Benzodiazepine Overdose: Emergency Treatment and Monitoring
 Dec, 21 2025
Dec, 21 2025
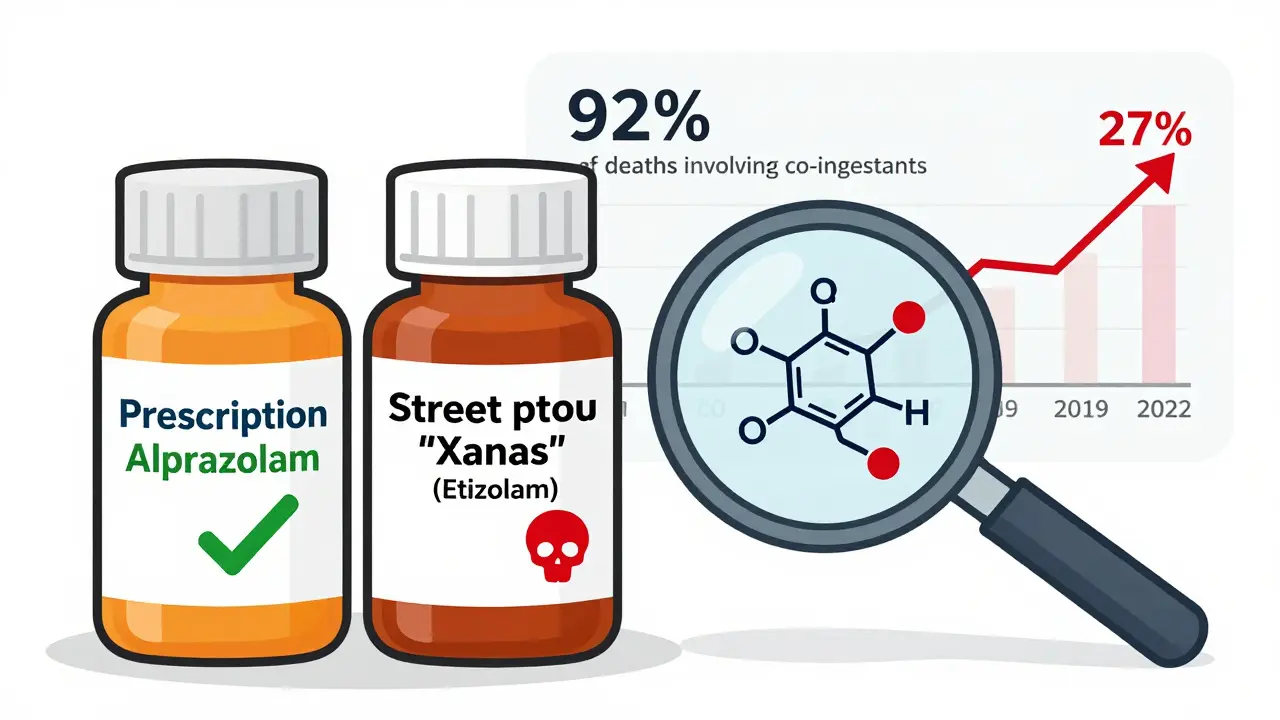
When someone overdoses on benzodiazepines, the biggest danger isn’t the drug itself-it’s what happens when it teams up with something else. A person might take a prescribed pill for anxiety, then have a few drinks or take painkillers. That’s when things turn dangerous. Benzodiazepines slow down the brain. Too much, especially with opioids or alcohol, and breathing can stop. In 2022, the CDC found that 92% of benzodiazepine-related deaths involved other drugs. Isolated benzodiazepine overdoses? Rarely fatal. But mixed overdoses? That’s where the real risk lies.
What Happens During a Benzodiazepine Overdose?
Benzodiazepines like alprazolam, lorazepam, and diazepam work by boosting GABA, a calming chemical in the brain. Too much of it, and the brain shuts down too far. Symptoms start with drowsiness, slurred speech, and unsteady walking. Then comes confusion, slow breathing, and eventually, coma. The Glasgow Coma Scale (GCS) is used to measure consciousness. A score of 8 or lower means the person can’t protect their airway and needs help fast.
Here’s the catch: alprazolam is 3.2 times more likely to cause deep sedation than other benzodiazepines. And newer street drugs like etizolam and clonazolam? They’re 3 to 10 times stronger. The California Poison Control System found these illicit versions made up 68% of severe overdose cases in the Western U.S. in 2022. People don’t always know what they’re taking. That’s why every overdose case needs toxicology screening-not just for benzos, but for opioids, alcohol, and other hidden drugs.
Emergency Treatment: ABCDE, Not Flumazenil
For years, doctors thought flumazenil was the answer. It’s a drug that reverses benzodiazepines. But here’s the truth: flumazenil is rarely the right choice. The American College of Medical Toxicology says it’s only appropriate in 0.7% of cases. Why? Because it can trigger seizures. If someone’s been taking benzos daily for months-even at prescribed doses-flumazenil can yank the drug out of their system too fast. Their brain goes into overdrive. Seizures happen within seconds. One ER nurse on Reddit described watching a patient seize 90 seconds after receiving flumazenil. He’d been taking trazodone with his alprazolam. No one knew.
Today, the standard is ABCDE: Airway, Breathing, Circulation, Disability, Exposure. That’s it. No flumazenil unless the patient is in a hospital with a team ready to handle seizures. Most ERs don’t even stock it anymore. A 2022 survey by the American College of Emergency Physicians found that 78% of departments have stopped keeping flumazenil on hand. The European Resuscitation Council and the American Heart Association both removed it from guidelines in 2021 and 2023, respectively.
What you do instead:
- Check breathing. If it’s under 10 breaths per minute, prepare for intubation.
- Give oxygen through a non-rebreather mask at 15 liters per minute.
- Monitor heart rate, blood pressure, and oxygen levels every 5 to 15 minutes.
- Test blood sugar immediately. Low sugar can mimic overdose symptoms.
- Run a toxicology screen for opioids, alcohol, and other drugs.
Activated charcoal? Only useful if given within 60 minutes of ingestion. After that, the drug’s already absorbed. Hemodialysis? Useless. Benzodiazepines bind tightly to fat and proteins-they don’t wash out.
Monitoring: It’s Not Over When They Wake Up
Many patients get discharged too soon. Sedation fades in 6 to 12 hours. But ataxia-loss of muscle control-can last 24 to 48 hours. That’s a fall risk. Elderly patients or those with liver disease take even longer to clear the drug. One study showed that 28% of cases missed co-ingestants because providers focused only on the benzo.
Proper monitoring means:
- Continuous pulse oximetry and ECG
- Rechecking GCS every hour
- Using the Pasero Sedation Scale to track drowsiness
- Waiting until the patient can walk straight and answer questions clearly
Emergency Care BC recommends a minimum 6-hour observation for asymptomatic patients. Symptomatic patients? Stay until every sign of CNS depression is gone. That could mean 24 to 48 hours. Discharging someone too early is a common mistake-and it’s deadly.
Why the Rules Changed
The shift away from flumazenil didn’t happen overnight. It came from real-world data. In 2021, the CDC found that opioid-benzo combinations increased the risk of respiratory arrest by 15-fold. That’s why the FDA updated benzodiazepine labels in 2022 to warn about this deadly mix. The National Overdose Response Strategy now spends $18.7 million a year training providers to spot these combinations.
But the biggest change? The rise of illicit benzodiazepines. Etizolam, clonazolam, and others are made in labs overseas. They’re cheaper, stronger, and sold as fake Xanax or Klonopin. People think they’re taking a prescription drug. They’re not. These drugs hit harder, last longer, and have no antidote. That’s why overdose cases rose 27% between 2019 and 2022-even as prescriptions dropped 14.3%. The problem isn’t pills from the pharmacy anymore. It’s pills from the street.

What’s Coming Next
There’s new tech on the horizon. In January 2023, the FDA approved a prototype device called BenzAlert™ for clinical trials. It measures benzodiazepine levels in real time with 94.7% accuracy. That means doctors can see exactly when the drug is clearing-and avoid premature discharge.
The NIH is also funding $4.2 million in research to develop longer-acting reversal agents. Flumazenil’s half-life is 41 minutes. That’s why repeat doses are needed-and why seizures happen. A longer-lasting antidote could be a game-changer.
Meanwhile, harm reduction programs are expanding. As of January 2023, 37 U.S. states include benzodiazepine recognition in their naloxone distribution programs. That’s up from just 12 in 2020. First responders are now trained to watch for sedation, not just stopped breathing. It’s a smarter, safer approach.
Bottom Line
Benzodiazepine overdose isn’t about the drug alone. It’s about what it’s mixed with. The best treatment isn’t a miracle drug-it’s careful observation, smart monitoring, and patience. Don’t rush to reverse. Don’t assume it’s just a benzo. Check for opioids. Check for alcohol. Watch for ataxia. Wait until the person is fully alert. Most overdoses resolve on their own. The job of emergency care isn’t to fix it fast. It’s to keep the person alive until their body does.
The future of overdose treatment isn’t in new antidotes. It’s in better education, better screening, and better harm reduction. Because the next person who overdoses might not be taking a prescription. They might be taking something they bought online. And they might not know what’s in it.
Can you reverse a benzodiazepine overdose with flumazenil?
Flumazenil can reverse benzodiazepine effects, but it’s rarely used. It carries a 38% risk of triggering seizures in people with chronic use or dependence. It’s only considered in rare cases-pure overdoses in non-dependent patients with severe respiratory depression. Most emergency departments no longer stock it because the risks outweigh the benefits, especially when opioids or other drugs are involved.
Is a benzodiazepine overdose fatal on its own?
Isolated benzodiazepine overdoses are rarely fatal. Mortality is between 0.01% and 0.05%. The real danger comes from mixing benzos with opioids, alcohol, or other depressants. In 92% of deaths, other substances were involved. That’s why checking for co-ingestants is critical.
How long does a benzodiazepine overdose last?
Sedation usually clears in 6 to 12 hours. But muscle control (ataxia) can linger for 24 to 48 hours, especially in older adults or those with liver problems. Discharging someone too early is dangerous because they’re still at risk of falling or choking. Monitoring should continue until full mental and motor function returns.
Do activated charcoal or dialysis help in benzodiazepine overdose?
No. Activated charcoal only helps if given within 60 minutes of ingestion, and even then, it reduces absorption by only 45%. After that, the drug is already absorbed. Hemodialysis and whole bowel irrigation don’t work because benzodiazepines bind to fat and proteins in the body-they can’t be filtered out. Current guidelines say these treatments have no role in management.
What should you do if you suspect someone overdosed on benzos?
Call 911 immediately. Do not try to make them vomit or give them anything to drink. Stay with them and monitor their breathing. If they stop breathing or become unresponsive, begin CPR if trained. Tell emergency responders everything you know-what they took, how much, and if they used other drugs. This helps providers choose the right treatment.
Gabriella da Silva Mendes
December 21, 2025 AT 12:42Okay but like… why are we still acting like this is a new problem? 😒 People have been mixing Xanax with whiskey since the 90s. The only thing that changed is now the street stuff is 10x stronger and no one knows what they’re holding. I saw a guy at the gas station last week buy ‘Xanax’ that was actually etizolam. He thought he was getting anxiety relief. He got a 3-day coma. 🤦♀️
Sai Keerthan Reddy Proddatoori
December 22, 2025 AT 09:12This is why America is falling apart. You let people take pills like candy, then blame the drug when they die. In India, we don’t have this mess. If you take medicine, you take it with doctor. No drinking, no mixing, no nonsense. This is Western chaos. 🇮🇳
Johnnie R. Bailey
December 23, 2025 AT 13:39What’s fascinating here isn’t just the pharmacology-it’s the systemic abandonment of clinical judgment. Flumazenil was never a silver bullet, but we clung to it because it felt like control. The real tragedy? We replaced one myth (‘there’s an antidote’) with another (‘just watch and wait’). But watching isn’t passive-it’s active, meticulous, and demands resources we’re unwilling to fund. We’ve turned overdose care into triage theater. And the people paying the price? The ones who never had a chance to ask for help.
Also-illicit benzodiazepines aren’t just stronger. They’re unregulated, untraceable, and often laced with fentanyl. That’s not a pharmacology problem. That’s a criminal supply chain. And until we treat it like one, we’re just rearranging deck chairs on the Titanic.
Kathryn Weymouth
December 25, 2025 AT 01:43Minor correction: The Pasero Sedation Scale is specifically validated for post-anesthesia and ICU use-not general emergency departments. Many ERs use the Ramsay Scale or even just clinical judgment. Also, the 28% missed co-ingestants stat-was that from retrospective chart reviews? If so, it’s likely an underestimate. I’ve seen cases where patients had multiple substances but only the benzo was documented because it was ‘the obvious one.’ We need mandatory toxicology panels, not optional ones.
Herman Rousseau
December 26, 2025 AT 19:50Biggest takeaway? Patience saves lives. 🙌 I used to think if they’re not dead in 2 hours, they’re fine. Nope. One guy I worked with woke up at 8 hours… then fell at 14 hours because his legs still didn’t work. We almost missed it. Now we wait 24 hours if there’s any doubt. No rush. No ego. Just care. And yeah-flumazenil? I haven’t used it in 5 years. Not worth the risk.
Also shoutout to the harm reduction folks pushing naloxone + benzo training. That’s the future.
Vikrant Sura
December 27, 2025 AT 16:0192% of deaths involve other drugs? That’s a lazy statistic. It doesn’t mean the benzo wasn’t the trigger. You can’t blame the alcohol if the person wouldn’t have mixed it without the benzo. This is just corporate spin to make benzos look safer. Also, why is everyone ignoring that these drugs are addictive as hell? We’re treating the symptom, not the cause.
Art Van Gelder
December 27, 2025 AT 17:30Let me tell you about the guy who came in last month. 68-year-old, took his diazepam like clockwork. Then his grandson gave him a ‘sleep aid’ from Amazon. Said it was ‘just a stronger Valium.’ Turned out to be clonazolam. 3x potency. No one knew. He was sitting in the waiting room, nodding off, when his pulse dropped to 38. We intubated him. He woke up 36 hours later, looked at me, and said, ‘I just wanted to sleep.’
That’s the real story. Not stats. Not guidelines. Just a man who trusted a label. And now he’s terrified to take anything. We’re not just treating overdoses-we’re breaking trust in medicine. And that’s scarier than any drug.
Ajay Brahmandam
December 28, 2025 AT 16:07Good breakdown. I’m a nurse in Bangalore and we don’t even have flumazenil here. We just monitor, oxygenate, and wait. Simple. Effective. People think we’re doing less, but we’re doing it right. Also, the 6-hour observation rule? We do 12 minimum. Better safe than sorry. 👍
jenny guachamboza
December 29, 2025 AT 11:55Wait wait wait-so you’re saying the FDA approved some ‘BenzAlert’ device?? 😳 Like… a magic scanner? That’s just Big Pharma’s new money grab. They’re gonna charge $5000 per scan and make us all pay for it. And don’t get me started on the NIH funding-this is all just to push new drugs so they can patent them. Flumazenil was fine! They just wanted an excuse to kill it so they could sell something else. 🤨 #Conspiracy