Creatine and Kidney Disease Medications: How to Monitor Renal Function Safely
 Dec, 3 2025
Dec, 3 2025
Creatine Adjustment Calculator
Adjust your estimated glomerular filtration rate (eGFR) for creatine supplementation to avoid misdiagnosis of kidney function.
How This Works
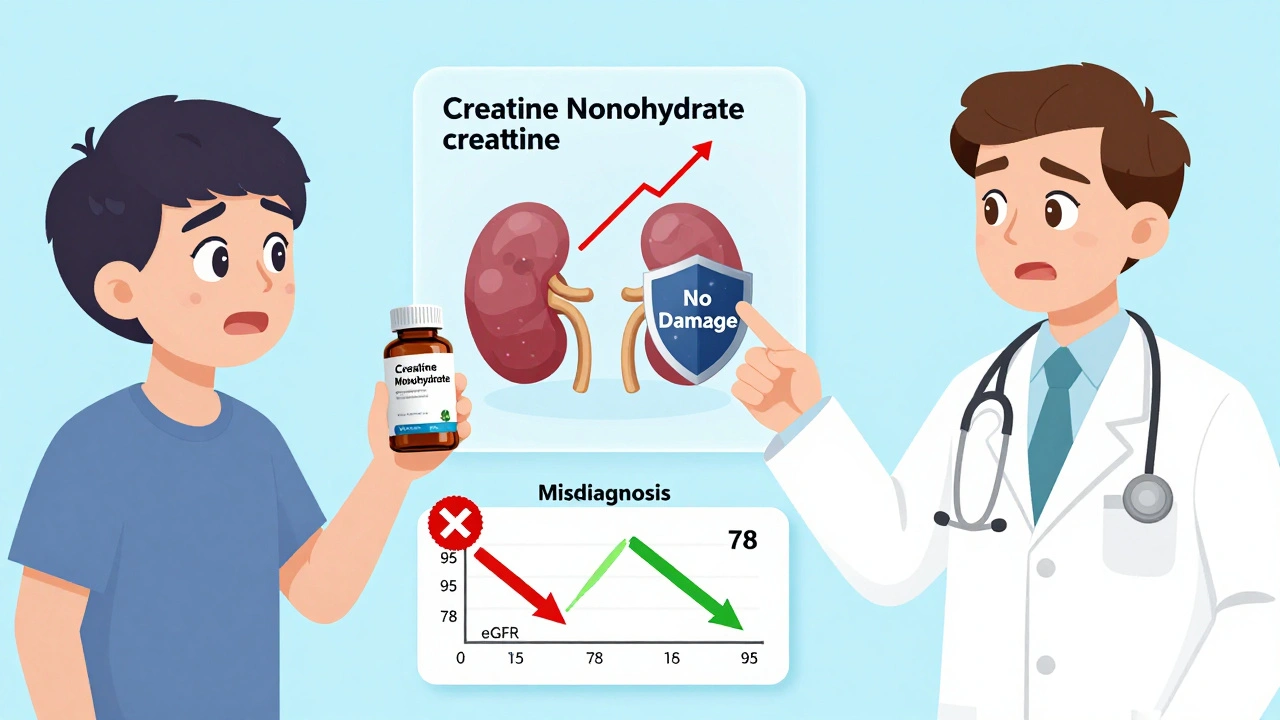
Creatine supplementation can raise serum creatinine levels by 10-30%, leading to falsely low eGFR values. This calculator adjusts your eGFR based on evidence that multiplying your standard eGFR by 0.9 gives a more accurate assessment for creatine users.
Important: This adjustment factor comes from University of Toronto research (2024) and is not yet standard clinical practice. Always discuss results with your doctor.
Your Estimated Kidney Function
This represents your estimated glomerular filtration rate (eGFR), a measure of kidney function.
What this means:
Based on your inputs and creatine adjustment factor of 0.9, your adjusted eGFR shows kidney function that is not impaired. This is especially important as creatine can falsely lower your eGFR by 10-30%.
Always discuss your kidney function results with your doctor, especially if you're taking kidney medications like ACE inhibitors or ARBs.
Many people take creatine to build muscle, boost strength, or recover faster from workouts. But if you’re on kidney disease medications - or have any kind of kidney issue - you need to know one critical thing: creatine doesn’t hurt your kidneys, but it can make your blood tests look like they do.
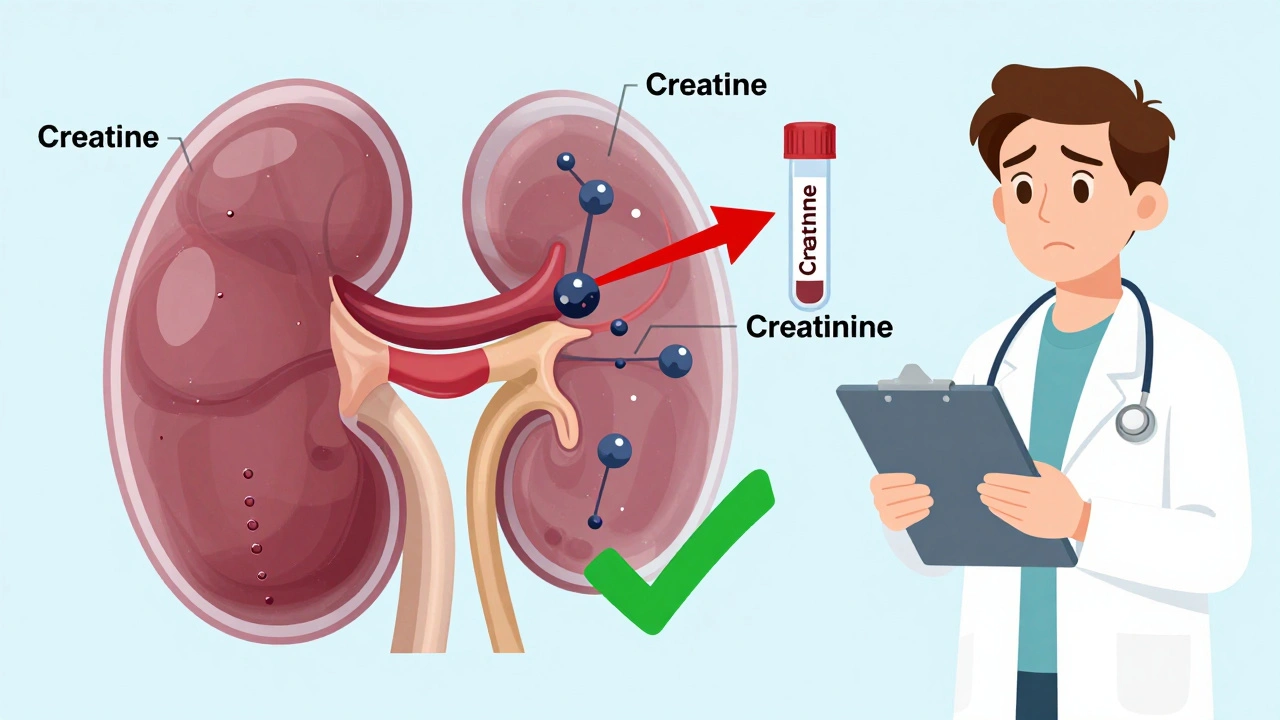
Here’s the problem: creatine breaks down into creatinine, a waste product your kidneys filter out. Doctors use creatinine levels to calculate your eGFR - a number that tells them how well your kidneys are working. When you take creatine, your creatinine levels rise. Not because your kidneys are failing - but because you’re flooding your body with more creatine to break down. That spike can trick doctors into thinking you have chronic kidney disease when you don’t.
Studies show creatine can raise serum creatinine by 10% to 30% without touching actual kidney function. One 2000 study tracked 48 healthy adults taking 5 grams of creatine daily for weeks. Their creatinine went up - but their kidneys kept working just fine. Blood urea nitrogen (BUN), urine output, and electrolytes stayed normal. The same pattern shows up in older adults, athletes, and sedentary people alike. The rise is real. The damage isn’t.
But here’s where it gets dangerous. If you’re already on meds for kidney disease - like ACE inhibitors, ARBs, or diuretics - and your doctor sees a rising creatinine, they might assume your condition is worsening. They could change your meds, order unnecessary scans, or even refer you to a specialist. Meanwhile, you’re perfectly fine. This isn’t hypothetical. On Reddit, users have shared stories of being misdiagnosed with stage 2 chronic kidney disease after starting creatine. Their eGFR dropped from 95 to 78. After stopping creatine, it bounced back to 95. No treatment needed. Just a misunderstood lab result.
Primary care doctors are often unaware of this. A 2021 survey found 67% of them didn’t know creatine affects creatinine levels. They see a high number, they worry. They don’t ask if you’re taking supplements. And most people don’t think to mention creatine unless they’re asked. It’s not a drug. It’s a powder in a shaker bottle. But it’s powerful enough to mess with medical decisions.
What Happens When Creatine Meets Kidney Medications?
If you have kidney disease and take medications like lisinopril, losartan, furosemide, or spironolactone, your kidneys are already under stress. These drugs help control blood pressure and reduce protein leakage - important for slowing kidney damage. But they can also affect how creatinine is cleared.
There’s no evidence that creatine makes these medications more toxic. But combining them with creatine creates a perfect storm for misinterpretation. Your creatinine goes up. Your doctor sees it and wonders: Is this the medicine? Is it the creatine? Is your disease getting worse? The answer is usually none of the above - but without the right context, you’ll get treated as if it is.
One case report from 2011 described a healthy man who developed acute tubular necrosis after taking 3 grams of creatine daily. He had no prior kidney issues. No other drugs. No dehydration. But that’s the exception - not the rule. Over 500 studies have looked at creatine and kidney health. Only one showed a possible link - and even that case had no clear cause. The rest? Nothing. Not even a hint of harm.
What’s worse? Some supplement brands now sell “kidney-safe creatine.” They claim it’s different. But ConsumerLab.com tested these products in 2024. There’s no difference in how they affect creatinine. They’re all creatine monohydrate. The label doesn’t change the science.
How to Monitor Your Kidneys Correctly
If you’re taking creatine - and especially if you’re on kidney meds - you need a smarter way to check your kidney function. Relying on serum creatinine alone is like judging a car’s engine by how loud it sounds. The noise might be normal. Or it might mean something’s broken. You need better tools.
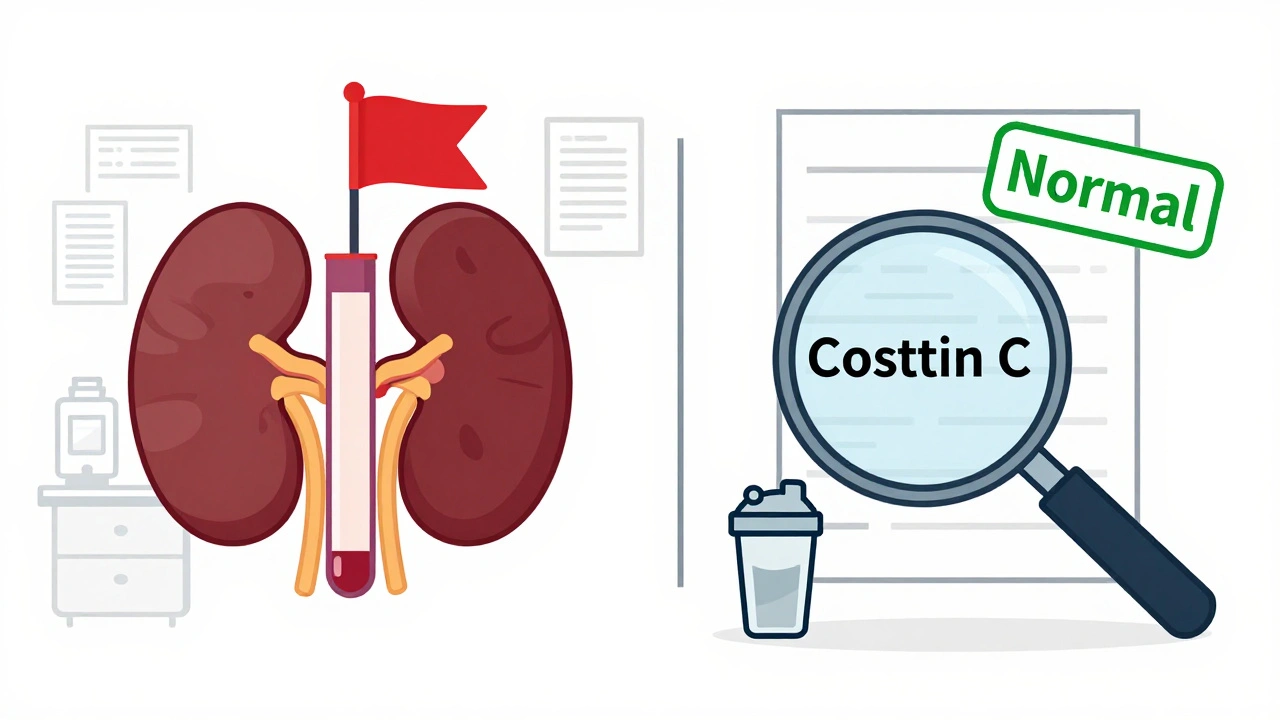
The best solution is cystatin C. This protein is filtered by the kidneys too, but it’s not affected by creatine. When you combine cystatin C with creatinine in an eGFR equation (called CKD-EPI CysC), you get a much clearer picture. A 2020 study found cystatin C-based eGFR matches actual kidney function with 95% accuracy - even in people taking creatine.
But not every lab offers cystatin C. If yours doesn’t, ask for a 24-hour urine creatinine clearance test. This measures exactly how much creatinine your kidneys are removing over a full day. Unlike blood tests, this number doesn’t go up just because you’re supplementing. It stays stable - even if your blood creatinine spikes.
Here’s what to do:
- Get a baseline creatinine and cystatin C test before starting creatine.
- Start with 3-5 grams per day. Skip the 20-gram loading phase unless you’re an elite athlete.
- After 4-6 weeks, repeat the tests. If creatinine rose but cystatin C didn’t, you’re fine.
- Keep taking your kidney meds as prescribed. Don’t stop them because your creatinine went up.
- Always tell your doctor you’re taking creatine - even if they don’t ask.
Most people who take creatine safely never have an issue. A 2022 survey of 157 users found 89% had no kidney-related problems. Only 11% saw a temporary creatinine rise - and it dropped back to normal after they stopped.
What the Experts Say
The National Kidney Foundation says creatine is safe for healthy people. UCLA Health agrees. The American College of Sports Medicine recommends testing kidney function before starting - but only because of the risk of misdiagnosis, not because creatine causes harm.
Nephrologists in Chile and the U.S. all say the same thing: creatine doesn’t cause kidney disease. But they also warn: don’t take it if you already have kidney disease. Why? Because even though creatine isn’t the problem, your kidneys might not handle the extra load - and you’re already on meds that can interact with other substances.
There’s one more thing: a 2024 Mendelian randomization study used genetic data to prove creatine doesn’t cause kidney damage. It looked at thousands of people and found zero link between creatine levels and kidney function. The authors concluded: “Concerns about creatine triggering kidney issues may not be justified.”
What You Should Do Right Now
If you’re on kidney meds and thinking about taking creatine - don’t. Wait. Talk to your nephrologist first. They know your history. They can tell you if your kidneys can handle the extra creatinine load - even if it’s not harmful.
If you’re already taking creatine and have kidney disease - stop. Don’t panic. But get your kidney function checked with cystatin C or a 24-hour urine test. Don’t rely on your regular blood work. It’s lying to you.
If you’re healthy and taking creatine - tell your doctor. Write it down on your medication list. Bring it up at every checkup. If your creatinine jumps and your doctor starts asking questions, say: “I’m taking creatine. Can we check cystatin C?” Most won’t know what to do. But now you do.
Supplements aren’t harmless just because they’re natural. Creatine is one of the most studied supplements on earth. It’s safe. But it’s not invisible to your lab results. And in the world of kidney disease, a single wrong number can change your treatment - and your life.
What About Long-Term Use?
People have taken creatine for 20+ years. Long-term studies show no decline in kidney function - even in athletes who use it daily for over a decade. The European Food Safety Authority says 3 grams per day is safe for life. The FDA doesn’t regulate it, but that doesn’t mean it’s risky. It just means you need to be smarter about how you use it.
Some researchers are now working on formulas that adjust eGFR automatically for creatine users. Early data from the University of Toronto suggests multiplying your creatinine-based eGFR by 0.9 gives you the right number. That’s not standard yet - but it’s coming.
For now, the rule is simple: creatine doesn’t break your kidneys. But it can break your diagnosis.
Does creatine damage the kidneys?
No, creatine does not damage the kidneys in healthy people. Over 500 studies show no harmful effects on kidney function. The rise in creatinine levels is a metabolic side effect, not a sign of damage. However, people with existing kidney disease should avoid creatine because their kidneys may not handle the extra workload, especially when combined with nephrotoxic medications.
Why does creatine raise creatinine levels?
Creatine naturally breaks down into creatinine at a rate of about 1.7% per day. When you supplement with creatine, your body has more of it to convert. This increases the amount of creatinine in your blood, which is what labs measure. It’s like pouring more water into a river - the flow increases, but the riverbed isn’t eroded.
Can I still take creatine if I have kidney disease?
No. If you have chronic kidney disease (CKD), you should avoid creatine. Even though creatine isn’t toxic, your kidneys are already struggling to filter waste. Adding extra creatinine could make it harder for them to keep up - especially when combined with medications like ACE inhibitors or diuretics. Always check with your nephrologist before taking any supplement.
What test should I ask for instead of serum creatinine?
Ask for cystatin C or a 24-hour urine creatinine clearance. Cystatin C is not affected by creatine supplementation and gives a more accurate picture of kidney function. If cystatin C isn’t available, a 24-hour urine test measures actual creatinine excretion and isn’t skewed by supplement use.
Should I stop creatine before a kidney blood test?
If you’re being tested for kidney function and you take creatine, it’s best to stop for at least 2 weeks before the test. This lets your creatinine levels return to baseline. But if you’re on kidney disease meds, don’t stop creatine without talking to your doctor. They may prefer to use cystatin C instead of asking you to quit.
Do ‘kidney-safe’ creatine products work?
No. Products labeled as ‘kidney-safe’ or ‘low-creatinine’ are marketing gimmicks. All creatine supplements - even those with fancy names - break down into creatinine the same way. ConsumerLab.com tested these products in 2024 and found no difference in their effect on creatinine levels. Stick with plain creatine monohydrate and focus on proper testing instead.
How common is misdiagnosis from creatine use?
It’s more common than you think. A 2023 survey found only 42% of primary care doctors routinely ask patients if they take creatine when they see high creatinine. Many patients don’t mention it because they don’t think it matters. This leads to unnecessary referrals, anxiety, and even incorrect treatment. Awareness is growing, but it’s still not standard practice.
What Comes Next?
The next big update from the National Kidney Foundation is expected in late 2024. It will likely include formal guidelines for managing creatine users - something most nephrologists still don’t have. Until then, you’re your own best advocate.
Know your numbers. Know your supplements. Ask the right questions. Creatine is safe. But your kidneys deserve more than a guess. They deserve the truth - even if the truth is hiding in plain sight on a lab report.
Martyn Stuart
December 4, 2025 AT 07:25Just wanted to say this is one of the clearest, most important posts I’ve read all year. So many people are getting misdiagnosed because doctors don’t ask about supplements-creatinine isn’t a disease marker, it’s a metabolic byproduct. If you’re on kidney meds and taking creatine, you’re not being reckless-you’re just uninformed. And that’s on the system, not you.
Shofner Lehto
December 6, 2025 AT 06:58This is why I stopped trusting routine blood panels. I’ve been on losartan for 5 years and started creatine last year. My creatinine jumped from 1.0 to 1.3. My nephrologist asked if I was supplementing before even looking at the numbers. That’s the kind of doctor you want.
Yasmine Hajar
December 7, 2025 AT 20:47Okay but can we talk about how wild it is that a powder in a shaker bottle can derail someone’s entire medical trajectory? I had a friend get referred to a specialist because her eGFR dropped to 72. She cried for a week. Turned out she’d been taking creatine for 3 months. Stopped it. Two weeks later-back to 90. No meds changed. No scans needed. Just a lab result that lied.
Jake Deeds
December 8, 2025 AT 01:17It’s fascinating how the medical establishment still treats supplements like they’re voodoo. Creatine is one of the most rigorously studied compounds in sports science-over 500 studies, zero evidence of renal harm. Yet we’re still letting untrained PCPs panic over a number that’s been proven to be a red herring. The fact that ‘kidney-safe creatine’ is even a thing speaks volumes about how profit-driven healthcare has become.
Chase Brittingham
December 8, 2025 AT 23:06My dad’s on dialysis. He asked me if he could take creatine to feel stronger. I told him no-not because it’s dangerous, but because his kidneys can’t handle the extra load. Even if it’s not toxic, it’s still more work for a system that’s already overwhelmed. This post nails it: it’s not about creatine being bad. It’s about knowing your body’s limits.
Bill Wolfe
December 10, 2025 AT 01:52People still don’t get it. Creatine isn’t ‘natural’-it’s a synthetic compound that alters biochemistry. Just because it’s not ‘toxic’ doesn’t mean it’s benign. The fact that you’re casually suggesting people keep taking it while on ACE inhibitors is dangerously irresponsible. What if your kidneys are borderline? What if you’re pre-diabetic? You’re not just messing with labs-you’re playing Russian roulette with your renal function.
michael booth
December 10, 2025 AT 03:04Thank you for this. As a primary care provider, I was unaware of the creatinine artifact until last month. I’ve since added a supplement checklist to my intake forms. We’re not trained for this. But we’re learning. And we need more posts like this to bridge the gap.
Carolyn Ford
December 11, 2025 AT 14:51So… you’re telling me that people who take creatine are just… lazy? They don’t want to wait for results, so they pop a powder and then get scared when the numbers go up? And now we’re supposed to trust cystatin C? Who even tests for that? And why is it so expensive? This feels like a rich person’s solution to a problem created by people who think supplements are vitamins.
Rudy Van den Boogaert
December 12, 2025 AT 03:08My sister’s a nephrologist. She told me last week that 3 out of the last 5 patients she saw with ‘newly diagnosed’ CKD were creatine users. All of them were healthy otherwise. One was a 68-year-old grandma who thought creatine was just ‘protein powder for muscles.’ She was terrified. They did cystatin C-her eGFR was 94. She cried again, but this time from relief.
Gillian Watson
December 12, 2025 AT 18:48Just started creatine last month. I’m 42, no kidney issues, but I’m on a low-dose diuretic for blood pressure. I’m gonna wait 6 weeks and ask for cystatin C. If my doc doesn’t know what it is, I’ll print this post and hand it to them. No drama. Just facts.
Karl Barrett
December 12, 2025 AT 23:12The epistemological rupture here is profound. We’ve constructed a diagnostic framework predicated on creatinine as a biomarker of glomerular filtration, yet we’ve failed to account for the exogenous modulation of that biomarker’s baseline. The clinical inference chain is thus compromised-false positives proliferate because the model lacks a correction factor for supplement-induced creatinine elevation. We need algorithmic recalibration, not just patient education.
Elizabeth Crutchfield
December 13, 2025 AT 03:36i just started creatine and my dr said my creatinine is high but i didnt even know what that meant… now im scared. should i stop??
Augusta Barlow
December 14, 2025 AT 19:27Look, I’ve been following this stuff for years. The truth is, creatine isn’t the problem. The problem is that the pharmaceutical industry doesn’t profit from a supplement that doesn’t cause disease. That’s why they let doctors stay ignorant. That’s why labs don’t offer cystatin C unless you beg for it. That’s why ‘kidney-safe creatine’ exists-it’s a scam to make you feel better while they keep selling you the same product under a new label. Wake up. They don’t want you to know the truth.
Jenny Rogers
December 16, 2025 AT 05:44It is not merely irresponsible to suggest that creatine is safe for individuals with compromised renal function. The very premise of this article ignores the fundamental principle of nephrology: the kidney is a homeostatic organ, and any exogenous metabolic burden-no matter how benign in isolation-must be evaluated in the context of systemic fragility. To equate ‘no histological damage’ with ‘no clinical risk’ is a fallacy of the highest order.
val kendra
December 17, 2025 AT 08:07Been taking creatine for 8 years. On lisinopril for hypertension. Got cystatin C done last year-perfectly normal. Told my doctor I take it. He nodded and said, ‘Good, we’ll monitor it.’ No panic. No confusion. Just a smart doc who knows his stuff. This post is gold. Share it with your doctor. They might not know-but you do now.