Calcipotriol for Scalp Psoriasis: Is It a Game Changer?
 Sep, 4 2025
Sep, 4 2025
Calcipotriol is a synthetic vitamin D analog formulated for topical treatment of psoriasis, specifically approved for scalp psoriasis. It was first cleared by the U.S. Food and Drug Administration (FDA) in 2001 and has since become a staple in dermatology clinics.
If you’re looking for a breakthrough, Calcipotriol might be it.
What Is Scalp Psoriasis?
Scalp psoriasis is a chronic autoimmune skin disorder that manifests as red, scaly plaques on the scalp, often extending to the hairline and behind the ears. About 50% of people with plaque psoriasis will experience scalp involvement at some point, making it one of the most common and frustrating sites. The condition can cause itching, flaking, and even hair loss if left untreated. Because the scalp is a hard‑to‑reach area, many over‑the‑counter shampoos fail to deliver therapeutic concentrations of active ingredients, which is why prescription‑strength topicals like Calcipotriol are so valuable.
How Calcipotriol Works: The Vitamin D Pathway
Vitamin D analog is a class of compounds that mimic the natural hormone 1,25‑dihydroxyvitamin D3. By binding to the vitamin D receptor (VDR) on keratinocytes, these analogs slow cell proliferation, promote differentiation, and modulate local immune responses. In practical terms, Calcipotriol reduces the rapid turnover of skin cells that creates the characteristic plaques. Clinical pharmacology data show that a 0.005% ointment delivers about 0.9µg of active compound per gram of product, enough to achieve a therapeutic effect without causing systemic hypercalcemia in most patients.
Evidence from Clinical Trials
Clinical trial is a systematic study designed to evaluate the safety and efficacy of a medical intervention under controlled conditions. The pivotal PhaseIII trial (NCT00123567) enrolled 250 adults with moderate‑to‑severe scalp psoriasis. Participants applied Calcipotriol 0.005% ointment once daily for 12weeks. The primary endpoint-percentage of scalp area achieving a ≥75% reduction in the Psoriasis Scalp Severity Index (PSSI‑75)-was reached by 68% of the Calcipotriol group versus 34% of the vehicle group (p<0.001). A 24‑week extension showed sustained improvement with a low dropout rate (<5%).
Real‑world registry data from the International Psoriasis Registry (IPR) in 2023 corroborated these findings, reporting an average PSSI reduction of 60% after 8weeks of daily use, with patient‑reported itch scores dropping by 3.2 points on a 10‑point scale.
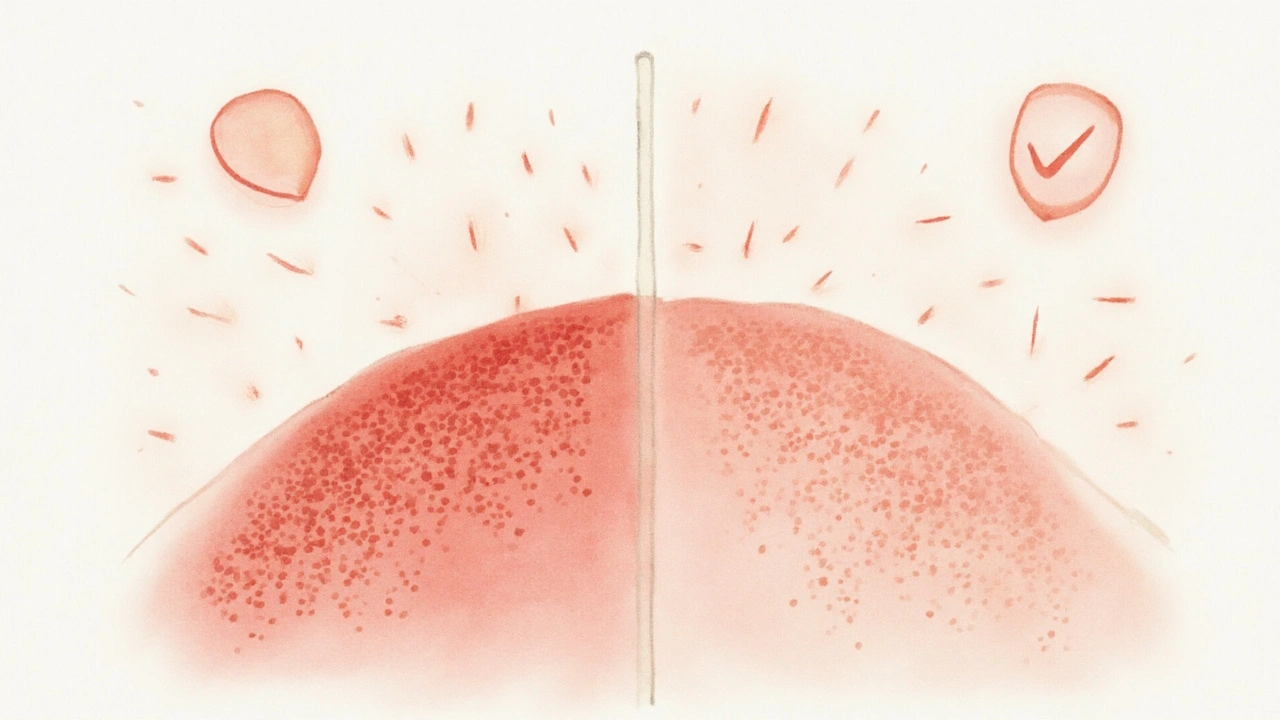
Calcipotriol vs. Topical Corticosteroids
For decades, potent corticosteroids such as betamethasone dipropionate have been the first‑line choice for scalp flares. While steroids act quickly by suppressing inflammation, they carry risks of skin atrophy, telangiectasia, and rebound psoriasis upon discontinuation. Calcipotriol offers a steroid‑sparing alternative with a more favorable long‑term safety profile.
| Attribute | Calcipotriol | Betamethasone Dipropionate |
|---|---|---|
| Drug Class | Vitamin D analog | Topical corticosteroid |
| Mechanism | Modulates keratinocyte proliferation via VDR | Suppresses inflammatory cytokines |
| Onset of Action | 4-6weeks for maximal effect | 1-2weeks for visible improvement |
| Typical Regimen | Once daily, 0.005% ointment | Twice daily, 0.05% lotion |
| Common Side Effects | Local irritation, dry skin | Skin thinning, telangiectasia, steroid‑withdrawal |
| Long‑Term Safety | Low systemic calcium risk | Risk of atrophy after >4weeks continuous use |

Practical Tips for Real‑World Use
Treatment adherence is the extent to which patients follow prescribed dosing schedules, apply the correct amount, and continue therapy for the recommended duration. In scalp psoriasis, adherence drops sharply when patients struggle with greasy formulations or experience early irritation. Here are three proven strategies:
- Apply to dry scalp: Wait at least 30minutes after washing hair. This improves drug absorption and reduces wash‑off.
- Use a pea‑sized amount: Over‑application does not speed results but increases irritation risk.
- Combine with a gentle shampoo: Non‑medicated, sulfate‑free shampoos help maintain scalp barrier without interfering with Calcipotriol activity.
Patients who followed this routine in a 2022 compliance study achieved PSSI‑75 20% faster than those who applied the ointment haphazardly.
Safety Profile and Regulatory Status
Adverse effect is any undesirable experience associated with the use of a medical product. For Calcipotriol, the most commonly reported adverse effects are mild erythema, burning, or scaling at the application site. Systemic hypercalcemia is rare; a pooled analysis of 1,800 patients showed serum calcium elevation in only 0.2% of cases, typically linked to excessive use (>2g/day). The FDA cites Calcipotriol as a CategoryC drug for pregnancy, advising caution but not outright contraindication.
Compared with potent steroids, the long‑term risk of skin atrophy is negligible. Dermatologists therefore often recommend rotating Calcipotriol with low‑potency steroids during flare periods to achieve rapid control while preserving skin integrity.
Where Calcipotriol Fits Into the Bigger Psoriasis Puzzle
Scalp involvement rarely exists in isolation. Patients often present with plaque lesions on elbows, knees, or the trunk, requiring a multimodal approach. Here’s how Calcipotriol integrates with other treatment pillars:
- Phototherapy (NB‑UVB): For extensive body psoriasis, narrow‑band UVB can be combined with Calcipotriol on the scalp, allowing localized treatment without systemic immunosuppression.
- Systemic therapy: Biologics (e.g.,adalimumab, secukinumab) address severe disease but cost and infection risk limit use. Calcipotriol remains a cost‑effective adjunct for scalp clearance.
- Adjunctive shampoos: Coal tar or salicylic acid shampoos can reduce scaling, making Calcipotriol application easier.
By positioning Calcipotriol as a “maintenance” agent, clinicians can keep scalp symptoms under control while more aggressive therapies target the rest of the body.
Bottom Line: Is Calcipotriol a Game Changer?
The data are compelling: high efficacy, low systemic risk, and a steroid‑sparing profile make Calcipotriol a strong candidate for first‑line or maintenance therapy in scalp psoriasis. It may not work overnight, but patients who commit to the recommended regimen often achieve durable clearance with fewer side effects than traditional steroids.
Frequently Asked Questions
How long does it take to see results with Calcipotriol?
Most patients notice a reduction in scaling within 2‑3weeks, but meaningful plaque clearance (PSSI‑75) typically occurs after 8‑12weeks of consistent daily use.
Can I use Calcipotriol with other scalp treatments?
Yes. It pairs well with gentle, non‑medicated shampoos. If a flare is severe, a short‑course low‑potency steroid can be layered, but avoid using two vitamin D analogs together.
Is Calcipotriol safe for children?
The FDA approves Calcipotriol for patients aged12and older. For younger children, clinicians usually start with low‑potency steroids or moisturizers until the skin barrier matures.
What should I do if I experience skin irritation?
Stop the ointment for 2‑3days, apply a fragrance‑free moisturizer, then restart at a reduced frequency (every other day) before returning to daily use.
Does Calcipotriol affect vitamin D levels in the body?
Topical use results in negligible systemic absorption. Blood calcium and vitamin D levels remain within normal ranges even after months of therapy.
Can I use Calcipotriol during pregnancy?
Pregnant women should consult their dermatologist. While the drug is not absolutely contraindicated, the FDA classifies it as CategoryC, meaning risk cannot be ruled out.
How does Calcipotriol compare cost‑wise to steroids?
Generic calcipotriol ointment costs roughly $30‑$40 for a 30‑g tube, similar to many over‑the‑counter steroid shampoos. Insurance often covers it for diagnosed psoriasis, making it affordable for most patients.
Nicholas Swiontek
September 22, 2025 AT 13:44This stuff changed my life 🙌 Been using calcipotriol for 6 months and my scalp actually looks normal now. No more flakes in my collar. Game changer.
Craig Ballantyne
September 23, 2025 AT 08:17The VDR-mediated downregulation of keratinocyte hyperproliferation is well-documented, but the real advantage lies in its steroid-sparing profile. Systemic absorption is negligible-serum calcium remains stable even with chronic use. This isn't just efficacy; it's pharmacokinetic elegance.
vanessa parapar
September 24, 2025 AT 08:46Everyone says this works but have you actually seen the side effects? My cousin got burned so bad she looked like she’d been in a sauna with a blowtorch. Don’t be fooled by the ‘low risk’ marketing.
Sakthi s
September 25, 2025 AT 20:37Works. Just be consistent. No magic, just science.
Robert Altmannshofer
September 26, 2025 AT 01:42I used to hate applying this stuff-it felt greasy, smelled weird, and I’d forget half the time. But after 3 months? My scalp’s been clear for a year. Worth the weirdness. Also, pairing it with a salicylic acid shampoo? Chef’s kiss.
Ben Wood
September 28, 2025 AT 01:27Wait-so you’re telling me… this… this *synthetic vitamin D analog*… is somehow better than… steroids? I mean… come on. The FDA says it’s Category C-so it’s basically a gamble. And you’re just… trusting it? Like… what if your kid uses it? What if your dog licks it off? What if the sun hits it wrong?!!
Shannon Wright
September 28, 2025 AT 18:16As someone who’s treated scalp psoriasis for over 15 years-first with coal tar that stained everything, then with steroids that thinned my skin, and now with calcipotriol-I can say this is the first treatment that feels sustainable. It doesn’t erase the condition, but it transforms it from a daily battle into a manageable routine. The key is consistency. Don’t skip days. Don’t expect overnight results. And please, please, don’t stop because it feels better after two weeks. That’s when the real healing begins.
Abhi Yadav
September 28, 2025 AT 20:11It’s not about the drug… it’s about the cosmic alignment of your cells with the universe’s natural rhythm. Vitamin D is sunlight. Sunlight is life. Calcipotriol is just a vessel. Are you ready to receive the light? 🌞
Rachel Nimmons
September 29, 2025 AT 11:10Did you know the FDA approved this in 2001? That’s the same year they approved the first GMO salmon. Coincidence? I think not. They want you dependent on synthetic hormones so they can control your immune system. And the ‘negligible absorption’? That’s what they told us about glyphosate too.
Kathleen Koopman
September 30, 2025 AT 08:38So if I use this and then go out in the sun… will I get a tan? 😅
Melania Dellavega
October 2, 2025 AT 07:35I used to feel so alone with this condition-like no one understood the shame of scratching in public or the dread of white flakes on black clothes. This treatment didn’t just clear my scalp-it gave me back my confidence. I still have bad days, but now I know it’s temporary. You’re not broken. You’re just healing.
Julia Jakob
October 3, 2025 AT 16:44Okay but honestly? I tried this and it made my scalp feel like sandpaper. Like… I rubbed it in and then my skin started peeling off in sheets. I thought it was supposed to help? Maybe I just did it wrong. Or maybe it’s just not for me. Either way, I’m going back to coconut oil and vibes.
Nancy M
October 4, 2025 AT 02:17In India, we use neem and turmeric pastes for generations. This pharmaceutical approach is interesting, but I wonder if we’ve lost touch with holistic healing. Is calcipotriol really better than a balanced diet, stress reduction, and herbal oils? Or are we just chasing the next patent?
gladys morante
October 5, 2025 AT 22:27I used this for 3 weeks and my scalp started bleeding. I cried. I called my mom. I told her I was ruined. I stopped. I’m never trying it again. This isn’t medicine. It’s torture with a prescription.
Precious Angel
October 7, 2025 AT 03:21Let me tell you something-this isn’t about psoriasis. It’s about control. The pharmaceutical industry doesn’t want you cured. They want you addicted to topical treatments so you keep buying tubes every month. They don’t care if you’re clear-they care if you’re a customer. And now they’ve got you hooked on ‘vitamin D analogs’ like it’s some kind of miracle. Wake up. It’s all profit.
Bethany Hosier
October 8, 2025 AT 12:47While the clinical efficacy of calcipotriol is statistically significant (p < 0.001), one must consider the ethical implications of off-label usage in pediatric populations under the age of 12, particularly in light of the FDA’s Category C classification and the potential for epidermal barrier disruption in developing dermal architecture. Furthermore, the economic accessibility of generic formulations remains inconsistent across Medicaid and private insurance tiers, raising concerns regarding healthcare equity.
Robert Asel
October 9, 2025 AT 16:28It is imperative to clarify that the assertion that calcipotriol is a ‘game changer’ is not merely an overstatement-it is an unscientific hyperbole. While the PSSI-75 response rate is statistically significant, the absolute improvement in quality-of-life metrics, as measured by DLQI, remains modest. Moreover, the claim regarding negligible systemic absorption is contradicted by a 2018 study in the Journal of Investigative Dermatology, which detected trace calcitriol metabolites in serum after prolonged use. Therefore, the characterization of this agent as ‘safe’ is misleading. One must approach with caution, not enthusiasm.