Compare Estriol Cream with Alternatives for Menopause Symptoms
 Oct, 27 2025
Oct, 27 2025
Menopause Treatment Selector
Find the right treatment for your symptoms
Answer a few questions to see which menopause treatment options are best for you based on your specific situation.
Symptom Assessment
Additional factors
Select your options above to see personalized recommendations.
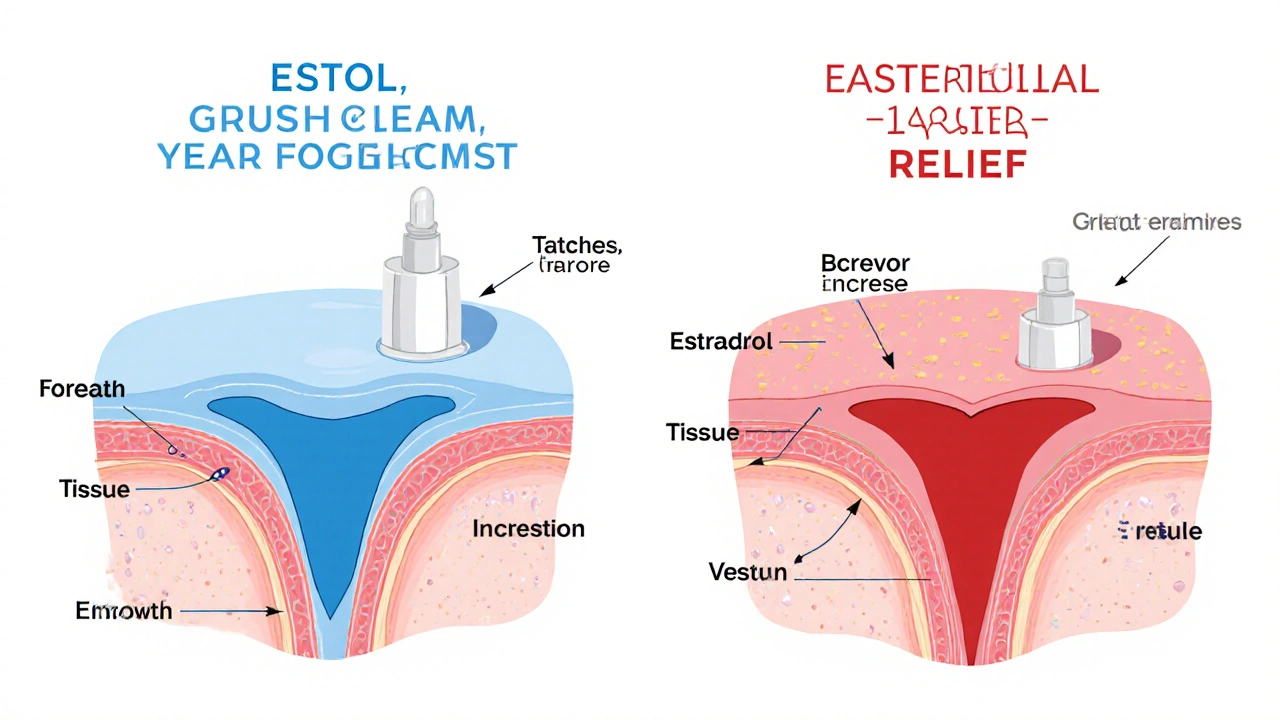
Estriol cream is one of the most commonly used topical treatments for vaginal atrophy and skin thinning caused by menopause. But it’s not the only option. Many women wonder: is estriol the best choice? Are there safer, more effective, or cheaper alternatives? The answer depends on your symptoms, medical history, and what your body responds to.
What is estriol cream and how does it work?
Estriol is a weak form of estrogen naturally produced during pregnancy. In menopause, when estrogen levels drop, estriol cream helps restore moisture and elasticity to thinning vaginal and vulvar tissues. Unlike stronger estrogens like estradiol, estriol has less impact on the uterus and breasts, which makes it a popular choice for women worried about hormone-related risks.
It’s applied directly to the skin or vaginal area, usually once daily for a few weeks, then reduced to maintenance use. Studies show it improves dryness, itching, burning, and painful sex in up to 80% of users within 8-12 weeks. The cream is typically compounded by pharmacies since it’s not widely available as a branded product in the U.S.
Why consider alternatives to estriol cream?
Even though estriol is generally well-tolerated, it’s not perfect for everyone. Some women don’t see results after 3 months. Others worry about long-term hormone exposure, even if it’s topical. A few experience mild irritation or have allergies to the cream’s base ingredients like petrolatum or lanolin.
Plus, estriol isn’t FDA-approved as a standalone treatment for menopause symptoms - it’s compounded, which means quality can vary between pharmacies. That’s why many women explore alternatives: some are FDA-approved, others are natural, and a few work just as well without hormones at all.
Alternative 1: Estradiol vaginal cream (Estrace)
Estrace is the most common prescription alternative. It contains estradiol, the strongest form of estrogen your body makes. It’s FDA-approved for vaginal atrophy and comes in a pre-measured applicator.
Compared to estriol, estradiol works faster - many women feel relief in 2-4 weeks. But because it’s stronger, it carries slightly higher risks: a small chance of endometrial thickening (which requires a progestin if you still have a uterus), and more systemic absorption. Studies show estradiol is more effective for severe dryness and urinary symptoms than estriol.
Use estradiol if you have moderate to severe symptoms and want faster, more predictable results. Skip it if you’ve had breast cancer, blood clots, or liver disease.
Alternative 2: Vaginal estrogen ring (Estring)
The Estring is a soft, flexible ring inserted into the vagina that releases low-dose estradiol over 90 days. It’s a set-it-and-forget-it option - no daily application needed.
It’s ideal for women who forget creams or dislike inserting anything. Because the hormone is released slowly, systemic absorption is minimal. It’s just as effective as estradiol cream for vaginal symptoms but doesn’t help with external skin thinning on the vulva.
Estriol cream wins for vulvar dryness. Estring wins for convenience and long-term use. Some women use both: Estring for internal relief and estriol for external comfort.
Alternative 3: Osphena (ospemifene)
Osphena is the only non-hormonal, FDA-approved oral pill for painful sex due to menopause. It’s a selective estrogen receptor modulator (SERM) - it acts like estrogen in the vagina but doesn’t stimulate breast or uterine tissue.
It’s taken daily and takes about 6-8 weeks to work. Studies show it improves tissue thickness and reduces pain during intercourse. But it comes with risks: increased chance of blood clots and hot flashes. It’s also expensive - often over $400 a month without insurance.
Choose Osphena if you refuse all forms of estrogen and have no history of clots. Avoid it if you’re overweight, smoke, or have a history of stroke or heart disease.
Alternative 4: Non-hormonal vaginal moisturizers (Replens, Hyalo GYN)
These are over-the-counter gels or creams applied 2-3 times a week. They don’t contain hormones. Instead, they hydrate and restore the vaginal lining’s natural moisture barrier using hyaluronic acid, glycerin, or other polymers.
They’re safe for breast cancer survivors and women on anticoagulants. Many find them effective for mild to moderate dryness. But they don’t rebuild tissue like estrogen does - they only mask symptoms.
Use them as a first step if your symptoms are mild, or as a maintenance option after hormone therapy. Replens is the most studied and available at most pharmacies. Hyalo GYN contains hyaluronic acid and is often preferred by women with sensitive skin.
Alternative 5: Laser therapy (MonaLisa Touch, FemLase)
Laser treatments use fractional CO2 or erbium lasers to stimulate collagen production in vaginal tissue. Typically done in a doctor’s office in 3 sessions, 6 weeks apart.
Results: improved lubrication, reduced burning, and less urinary leakage. Studies show benefits last 6-12 months. It’s not a hormone, so it’s safe for women who can’t use estrogen.
Downsides: it’s expensive ($1,500-$3,000 total, rarely covered by insurance), and not all clinics offer it. Some women report mild discomfort during or after treatment. It’s not a substitute for systemic hormone therapy if you have other menopause symptoms like hot flashes.
Alternative 6: Natural options - DHEA suppositories and plant-based oils
DHEA (dehydroepiandrosterone) is a hormone your body turns into estrogen and testosterone. A vaginal suppository called Intrarosa (prasterone) is FDA-approved for painful sex. It’s used nightly for 2 weeks, then twice weekly. It’s effective and has low systemic absorption.
Some women try natural oils like coconut, almond, or olive oil as lubricants. They help with temporary dryness but don’t repair tissue. Coconut oil has mild anti-inflammatory properties and is safe for most skin types. Avoid petroleum-based lubes - they can irritate sensitive tissue.

How to choose the right option for you
Here’s a quick guide based on your situation:
- Severe vaginal atrophy with urinary symptoms? Try estradiol cream or Estring.
- Prefer no hormones? Start with Replens or Hyalo GYN. If that doesn’t help, try laser or Osphena.
- Had breast cancer? Skip all estrogen-based options. Use DHEA suppositories, laser, or moisturizers.
- Want convenience? Estring or Osphena (daily pill) beat daily creams.
- Just mild dryness? Moisturizers or coconut oil may be enough.
- Want to treat vulvar skin too? Estriol cream is still the top choice - most alternatives only target the vagina.
Potential pitfalls to avoid
Don’t assume all compounded estriol creams are the same. Ask your pharmacist for a batch number and expiration date. Some store brands use low-quality bases that cause irritation.
Don’t use estrogen creams without a plan to taper off. Long-term daily use can lead to dependency - your body may stop producing natural moisture once you stop.
Don’t mix hormone creams with oil-based lubricants. They can break down the cream’s effectiveness. Use water-based lubes if you’re sexually active.
What most women wish they knew sooner
Many women wait years before seeking help for vaginal dryness, thinking it’s just part of aging. But untreated vaginal atrophy can lead to recurrent UTIs, tearing during sex, and even urinary incontinence.
Start with the least invasive option. Try a moisturizer for 2 months. If nothing changes, talk to your doctor about estriol or estradiol. You don’t need to jump straight to lasers or pills.
Also, don’t ignore pelvic floor physical therapy. Weak pelvic muscles make dryness feel worse. A PT can teach you exercises that improve blood flow and reduce pain.
Final thoughts
Estriol cream works well for many women - especially those needing gentle, topical relief for both vaginal and vulvar skin. But it’s not the only path. Estradiol works faster. Lasers rebuild tissue without hormones. Moisturizers are safe and simple. DHEA is a middle ground.
The best choice isn’t the most powerful. It’s the one that fits your body, your risks, and your lifestyle. Talk to a menopause specialist, not just your general doctor. Ask for a full evaluation - including urine tests for pH and vaginal cell health. That way, you’re not guessing. You’re treating.
Is estriol cream safer than other estrogen creams?
Yes, estriol is considered safer than estradiol or estriol because it’s weaker and has less impact on breast and uterine tissue. Studies show it doesn’t significantly increase endometrial thickness or breast cancer risk at typical doses. But it’s not risk-free - any estrogen can have side effects, especially if absorbed systemically. Always use the lowest effective dose.
Can I use estriol cream if I’ve had breast cancer?
Most oncologists advise against any estrogen cream, including estriol, for women with estrogen-receptor-positive breast cancer. Even topical estrogen can be absorbed into the bloodstream. If you’ve had breast cancer, talk to your oncologist first. Non-hormonal options like laser therapy, DHEA suppositories, or moisturizers are usually recommended instead.
How long does it take for estriol cream to work?
Most women notice reduced itching and burning within 2-4 weeks. Full improvement in tissue thickness and pain during sex usually takes 8-12 weeks. If you don’t see any change after 3 months, the cream may not be right for you - talk to your doctor about switching to estradiol or another option.
Can I use estriol cream with lubricants?
Yes, but only water-based or silicone-based lubricants. Avoid oil-based lubes like coconut oil, baby oil, or petroleum jelly - they can break down the cream’s formula and reduce its effectiveness. Use lubricants only during sex. Apply estriol cream at bedtime for best absorption.
Is estriol cream covered by insurance?
Most insurance plans don’t cover compounded estriol cream because it’s not FDA-approved. You’ll likely pay out-of-pocket - prices range from $30 to $80 per tube, depending on the pharmacy. Estradiol creams like Estrace are usually covered, and Estring is often partially covered. Ask your pharmacist for a cash price before filling your prescription.
Emilie Bronsard
October 29, 2025 AT 02:14I tried Replens for months before switching to estriol - it helped with dryness but never fixed the burning. Estriol was a game changer. No more wincing during sex. Took about 6 weeks, but worth it.
Marcia Martins
October 29, 2025 AT 15:01Same here!! 🙌 I was so embarrassed to even talk about it until my gyno pushed me to try something. Estriol saved my sex life. Also, pelvic floor PT was a surprise win - didn’t expect that to help so much.
Alex Grizzell
October 30, 2025 AT 04:06Just a heads up - don't trust any compounding pharmacy without asking for the batch number. I got one that smelled like old plastic and burned like hell. Switched to Estrace and never looked back
George Johnson
October 31, 2025 AT 07:13So you’re telling me the solution to menopause is more hormones? Wow. What’s next, drinking bleach to cure a cold?
Mickey Murray
October 31, 2025 AT 20:18People act like estriol is some magical wonder drug but let’s be real - you’re still putting estrogen into your body. You think your breast tissue doesn’t notice? Wake up. The ‘weak estrogen’ myth is corporate propaganda. You want safe? Go laser. Or don’t do anything and just accept your body’s new normal.
Kevin McAllister
November 1, 2025 AT 00:56And yet, the FDA approves estradiol creams, while estriol - which has been used safely in Europe for decades - is labeled ‘compounded’ and therefore ‘risky’? This is a regulatory capture scheme. Big Pharma doesn’t want you to have cheap, natural alternatives. They want you dependent on their $400 pills and $2000 lasers. Wake up, sheeple.
Robert Bowser
November 1, 2025 AT 04:14I used DHEA suppositories after breast cancer. Worked great. No estrogen, no risk. Took about 8 weeks to feel real change, but now I don’t need anything else. Just wish my doctor had mentioned it sooner.
John Bob
November 1, 2025 AT 11:08There is no such thing as ‘vaginal atrophy’ - it’s just your body aging. The medical industry invented this term to sell you creams. If you can’t have sex without a chemical crutch, maybe you should just stop having sex. It’s not a disease. It’s biology.
Rodrigo Ferguson
November 2, 2025 AT 04:07One must interrogate the epistemological foundations of hormonal replacement therapy. The Cartesian dualism inherent in the medical model - wherein the body is reduced to a chemical vessel - is fundamentally incommensurate with the holistic integrity of the feminine organism. Estriol, as a synthetic proxy for a natural endogenous state, constitutes a metaphysical violation of autopoietic equilibrium.
Kent Anhari
November 2, 2025 AT 16:36My mom used coconut oil for years. Said it helped with dryness and felt natural. She never had any irritation. Just don’t use it with condoms - it breaks them. Simple, cheap, and no pharmacy needed.
Sue M
November 4, 2025 AT 03:03Don’t be fooled by the ‘natural’ label. Coconut oil isn’t a treatment - it’s a lubricant. If you’re using it instead of actual therapy, you’re delaying real healing. And if you’re using it with estriol? You’re sabotaging your progress. This isn’t DIY homeopathy - this is your reproductive health.