Bursitis and Tendinitis: How to Tell Them Apart and Treat Them Right
 Dec, 4 2025
Dec, 4 2025
When your shoulder aches after lifting, your knee hurts when you kneel, or your heel burns after a long walk, it’s easy to blame "arthritis" or just call it "overuse." But if you’ve been dealing with this kind of pain for weeks, you might actually have bursitis or tendinitis-two very different problems that look similar but need totally different treatments.
What’s the Difference Between Bursitis and Tendinitis?
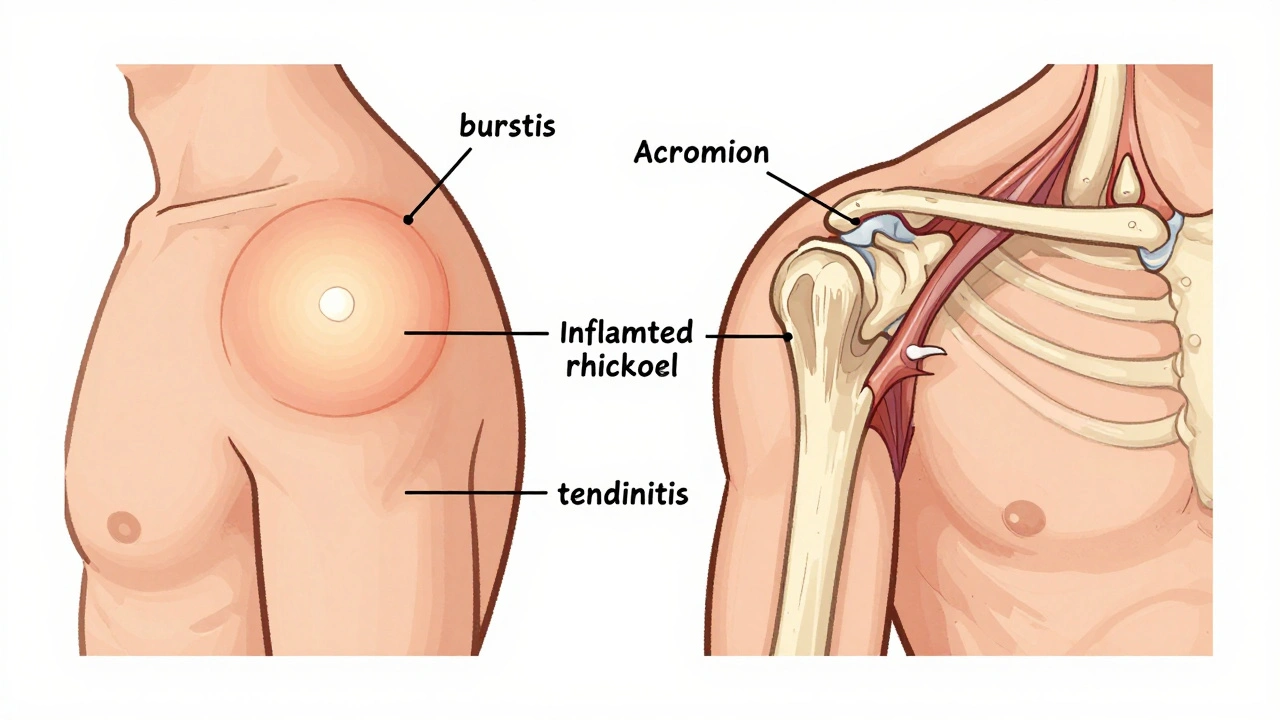
Bursitis and tendinitis both cause joint pain, but they affect completely different parts of your body. Think of it this way: your joints aren’t just bone meeting bone. Between the bones, muscles, and tendons, there are tiny fluid-filled sacs called bursae (say: bur-see). These act like shock absorbers, letting things slide smoothly without friction. When one of these sacs gets inflamed, that’s bursitis.
On the other hand, tendinitis happens in the tendons-the tough, rope-like tissues that connect your muscles to your bones. When those get irritated from repeated motion or sudden strain, they swell and hurt. So bursitis is about the cushion, and tendinitis is about the cable.
Common spots for bursitis: the shoulder (subacromial), elbow (olecranon), hip (trochanteric), and front of the knee (prepatellar). For tendinitis, it’s usually the rotator cuff in the shoulder, the Achilles tendon in the heel, or the patellar tendon just below the kneecap.
How Do You Know Which One You Have?
It’s not always obvious. Many people think they have rotator cuff tendinitis when they actually have bursitis. In fact, studies show that in 65% of shoulder pain cases, both are happening at the same time.
Here’s how to tell them apart:
- Bursitis pain feels more like a deep, dull ache around the joint. It often gets worse when you lie on the sore side at night. The area might feel swollen, warm, or even look puffy. Pressing on the spot usually hurts more than moving the joint.
- Tendinitis pain follows the line of the tendon. If your Achilles tendon is inflamed, you’ll feel it along the back of your ankle when you push off your foot. The pain usually spikes during specific movements-like raising your arm overhead or climbing stairs-and fades when you rest.
One key clue: if you get relief from a cortisone shot, it’s more likely bursitis. Studies show 78% of bursitis patients improve within four weeks after an injection. For tendinitis? Only 52% do. And in some cases, injecting a tendon can actually make it weaker.
Why Misdiagnosis Makes Things Worse
Getting the wrong diagnosis doesn’t just mean wasted time-it delays real healing. A 2023 study found that people who were misdiagnosed took three times longer to recover. Why? Because treatments for bursitis and tendinitis are opposites in key ways.
For example, if you have acute bursitis and start doing strengthening exercises too soon, you’ll irritate the already swollen bursa. That’s like poking a balloon that’s about to pop. On the flip side, if you have tendinitis and just rest and ice it, you’ll miss the one thing that actually fixes it: eccentric strengthening.
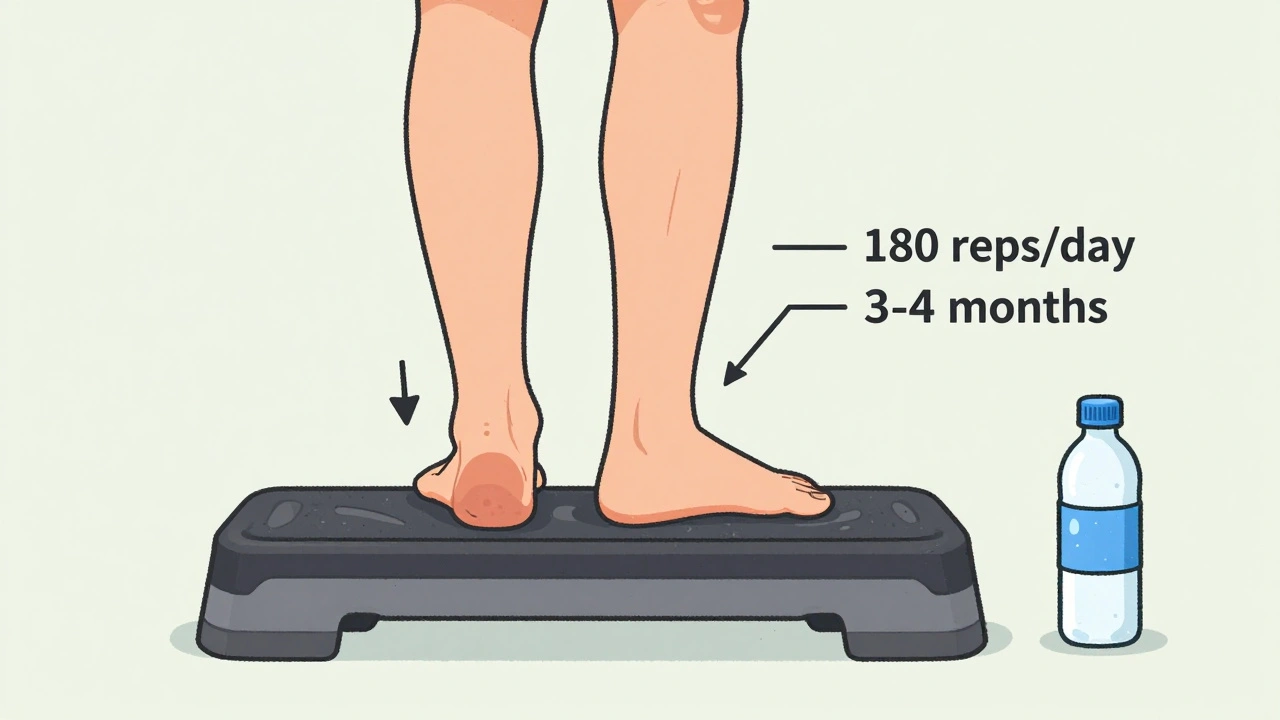
Eccentric strengthening means slowly lowering a weight while the muscle is under tension. For Achilles tendinitis, that’s doing heel drops: standing on a step, raising up on both feet, then lowering down slowly on just the sore foot. Do 180 reps a day for 12 weeks-and yes, it’s grueling. But research shows 68% of people see lasting improvement with this method, compared to just 41% with injections alone.
What Works: The Real Treatment Plan
Most cases of both conditions don’t need surgery. In fact, fewer than 5% of patients ever do. The key is starting with the right conservative approach.
First 7-10 days: Rest the joint. Don’t stop moving completely, but avoid anything that hurts. Apply ice for 15-20 minutes, 3-4 times a day. Use a frozen water bottle for rolling over the Achilles or shoulder-it’s easier to control pressure than an ice pack.
NSAIDs (like ibuprofen): Fine for short-term relief (no more than 10-14 days). They help with swelling, but they won’t fix the root problem. Long-term use can mess with your stomach or kidneys.
For bursitis: After the first week, gentle movement helps. Try slow shoulder circles or hip abductions without resistance. Cortisone injections can be very effective-but only if the bursa is the main issue. Don’t get more than 2-3 in a year. Too many can damage surrounding tissue.
For tendinitis: This is where patience pays off. Start range-of-motion exercises after the first week. Then move into eccentric training. For shoulder tendinitis, that means controlled downward movements with light dumbbells. For the knee, step-downs from a low platform. For the heel, the Alfredson protocol (180 heel drops daily) is gold standard. It takes 3-4 months to see full results, but the pain stays gone longer than with any shot.
What Doesn’t Work (And Why)
Many people try the wrong things because they’re easy or popular.
- Stretching alone: Stretching a tendon that’s already inflamed can make it worse. You need to strengthen it, not just pull on it.
- Heat therapy too early: Heat feels good, but it increases swelling in the first week. Save it for after the inflammation settles.
- Over-the-counter braces: They might feel supportive, but they don’t fix movement patterns. If your posture or technique is causing the problem, a brace just hides it.
- Waiting for the pain to go away: Tendinitis doesn’t heal on its own. If you ignore it, you risk a full tear. A ruptured Achilles tendon requires surgery and months of rehab.
Real People, Real Results
On Reddit’s r/PhysicalTherapy, one user shared how he thought he had a rotator cuff tear. After six months of pain, a physical therapist diagnosed bursitis. He stopped lifting weights, started ice rolling, and corrected his desk posture. Within six weeks, the pain was gone.
Another user, a runner with chronic Achilles pain, tried rest, stretching, and even PRP injections. Nothing worked. Then she found the Alfredson heel drop protocol. She did 180 reps every day for 16 weeks. She didn’t run for three months. But when she started again, she didn’t have a single flare-up in two years.
And on MyHealthTeams, 73% of users who used frozen water bottles for ice rolling said it was more effective than regular ice packs. Why? Better control. You can roll it directly over the inflamed spot without numbness or cold burns.

When to See a Doctor
You don’t need to rush to the ER for this. But if:
- The pain lasts more than two weeks despite rest and ice
- You can’t move the joint without severe pain
- You notice redness, fever, or the area feels hot to the touch
- You heard a pop or felt sudden weakness
…then get it checked. Ultrasound is the best first imaging tool-it’s accurate, fast, and doesn’t use radiation. MRI is overkill unless you suspect a tear.
Prevention Is Easier Than You Think
These conditions aren’t random. They’re caused by repeated stress. So prevention is about changing how you move.
- If you sit at a desk all day: adjust your chair so your shoulders stay relaxed, not hunched. Use a forearm rest if you type a lot.
- If you run or walk: replace your shoes every 300-500 miles. Worn-out soles change your stride and overload tendons.
- If you play sports: warm up properly. Don’t jump into high-intensity movements cold.
- If you kneel at work (plumbers, gardeners, cleaners): use knee pads. A 2023 NIOSH study found construction workers who used pads had 40% less bursitis.
And here’s a simple rule from physical therapists: if an exercise hurts more than a 3 out of 10, stop. You’re not building strength-you’re causing damage.
The Bigger Picture
These aren’t just "old person problems." In 2022, over 387,000 U.S. workers missed time because of bursitis or tendinitis. Musicians, painters, cashiers, and office workers are all at risk. The good news? Most cases respond well to the right plan-no surgery, no drugs, just time and smart movement.
What’s changing now? Wearable tech like the Apple Watch can detect abnormal movement patterns before pain even starts. A 2023 Stanford study showed it spots tendinitis risk with 89% accuracy. That means in the near future, you might get a notification: "Your shoulder motion looks off. Try this stretch."
For now, though, the best tool you have is awareness. Know what’s inflamed. Know what to avoid. And know that healing isn’t about pushing through pain-it’s about working with your body, not against it.
Can bursitis and tendinitis happen at the same time?
Yes, and it’s more common than you think. Studies show that in about 65% of shoulder pain cases, both the bursa and the rotator cuff tendon are inflamed. This is why misdiagnosis is so common-treating just one part won’t fix the problem. A good physical therapist or sports medicine doctor will check both structures during evaluation.
Are cortisone shots safe for tendinitis?
They’re risky. While cortisone helps reduce swelling in bursae, injecting it into a tendon can weaken the tissue and increase the chance of a tear. The American College of Rheumatology recommends limiting cortisone shots to no more than 2-3 per year, and only for bursitis. For tendinitis, they’re not the first-line treatment. Eccentric exercises and physical therapy are safer and more effective long-term.
How long does it take to recover from tendinitis?
It depends on how long you’ve had it and how consistent you are with rehab. Acute tendinitis (under 4 weeks) can improve in 4-6 weeks with rest and gentle movement. Chronic tendinitis (over 3 months) usually takes 12-16 weeks of targeted eccentric strengthening to heal fully. Patience is critical-rushing back to activity is the #1 reason people relapse.
Is tendinitis the same as tendinopathy?
Technically, no. "Tendinitis" implies active inflammation, but many chronic cases show no signs of inflammation on imaging. Experts now prefer the term "tendinopathy" for long-term tendon pain, which includes degeneration and failed healing-not just swelling. This shift matters because treatments for inflammation (like ice and NSAIDs) don’t help degenerative tendons. What works is load management and strengthening, not anti-inflammatories.
Can I still exercise with bursitis or tendinitis?
Yes-but not the way you think. You need to avoid the movement that triggers pain. For example, if shoulder bursitis flares up when you lift overhead, switch to swimming with a flutter kick instead of freestyle. If your knee tendinitis hurts when you squat, try seated leg extensions instead. The goal is to stay active without aggravating the area. Low-impact cardio like cycling or elliptical training is usually safe. Always listen to your body: pain over a 3/10 means you’re pushing too hard.
Do I need an MRI for bursitis or tendinitis?
Usually not. Most cases are diagnosed by physical exam and history. Ultrasound is the preferred imaging tool-it’s accurate, cheaper, and shows real-time movement. MRI is only needed if you suspect a tendon tear, if symptoms don’t improve after 8-12 weeks of treatment, or if there’s unexplained swelling or weakness. Many people over 50 show "tendinitis" on MRI even when they have no pain-so imaging alone doesn’t tell the full story.
Jimmy Jude
December 5, 2025 AT 01:53This is the kind of article that makes me want to scream into a pillow. People think pain is just a glitch in the matrix and pop ibuprofen like candy. Bursitis? Tendinitis? It’s all just your body begging you to stop being a dumbass. You think stretching fixes everything? Nah. You’re just yanking on frayed wires until they snap. And don’t even get me started on cortisone shots - they’re not magic, they’re a temporary bandage on a bleeding artery. Wake up.
Mark Ziegenbein
December 5, 2025 AT 07:24Let me be perfectly clear - the entire medical-industrial complex is built on the illusion of quick fixes. You want to cure tendinopathy? You don’t need injections you need discipline. Eccentric loading isn’t a suggestion it’s a covenant with your own tissue. The Alfredson protocol isn’t a workout it’s a rite of passage. 180 reps a day for 16 weeks? That’s not rehab that’s spiritual warfare against entropy. And if you can’t do it then maybe your pain isn’t physical maybe it’s existential.
Juliet Morgan
December 5, 2025 AT 15:40I had bursitis in my hip for 8 months and this article nailed it. Ice rolling with a water bottle changed my life. No more lying on my side like a wounded animal. Just 15 mins a day and boom - pain went from 8/10 to 2/10. I still do it every morning. You don’t need fancy gear. You just need consistency. And patience. I’m still learning that one.
Harry Nguyen
December 6, 2025 AT 18:12So let me get this straight - you’re telling me the government and Big Pharma don’t want us to know that a frozen water bottle beats a $500 MRI? Of course they don’t. They’re making billions off people who think they need surgery. Meanwhile, the real solution is sitting in your freezer. This is why America’s dying - we’ve forgotten how to be simple. Ice. Rest. Stop lifting. Done.
Stephanie Fiero
December 8, 2025 AT 11:32OMG YES. I did the heel drops and thought I was gonna die. My calves were on fire for weeks. But after 3 months? I ran a 5k without pain for the first time in 4 years. No shots. No meds. Just pure stubbornness. If you’re thinking about quitting - don’t. The pain gets worse before it gets better. But it WILL get better. I promise.
Laura Saye
December 10, 2025 AT 00:18There’s a profound metaphysical dimension to chronic musculoskeletal pain - it’s not merely biomechanical but an embodiment of unprocessed stress. Tendinopathy, as a degenerative phenomenon, reflects a dissonance between the individual’s internal rhythm and the external demands of modern life. The Alfredson protocol, then, becomes a form of somatic meditation - a recalibration of the body’s relationship to load, time, and surrender. We must stop treating tissue as inert matter and recognize it as a sentient archive of lived experience.
Stephanie Bodde
December 10, 2025 AT 17:59THIS. I’ve been there. 🥹 I thought I was broken. Then I found the water bottle trick and started doing the heel drops. I cried the first week. Now I run again. You’re not alone. Keep going. 💪❤️
Mellissa Landrum
December 12, 2025 AT 12:46They don’t want you to know this because the real cure is free. Ice. Rest. Stop lifting. No pills. No machines. No doctors. Just your body and a frozen bottle. Who profits from you getting MRIs? Who profits from your pain? The system is rigged. They’ll sell you a brace, a shot, a surgery - anything but the truth. The truth is simple. And simple is scary.
luke newton
December 12, 2025 AT 19:06I’ve been doing physical therapy for 14 months. I’m not better. I’m not worse. I’m just… tired. Everyone says "just do the exercises" but no one talks about how soul-crushing it is to do 180 heel drops every day for months while your boss yells at you for being late. The system doesn’t care if you’re broken. It just wants you to show up.
James Moore
December 14, 2025 AT 02:35It is, in fact, a matter of profound scientific and cultural significance that the majority of individuals suffering from chronic musculoskeletal discomfort - particularly those afflicted with bursitis and tendinopathy - are systematically misinformed by a medical establishment that prioritizes revenue over recovery. The efficacy of eccentric loading protocols, as validated by peer-reviewed literature from the Journal of Orthopaedic & Sports Physical Therapy, is not merely statistically significant - it is paradigm-shifting. Yet, the persistence of corticosteroid injections as a first-line intervention suggests not ignorance but institutional inertia. One must ask: Who benefits from the perpetuation of the myth that inflammation is the primary driver of tendon pathology? The answer, I fear, lies not in the clinic - but in the boardroom.
Carole Nkosi
December 15, 2025 AT 01:59Who the hell wrote this? This is the most accurate thing I’ve read in years. I’m from South Africa and we don’t have access to fancy clinics. We use ice, rest, and stubbornness. The Alfredson protocol saved my running. No one told me it would take 4 months. I almost quit. But I didn’t. And now? I’m faster than before. This isn’t magic. It’s math. And pain. Lots of pain.
Philip Kristy Wijaya
December 15, 2025 AT 20:13While I appreciate the empirical rigor of the aforementioned protocol, I must interject with a caveat of profound epistemological gravity: the very notion of "tendinitis" as a discrete pathological entity is an artifact of Cartesian reductionism. The human organism is not a machine composed of isolated subsystems. The inflammation of a bursa is invariably correlated with aberrant motor patterning, psychological stress, and systemic metabolic dysregulation. To isolate the tendon or bursa as the locus of pathology is tantamount to blaming the spark for the fire. Therefore, while eccentric strengthening may alleviate symptoms, it does not address the ontological dissonance between the individual and their environment. A holistic recalibration - encompassing sleep, nutrition, breath, and emotional coherence - is not merely advisable. It is imperative.