Blood Pressure Medication Safety in Older Adults: How to Reduce Orthostatic Hypotension Risks
 Jan, 1 2026
Jan, 1 2026
Standing up from a chair and feeling dizzy? For many older adults on blood pressure medication, this isn’t just a momentary blur-it’s a real risk of falling, injury, or hospitalization. Orthostatic hypotension, a sudden drop in blood pressure upon standing, affects up to 26% of older adults with hypertension. And here’s the twist: the very drugs meant to protect their hearts might be making them more vulnerable.
What Is Orthostatic Hypotension-and Why Does It Matter?
Orthostatic hypotension happens when your blood pressure drops at least 20 mm Hg systolic or 10 mm Hg diastolic within three minutes of standing. It’s not just about feeling lightheaded. It’s about balance, falls, and broken hips. In people over 65, a single fall can lead to long-term disability or even death. The problem is growing. With nearly 75 million Americans over 65 having high blood pressure, and up to 19 million of them experiencing orthostatic hypotension, this isn’t a rare side effect-it’s a widespread safety issue.Which Blood Pressure Medications Carry the Highest Risk?
Not all antihypertensives are created equal when it comes to orthostatic risk. Some are far safer than others for seniors.- Alpha blockers (like doxazosin, terazosin) carry the highest risk-up to 28% of older adults on these drugs develop orthostatic hypotension. They relax blood vessels too aggressively, especially when standing.
- Beta-blockers (such as metoprolol, atenolol) increase risk by more than threefold for sustained low blood pressure. They slow heart rate and reduce cardiac output, making it harder to adjust to standing.
- Diuretics (like hydrochlorothiazide) deplete fluid volume. If you’re not drinking enough, this can trigger a sharp drop in pressure when you rise.
- Central sympatholytics (clonidine, methyldopa) interfere with nerve signals that help maintain blood pressure. These are rarely used today but still appear in older prescriptions.
On the flip side, two classes stand out as safer:
- ACE inhibitors (lisinopril, enalapril) and ARBs (losartan, valsartan) show the lowest risk-only 8-10% of users experience orthostatic hypotension. Some studies even suggest they may help prevent it.
- Amlodipine and isradipine (calcium channel blockers) are better tolerated than other CCBs like diltiazem or verapamil, which can cause more pronounced drops in blood pressure in older patients due to slower liver metabolism.
The Myth That Lower BP = More Danger
For years, doctors assumed that pushing blood pressure lower-especially below 130/80-would increase orthostatic hypotension risk. That’s what most people believed. But the data says otherwise. The landmark SPRINT trial followed nearly 9,400 adults over 50 with hypertension. One group aimed for a systolic target under 120 mm Hg. The other targeted under 140 mm Hg. After nearly four years, the intensive group had the same rate of orthostatic hypotension (14.7% vs. 14.5%). More importantly, they had 25% fewer heart attacks, strokes, and heart failure events. No increase in falls. No increase in dizziness. A 2022 meta-analysis of 18,466 patients confirmed this: aggressive blood pressure control actually reduced orthostatic hypotension risk by 17%. Why? Because well-controlled blood pressure stabilizes the system. It’s not the low number-it’s the wild swings that hurt.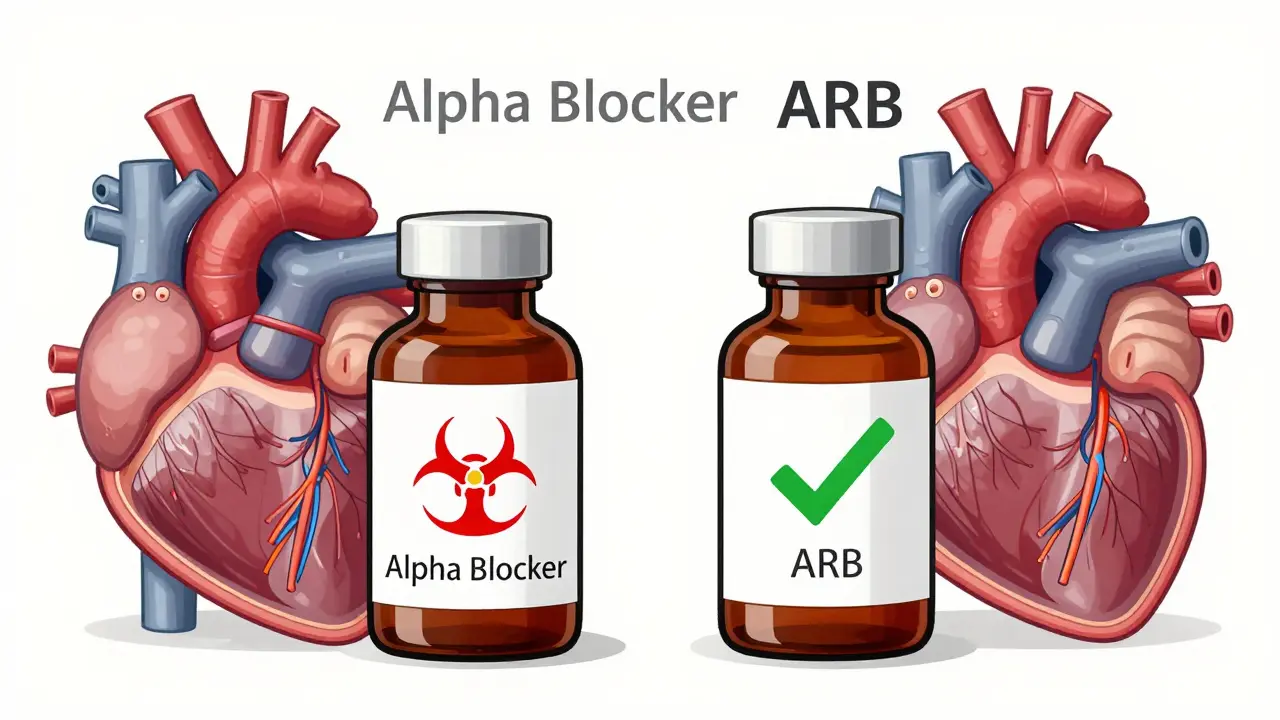
When to Consider Stopping or Switching Medications
If you’re an older adult on blood pressure meds and you’ve had a fall, feel dizzy when standing, or get lightheaded after meals or bathroom trips, it’s time to review your regimen. Don’t stop anything on your own. But do ask your doctor:- Could I be on a medication with higher orthostatic risk?
- Is my dose higher than needed?
- Would switching to an ARB or ACE inhibitor help?
Studies show that 65% of patients who switched from alpha blockers or beta-blockers to ARBs reported fewer dizziness episodes and fewer falls within six weeks. The change isn’t always immediate-it takes 4 to 6 weeks for the body to adjust-but the results are often dramatic.
Also, watch out for non-blood pressure drugs that worsen orthostatic hypotension. SNRIs (like duloxetine), tricyclic antidepressants, nitrates, and even erectile dysfunction pills (like sildenafil) can add to the problem. A full medication review is essential.
Non-Medication Strategies That Work
Medication changes help-but they’re not the whole story. Simple habits can make a huge difference:- Stand up slowly. Sit on the edge of the bed for a full minute before standing. Pause before walking.
- Wear compression stockings. These help push blood back toward your heart and brain. Even over-the-counter ones can reduce dizziness by 30-40%.
- Drink water before standing. A 16-ounce glass of water can raise blood pressure for up to an hour. It’s a cheap, safe trick.
- Eat smaller, more frequent meals. Large meals divert blood to your gut, which can cause post-meal drops in pressure.
- Avoid hot showers or baths. Heat dilates blood vessels and lowers pressure further.
- Sleep with your head slightly elevated. A 6-8 inch wedge under your mattress helps reduce nighttime drops in pressure and improves morning stability.
Patients who practice these habits daily see improvement in 2-4 weeks. No pills needed.

What About Medications to Treat Orthostatic Hypotension?
If lifestyle changes and medication switches aren’t enough, doctors may consider adding drugs like:- Midodrine (Orvaten): A vasoconstrictor that tightens blood vessels. It’s taken 3 times a day, but not after 6 PM-it can cause high blood pressure while lying down.
- Droxidopa (Northera): Boosts norepinephrine to help maintain pressure. Used for neurogenic orthostatic hypotension, often in Parkinson’s patients.
- Fludrocortisone: A steroid that helps retain salt and water. Can cause swelling or heart strain if overused.
- Pyridostigmine (Mestinon): Helps nerve signaling. Less commonly used, but effective for some.
These aren’t first-line solutions. They’re for when the root cause isn’t fixed. They also come with side effects. The goal is always to reduce or eliminate the need for them by optimizing your main blood pressure drugs and habits.
What’s Changing in 2026?
Guidelines are shifting fast. The 2023 update to the American Geriatrics Society Beers Criteria now strongly warns against using alpha blockers and certain beta-blockers in older adults with orthostatic hypotension risk. Insurance companies and pharmacies are starting to flag these prescriptions automatically. New research is underway. The OPTIMISE trial is testing whether personalized blood pressure targets (not just one number for everyone) can reduce falls without increasing heart risks. Early results suggest yes. And the future? Scientists are developing “smart” blood pressure pills that release medication only when you’re upright-so they don’t drop pressure while you’re lying down. Two compounds are already in Phase II trials.Bottom Line: Safety Isn’t About the Number on the Meter
Your blood pressure goal isn’t just a number. It’s about living safely, staying steady, and avoiding falls. For older adults, the safest approach isn’t the lowest BP-it’s the most stable one.- Ask your doctor if your meds are high-risk.
- Consider switching to ARBs or ACE inhibitors if you’re on alpha blockers or beta-blockers.
- Use simple, daily habits to prevent dizziness.
- Don’t assume lower BP is always better-stability matters more.
There’s no need to accept dizziness as normal. With the right medication choices and small daily changes, most older adults can manage their blood pressure without putting themselves at risk.
Can blood pressure medication cause dizziness when standing?
Yes, certain blood pressure medications-especially alpha blockers, beta-blockers, and diuretics-can cause orthostatic hypotension, which leads to dizziness, lightheadedness, or fainting when standing up. This happens because the body can’t adjust blood flow quickly enough. The risk is higher in older adults due to age-related changes in blood vessel elasticity and nerve function.
Are ACE inhibitors and ARBs safer for seniors than other blood pressure drugs?
Yes. ACE inhibitors and ARBs have the lowest risk of causing orthostatic hypotension among common blood pressure medications. Studies show only 8-10% of seniors on these drugs experience dizziness upon standing, compared to up to 28% on alpha blockers. They’re often recommended as first-line options for older adults, especially those at risk for falls.
Should I stop my blood pressure medicine if I feel dizzy?
No. Stopping medication suddenly can raise your blood pressure to dangerous levels, increasing your risk of stroke or heart attack. Instead, talk to your doctor. They can check your blood pressure in both lying and standing positions, review your full medication list, and adjust your treatment safely over several weeks.
Can lifestyle changes reduce orthostatic hypotension without changing meds?
Yes. Simple habits like standing up slowly, drinking 16 ounces of water before getting up, wearing compression stockings, avoiding large meals, and sleeping with your head slightly elevated can reduce dizziness by 30-50%. Many patients see improvement in just 2-4 weeks without any drug changes.
Is it true that lowering blood pressure too much increases fall risk in seniors?
No. Recent large studies, including the SPRINT trial, show that aggressive blood pressure control (targeting under 120 mm Hg) does not increase fall risk. In fact, it reduces heart events and may even lower orthostatic hypotension risk by stabilizing blood pressure overall. The real danger is inconsistent pressure-spikes and drops-not low numbers.
What should I ask my doctor about my blood pressure meds?
Ask: 1) Is my current medication linked to orthostatic hypotension? 2) Could I switch to an ARB or ACE inhibitor? 3) Am I on the lowest effective dose? 4) Should I check my standing blood pressure during visits? 5) Are any of my other meds (like antidepressants or pain pills) making dizziness worse? A full medication review can prevent serious falls.
sharad vyas
January 3, 2026 AT 02:29Interesting post. In India, we don’t always have access to fancy meds, but the simple things-standing slow, drinking water, avoiding hot baths-are what grandmas have taught for generations. Sometimes the oldest advice is the safest.
Ann Romine
January 4, 2026 AT 13:56I’ve seen my mom go through this. She was on doxazosin for years-fell twice. Switched to lisinopril and now she walks the neighborhood every morning without fear. Small changes, big difference.
Todd Nickel
January 5, 2026 AT 12:29The SPRINT trial data is compelling, but I’m curious about the confounding variables. Were the participants in the intensive group more likely to be adherent to lifestyle modifications? Was there a control for physical activity levels, hydration status, or sodium intake? The study’s conclusion that stability-not absolute BP-is the key metric makes sense, but the causality chain feels underexplored in the popular interpretation. The real villain isn’t low BP-it’s the lack of baroreflex adaptation in aging vasculature. We’re treating symptoms, not pathophysiology.
Austin Mac-Anabraba
January 6, 2026 AT 14:57Of course the pharmaceutical industry loves ARBs and ACE inhibitors-they’re patent-protected cash cows. Meanwhile, the real solution-reducing processed food, salt, and sugar-is never mentioned because it doesn’t involve a prescription. They’d rather you take five pills than change your diet. This is medicalization of lifestyle failure disguised as science.
Phoebe McKenzie
January 7, 2026 AT 08:42STOP TELLING PEOPLE TO JUST ‘STAND UP SLOWLY.’ That’s not a solution-it’s a cop-out. If your meds are making you dizzy, you’re being poisoned. Doctors are killing people with this ‘lower is better’ dogma. I’ve lost three friends to strokes because their BP was pushed too low. This isn’t medicine-it’s negligence dressed up as guidelines.
jaspreet sandhu
January 8, 2026 AT 23:22Why do Americans always think new pills are better? In my village, we use ginger tea, salted lemon water, and never stand up fast. No doctor needed. Maybe your problem isn’t medicine-it’s laziness.
Alex Warden
January 10, 2026 AT 01:37China and Russia don’t have this problem because they don’t over-medicate. We’ve turned aging into a disease. Wake up, America. Your doctors are making you weak.
LIZETH DE PACHECO
January 11, 2026 AT 23:53My grandma used compression socks and drank water before getting up. She lived to 96 and never broke a hip. Simple doesn’t mean ineffective. Thank you for sharing this-it’s exactly what my mom needs to hear.
Lee M
January 13, 2026 AT 22:03Stability isn’t just about BP numbers-it’s about rhythm. The body isn’t a thermostat, it’s a symphony. When you disrupt the natural cadence with blunt drugs, you don’t cure-you deafen the system. The goal shouldn’t be to control blood pressure, but to restore the body’s ability to regulate itself. That’s the real medicine.
Kristen Russell
January 14, 2026 AT 12:16This changed everything for me. My dad switched from metoprolol to losartan and now he dances with my mom on weekends. No more falls. No more fear. Thank you.
Liam George
January 14, 2026 AT 22:43Let’s be real-this whole article is a distraction. The real cause of orthostatic hypotension in seniors isn’t meds-it’s glyphosate in the food supply, EMF radiation from smart meters, and the government’s secret fluoride agenda. They want you dependent on pills so they can track your biometrics through your insulin pumps. The ARBs? Just a placebo to keep you docile while they reprogram your autonomic nervous system. Wake up. The system is rigged.