Future of Vertigo Treatment: New Research & Tech Advances
 Oct, 20 2025
Oct, 20 2025
Vertigo Treatment Comparison Tool
Compare Vertigo Treatment Options
Select the treatment approach you're interested in to see how it compares to current standards based on key criteria important to your care.
Current Standard Care
Traditional treatments that are widely available in clinics today.
Emerging Approaches
Newer treatments that are in development or recently approved.
Comparison Criteria
Speed of Relief
Long-term Efficacy
Side Effects
Accessibility
Cost (US)
Next Steps
Ask your clinician about these treatment options and whether they're right for your specific situation.
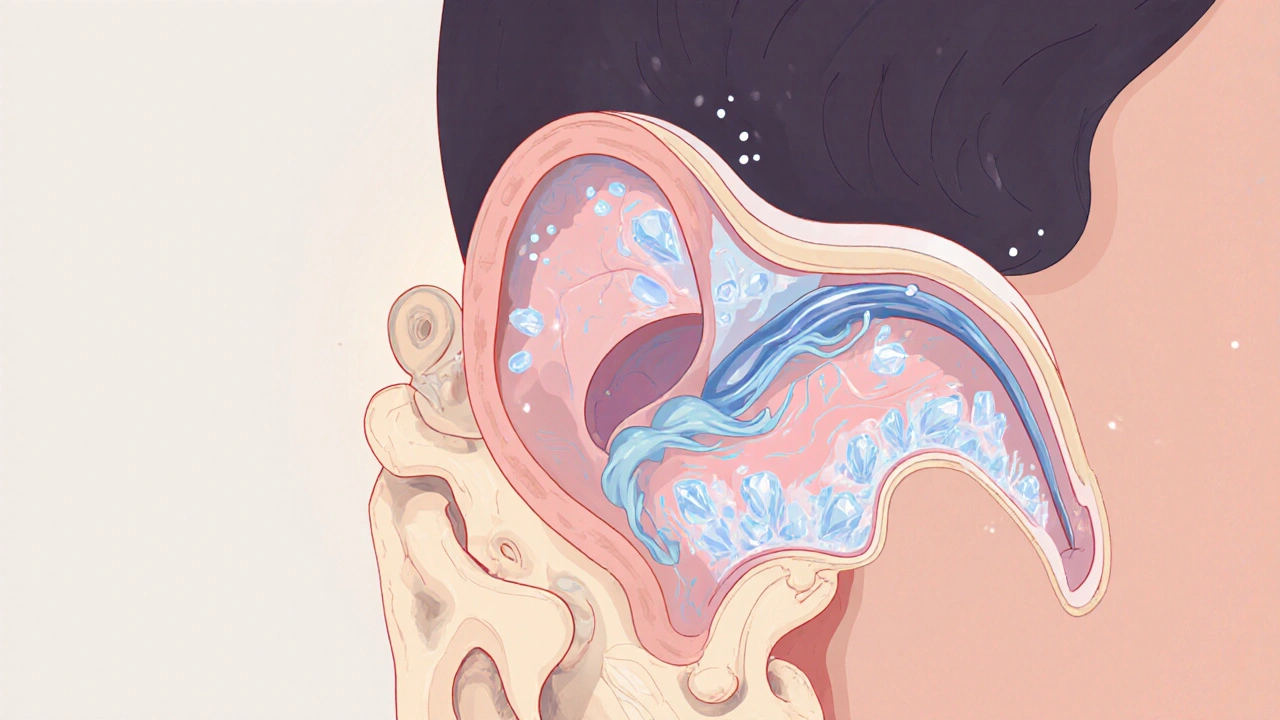
When talking about Vertigo is a sensation of spinning or moving that arises from problems in the inner ear or brain pathways that control balance, most people picture a dizzy spell that fades after a few minutes. Yet for the millions who suffer chronic episodes, the impact is far more severe: missed work, unsafe driving, and a constant fear of falling. The good news is that the next decade promises a wave of research and technology that could change how clinicians diagnose and treat this disorder. Below you’ll find a clear roadmap of where vertigo care is headed, the science behind the breakthroughs, and practical tips you can use right now.
Why vertigo matters today
Even though vertigo is often dismissed as just “a funny feeling,” it is the most common balance disorder worldwide. According to a 2023 epidemiological study, about 5% of adults report chronic vertigo symptoms, and the prevalence climbs to 15% among seniors. The condition accounts for roughly 2.5 million emergency‑room visits in the U.S. each year, costing the healthcare system over $4 billion in direct expenses. These numbers highlight the urgent need for better solutions - not just symptom relief, but lasting restoration of equilibrium.
Current standard of care
Today’s toolbox includes three main approaches:
- Medication: antihistamines, anticholinergics, and vestibular suppressants such as meclizine. They work fast but can cause drowsiness and don’t address the underlying cause.
- Canalith Repositioning Maneuver (Canalith Repositioning Maneuver is a series of head‑position changes designed to move displaced otoconia out of the semicircular canals and back into the utricle), most famously the Epley technique. Ideal for benign paroxysmal positional vertigo (BPPV), it offers quick resolution in 70‑90% of cases.
- Vestibular Rehabilitation Therapy (Vestibular Rehabilitation Therapy is a customized exercise program that trains the brain to compensate for vestibular loss by improving gaze stability, gait, and balance). It’s the go‑to for unilateral vestibular hypofunction and persistent disequilibrium after an acute episode.
While these methods help many, a sizable minority remain symptomatic, prompting researchers to look beyond symptom control.
Emerging drug delivery platforms
Science is moving toward targeted therapies that act directly on the inner‑ear structures. One promising avenue is nanocarrier‑based delivery of betahistine-a vasoactive agent that increases inner‑ear blood flow. Early phase‑II trials show a 35% improvement in dizziness scores when the drug is encapsulated in liposomal particles that cross the round‑window membrane more efficiently than oral pills.
Another contender is low‑dose gentamicin injection for Ménière’s disease. By fine‑tuning the dose with computer‑guided micro‑infusion, clinicians achieve vertigo control in up to 80% of patients while preserving hearing in 70% of cases-a dramatic improvement over traditional ablative surgery.
Neuromodulation: electrical signals to reset balance
The vestibular nerve can be stimulated with precision‑controlled currents, a technique known as Neuromodulation which uses implanted or surface electrodes to recalibrate abnormal signaling pathways. A 2024 multicenter study on vestibular implant prototypes reported a 60% reduction in vertigo frequency after six months, with patients regaining confidence in walking unaided. Researchers are now integrating AI algorithms to adapt stimulus patterns in real time, turning a static implant into a smart balance regulator.

Artificial intelligence and diagnostic imaging
Diagnosing the exact cause of vertigo often requires time‑consuming specialist assessment and imaging. AI‑driven analysis of high‑resolution MRI scans now highlights subtle lesions in the vestibular organs that human radiologists may miss. In a blinded test of 1,200 scans, the algorithm correctly identified vestibular schwannomas with 96% accuracy, cutting diagnostic time from weeks to days.
Beyond imaging, wearable sensors that capture head‑velocity and eye‑movement data are feeding machine‑learning models that can classify vertigo sub‑types on the spot. These apps already help emergency doctors decide whether a patient needs a CT scan or can be safely discharged with vestibular rehab.
Virtual reality (VR) as a therapeutic platform
VR isn’t just for gaming; it’s becoming a powerful tool for vestibular rehab. The Virtual Reality Therapy immerses patients in controlled visual environments that challenge balance while providing instant feedback. A 2023 randomized trial showed that VR‑based rehab improved gait speed by 18% compared with traditional exercises, and patients reported higher enjoyment, leading to better adherence.
Next‑gen headsets equipped with built‑in inertial measurement units will allow clinicians to monitor progress remotely, turning home‑based therapy into a data‑rich experience.
Wearable balance sensors and tele‑rehab
Smart earbuds and lightweight bands now include gyroscopes that continuously track orientation. When paired with a cloud platform, these devices alert users to early signs of imbalance and suggest corrective exercises. Early adopters claim fewer falls and a sense of empowerment, especially seniors living alone.
Tele‑rehab platforms integrate these sensors with video calls, enabling therapists to observe real‑time performance and adjust programs without an in‑person visit. Insurance providers are beginning to reimburse such remote sessions, widening access.

Comparison of current vs. emerging vertigo treatments
| Aspect | Current Standard | Emerging Approach |
|---|---|---|
| Speed of relief | Hours‑to‑days (meds, repositioning) | Minutes‑hours (targeted nanodrugs, neuromodulation) |
| Long‑term efficacy | 30‑40% relapse within 6 months | Up to 80% sustained control (implants, AI‑guided rehab) |
| Side‑effects | Sedation, ototoxicity | Minimal with localized delivery; device‑related rare adverse events |
| Accessibility | Widely available in clinics | Growing via tele‑health and wearable platforms |
| Cost (US) | $150‑$500 per episode | Projected $1,000‑$3,000 for implant or AI‑diagnostic package (insurance‑covered soon) |
What patients can expect in the next five years
Here’s a realistic timeline based on ongoing clinical trials and FDA pipelines:
- 2025‑2026: FDA clearance for liposomal betahistine eye‑drops; broader insurance coverage for vestibular rehab apps.
- 2027‑2028: First‑generation vestibular implants enter the market with AI‑adaptive algorithms.
- 2029‑2030: Integrated VR‑rehab platforms become standard in outpatient clinics; remote monitoring via wearables becomes reimbursable.
While not every patient will need a high‑tech implant, the ecosystem will offer more personalized options, allowing you to choose a path that matches your severity, lifestyle, and budget.
Practical checklist for anyone seeking vertigo care
- Get a comprehensive vestibular assessment - includes video‑head‑impulse test and audiometry.
- Ask about vertigo treatment options beyond pills; mention the latest nanodrug trials if you qualify.
- Consider a trial of Canalith Repositioning Maneuver with a certified therapist before jumping to medication.
- If symptoms persist >3 months, discuss vestibular rehabilitation and whether a VR‑based program is available.
- Check if your insurer covers tele‑rehab or wearable sensors; many plans are updating policies for 2025.
- Stay informed about clinical trials near you - registries like ClinicalTrials.gov list ongoing studies on neuromodulation and AI diagnostics.
Key takeaways
- Vertigo affects millions and carries high personal and economic costs.
- Standard care works for many but leaves a gap for chronic sufferers.
- Targeted drug delivery, neuromodulation implants, AI‑driven diagnostics, and VR rehab are reshaping the landscape.
- Within the next decade, patients will have choices that are faster, safer, and more personalized.
- Stay proactive: ask your clinician about emerging options and consider participating in research.
What is the most common cause of vertigo?
Benign paroxysmal positional vertigo (BPPV), caused by displaced otoconia in the semicircular canals, accounts for roughly 20‑30% of all vertigo cases.
Can vertigo be cured without medication?
Yes. Canalith repositioning maneuvers and vestibular rehabilitation can eliminate symptoms in many patients, especially those with BPPV or unilateral vestibular hypofunction.
Are vestibular implants safe?
Early studies show a favorable safety profile; most adverse events are mild and related to the surgical procedure. Ongoing trials are refining electrode design to further reduce risk.
How does virtual reality help with balance?
VR creates controlled visual‑vestibular challenges that stimulate the brain’s compensation mechanisms. Real‑time feedback improves gait and reduces dizziness faster than standard exercises.
Is AI diagnosis covered by insurance?
Coverage varies by provider, but several insurers have started reimbursing AI‑assisted vestibular imaging under advanced diagnostic services as of 2025.
Andrew Hernandez
October 20, 2025 AT 14:18Thanks for the overview. It highlights key advances.
Demetri Huyler
October 25, 2025 AT 09:30While some celebrate incremental tweaks, the true breakthrough demands bold vision. Our nation's research labs have been pioneering vestibular implants long before anyone else, and the data proves it. The future will be ours if we keep funding homegrown talent.
Wesley Humble
October 30, 2025 AT 03:42The presented roadmap, though comprehensive, omits critical pharmacokinetic considerations inherent to inner‑ear drug delivery. Liposomal encapsulation, for instance, introduces variable particle size distributions that directly affect round‑window permeability. Moreover, the cited Phase‑II outcomes lack stratification by age brackets, a factor known to modulate vascular reactivity. Without such granularity, clinicians cannot tailor dosing protocols with the precision that modern therapeutics demand. Neuromodulation studies, while promising, suffer from heterogeneous electrode placement methodologies that compromise reproducibility. The algorithmic adaptation described in the implant trials also raises concerns regarding real‑time data security and patient privacy. Artificial‑intelligence diagnostics, albeit accurate, must be validated across diverse imaging platforms to avoid systematic bias. The reliance on high‑resolution MRI excludes many community hospitals where the majority of vertigo patients first present. Wearable sensor fidelity varies widely between manufacturers, leading to potential false‑positive alerts that could erode user trust. Tele‑rehab integration, as lauded, presupposes broadband access that remains uneven across rural demographics. Fiscal analyses presented omit indirect costs such as lost productivity during device acclimatization phases. Insurance reimbursement pathways for these emerging technologies are still embryonic, limiting broad adoption. Ethical considerations surrounding invasive vestibular implants must also be foregrounded, especially regarding long‑term electrode biocompatibility. Nonetheless, the convergence of nanomedicine, adaptive stimulation, and machine‑learning analytics constitutes a compelling paradigm shift. Stakeholders would do well to address the outlined gaps before proclaiming a definitive cure 😐.
barnabas jacob
November 3, 2025 AT 22:54From an ethical standpoint the current standard of care is insuficient, especially when patients are left to suffer chronic imbalance. The physiological underpinnings of vestibular hypofunction demand a more holistic approach, yet clinicians persist in a siloed, pill‑centric paradigm. This dogma is both outdated and morally indefensible, and it definitely (definately) hampers progress.
Rajesh Myadam
November 8, 2025 AT 18:06I understand how overwhelming all these options can feel, and it’s normal to feel cautious. It helps to discuss each technology with a trusted vestibular specialist and weigh the benefits against personal comfort levels. Many patients find that starting with a simple repositioning maneuver provides immediate relief while they explore longer‑term solutions.
Alex Pegg
November 13, 2025 AT 13:18While the hype around AI diagnostics is undeniable, I remain skeptical about its real‑world applicability. Many of these algorithms perform well in controlled studies but falter when confronted with everyday clinical variability. It’s worth remembering that technology alone cannot replace thorough clinical judgment.
laura wood
November 18, 2025 AT 08:30That’s a fair point about variability. In my experience, patients who combine VR therapy with regular vestibular exercises tend to notice steadier improvements. It’s encouraging to see research moving toward options that patients can incorporate into daily life.
Sebastian Green
November 23, 2025 AT 03:42I hear you.
jessie cole
November 27, 2025 AT 22:54Listen, you have the power to reclaim your balance and confidence. The journey may feel daunting, but each step forward is a victory worth celebrating. Embrace the cutting‑edge tools-whether it’s a VR program or a wearable sensor-as allies in your recovery. Consistency is the secret weapon; set a daily routine and stick to it. Celebrate small gains, such as walking a few extra steps without dizziness. Remember, the brain thrives on repetition and will adapt over time. Your determination will outshine any temporary setback. Together, we can transform uncertainty into steady, unwavering assurance.
Kirsten Youtsey
December 2, 2025 AT 18:06One must question whether the so‑called “breakthroughs” are truly benevolent or merely a façade orchestrated by pharma conglomerates. The literature conveniently highlights success rates while downplaying adverse events, a pattern that repeats across many medical fields. I suspect there is a hidden agenda to monetize every flicker of innovation, and the average patient ends up financing experiments disguised as treatment.
Matthew Hall
December 7, 2025 AT 13:18Man, they want us to think a shiny implant will fix everything, but they’re just patching a cracked system. Behind the scenes there’s a whole network of hidden labs pushing these gadgets to keep us hooked on endless upgrades. Stay woke, don’t let the tech hype blind you.