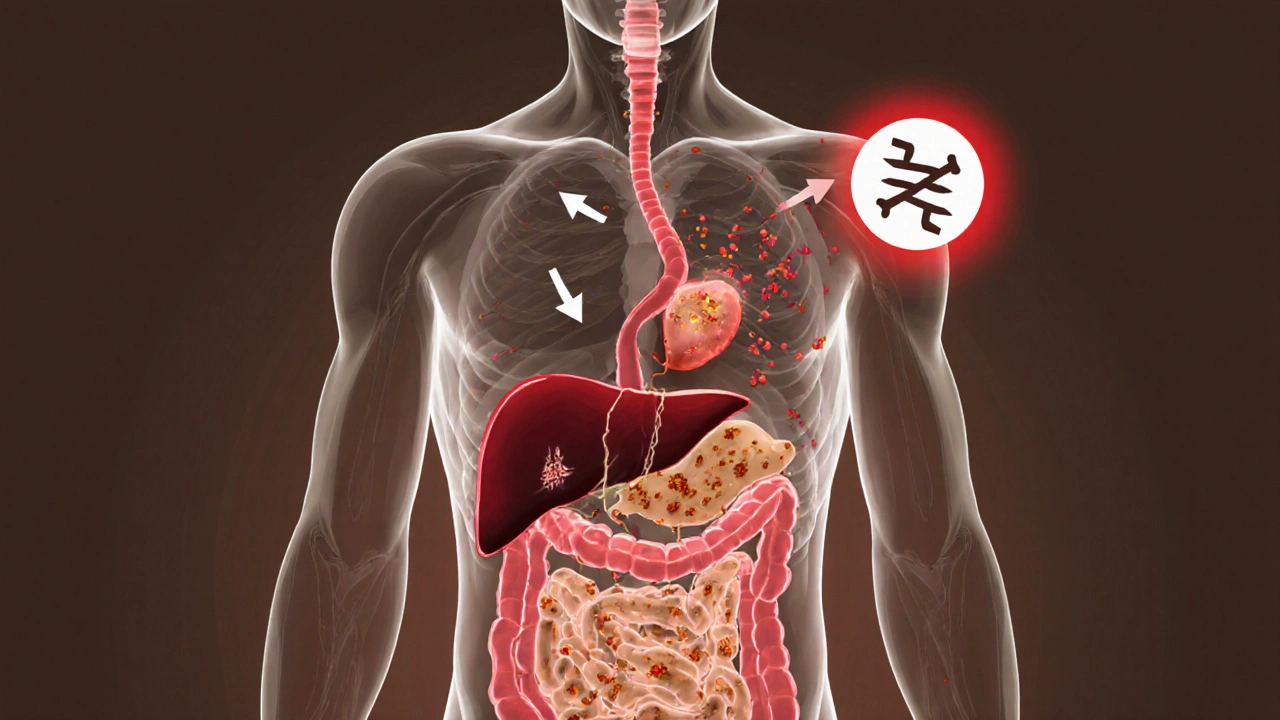
Hemochromatosis is a genetic disorder where your body absorbs way too much iron from food - even when you don’t need it. Normally, your gut stops absorbing iron once you’ve had enough. In hemochromatosis, that brake fails. The liver hormone hepcidin doesn’t work right, so iron keeps pouring into your bloodstream. Over time, that iron builds up like rust inside your organs.
It’s not caused by eating too much red meat or taking iron supplements. Even people who eat a normal diet end up with dangerously high iron levels. The main culprit? A mutation in the HFE gene, specifically the C282Y variant. About 80-95% of diagnosed cases come from having two copies of this mutation. It’s inherited - you get one copy from each parent. If you only have one, you’re a carrier and usually fine. But two copies? That’s when the trouble starts.
Why Your Liver Takes the First Hit
The liver is ground zero for iron overload. It’s the main storage site, and when it gets flooded, it can’t handle the stress. Iron doesn’t just sit there quietly - it generates free radicals that attack liver cells. Over years, this leads to inflammation, scarring, and eventually cirrhosis. By the time someone’s ferritin level hits 1,000 ng/mL, there’s a 50-75% chance they already have liver damage.
That’s why so many people with hemochromatosis are diagnosed after they’re sent to a liver specialist for elevated liver enzymes. But here’s the catch: early on, there are no symptoms. No jaundice. No pain. Just subtle signs like constant tiredness, joint aches, or loss of sex drive. These get written off as stress, aging, or depression. By the time the liver shows up on an ultrasound as scarred, it’s often too late to reverse it.
How You Know You Have It - Before It’s Too Late
Two simple blood tests can catch hemochromatosis before your liver fails: transferrin saturation and serum ferritin.
Transferrin saturation tells you how much iron is floating in your blood. Normal is under 45%. If it’s over 45%, that’s a red flag. Ferritin measures stored iron. In men, anything over 300 ng/mL is suspicious. In women, over 200 ng/mL. These numbers aren’t just markers - they’re warning signs.
Doctors rarely order these tests unless you’re clearly sick. But if you’re a man over 30 with unexplained fatigue, joint pain, or diabetes - get tested. If you have a family member with hemochromatosis, you should be screened. Genetic testing for HFE mutations confirms it. And it’s cheap now - $150 to $300 - far less than a liver biopsy.
Phlebotomy: The Simple, Free Treatment That Saves Lives
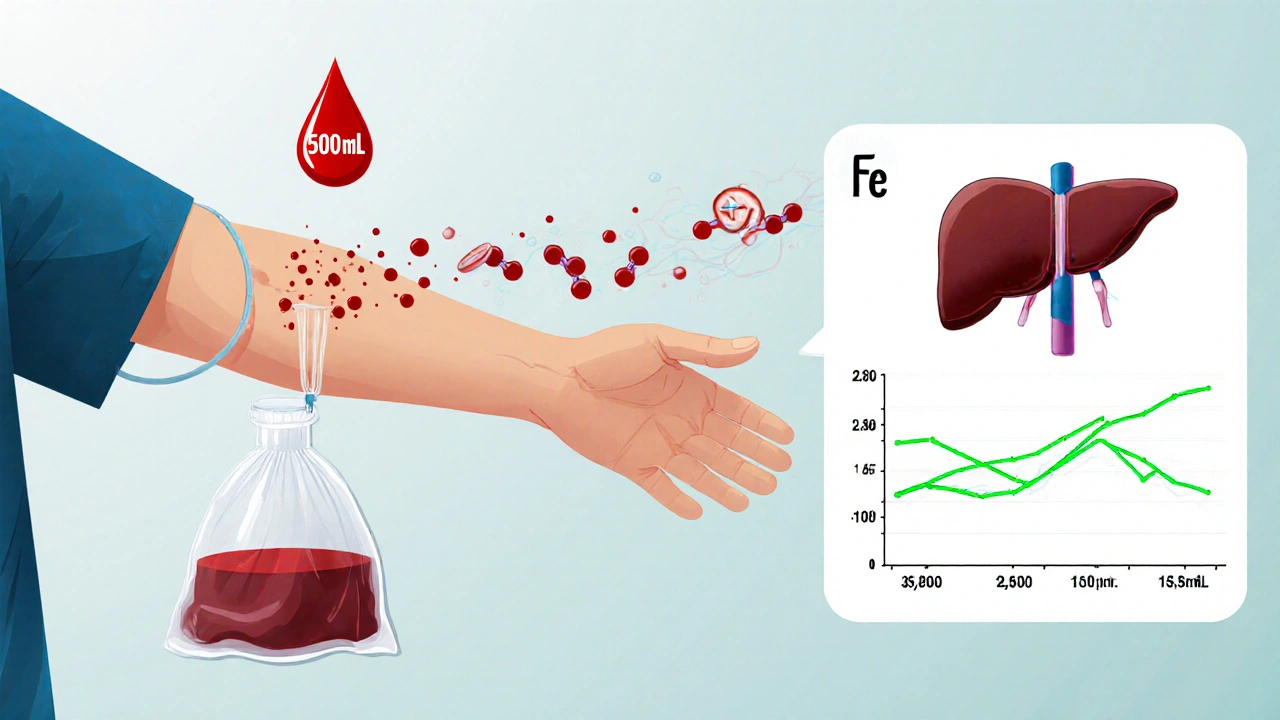
The treatment? Remove the iron. Not with pills. Not with fancy drugs. Just by taking blood out - the same way you donate blood.
This is called therapeutic phlebotomy. Each session removes about 500 mL of blood - and with it, 200 to 250 mg of iron. That’s the same amount of iron your body absorbs in a whole month. You start with weekly sessions until your ferritin drops to 50-100 ng/mL. For someone with ferritin at 2,500, that might take 50 sessions over 18 months.
It sounds brutal, but patients say it’s life-changing. Once the iron drops, energy returns. Joint pain fades. Skin color lightens. Diabetes becomes easier to control. One patient on Reddit said he needed 62 phlebotomies over 15 months. Afterward, he said, “I felt like I was 25 again.”
And here’s the best part: it’s covered by insurance. Most places charge $0 to $50 per session. Compare that to iron chelation drugs, which cost $25,000 to $35,000 a year and come with nasty side effects. Phlebotomy is the gold standard - simple, safe, and effective.
What Happens If You Don’t Treat It?
Untreated hemochromatosis doesn’t just hurt your liver. Iron piles up in your pancreas and causes diabetes. It builds up in your heart and leads to arrhythmias or heart failure. It knocks out your pituitary gland and causes low testosterone - which is why many men lose their sex drive and muscle mass.
And then there’s the cancer risk. If you develop cirrhosis from iron overload, your chance of liver cancer jumps 20-fold. One study found that patients diagnosed after ferritin hit 1,000 ng/mL had only a 60% survival rate over 10 years. But if caught early - before organ damage - survival is nearly 100%.
That’s why timing matters. The earlier you start phlebotomy, the better your outcome. If you’re diagnosed before age 40 and begin treatment, you can live a normal lifespan. Wait until you’re 60 with cirrhosis? Your life expectancy drops sharply.

Life After Diagnosis: The Long Game
Once you’ve cleared the excess iron, you’re not done. Maintenance is key. You’ll need phlebotomy every few months - usually 4 to 6 times a year - to keep ferritin in the 50-100 ng/mL range. Skip sessions? Iron creeps back. Within a year, you’re back at risk.
But here’s the problem: most patients stop after their symptoms go away. They think, “I feel fine now,” and quit. That’s a mistake. Iron doesn’t vanish - it just stops building up. If you stop treatment, it starts accumulating again. You’re not cured. You’re managing a lifelong condition.
Some struggle with vein access. Older patients or those who’ve had many phlebotomies find their veins harder to hit. Others can’t get appointments - not all blood centers do therapeutic phlebotomy. Talk to your doctor. They can write a prescription and help you find a clinic that accepts it.
And don’t forget your diet. Avoid iron supplements. Don’t take vitamin C with meals - it boosts iron absorption. Limit alcohol - it worsens liver damage. Eat normally, but skip iron-fortified cereals and red meat if your levels are still high.
Who Should Get Tested?
You don’t need to wait for symptoms. If any of these apply to you, get tested:
- You’re of Northern European descent (Irish, Scottish, Welsh, Scandinavian)
- You have a parent, sibling, or child with hemochromatosis
- You have unexplained fatigue, joint pain, or erectile dysfunction
- Your liver enzymes are high for no clear reason
- You’ve been diagnosed with type 2 diabetes without obesity
- You’re a man over 30 with no obvious cause for low energy
And if you’re diagnosed? Tell your family. First-degree relatives have a 25% chance of having two faulty copies. Screening them could prevent liver failure in your siblings or children.
The Future: New Treatments on the Horizon
Phlebotomy works, but it’s not perfect. That’s why researchers are working on alternatives. One drug, PTG-300, mimics hepcidin - the hormone your body should be making. Early trials show it lowers iron levels without needing blood draws. It’s not available yet, but it’s coming.
Another advance? MRI scans can now measure liver iron precisely without a biopsy. That means less invasive monitoring and better tracking of treatment progress.
But the biggest breakthrough isn’t a drug or machine. It’s awareness. Most doctors still don’t test for transferrin saturation. If you’re tired and your doctor says, “It’s just stress,” ask: “Could it be hemochromatosis?”
Can you get hemochromatosis from eating too much red meat?
No. Hemochromatosis is genetic. You can’t get it from diet. But eating a lot of red meat or taking iron supplements can make the iron overload worse if you already have the gene mutation. The problem isn’t how much iron you eat - it’s that your body absorbs too much of it, whether you eat a lot or a little.
Is phlebotomy the same as donating blood?
Yes, medically it’s the same procedure - 500 mL of blood removed from a vein. The difference is why it’s done. Blood donation is for others; therapeutic phlebotomy is for your health. Most blood banks won’t accept your blood if you have hemochromatosis, so you’ll need to go to a hospital or clinic that does therapeutic treatments. But the process is identical.
Can women get hemochromatosis too?
Yes, but they’re usually diagnosed later. Before menopause, women lose iron through monthly periods, which delays iron buildup. After menopause, their iron levels rise quickly. Women often don’t show symptoms until their 50s or 60s, but they’re just as likely to develop liver damage, diabetes, or heart problems if untreated.
Does everyone with the HFE gene mutation get sick?
No. Only about 1 in 4 people with two copies of the C282Y mutation develop serious symptoms. Some never have any problems. But we don’t know who will get sick - so if you have the gene, you’re still at risk. Doctors recommend monitoring ferritin levels and starting phlebotomy if levels rise above normal, even if you feel fine.
Can you reverse liver damage from hemochromatosis?
Early scarring can improve with treatment. If you start phlebotomy before cirrhosis develops, your liver can heal. But once cirrhosis is advanced - with nodules and hardened tissue - it’s permanent. The good news? Stopping further iron buildup prevents cancer and liver failure. Even with cirrhosis, treatment extends life and reduces complications.
If you’ve been told you’re just “tired” or “getting older,” and you have a family history or unexplained symptoms - don’t wait. Ask for a ferritin test. It’s quick. It’s cheap. And it could save your liver - and your life.
Sohini Majumder
November 30, 2025 AT 22:58tushar makwana
December 1, 2025 AT 21:54Richard Thomas
December 2, 2025 AT 01:41Peter Lubem Ause
December 2, 2025 AT 21:41linda wood
December 4, 2025 AT 05:43LINDA PUSPITASARI
December 4, 2025 AT 06:55gerardo beaudoin
December 5, 2025 AT 06:08Joy Aniekwe
December 5, 2025 AT 19:05Latika Gupta
December 5, 2025 AT 20:36