Autoimmune Thyroid Eye Disease: Symptoms and Treatment Progress
 Jan, 3 2026
Jan, 3 2026
Autoimmune Thyroid Eye Disease, also known as Thyroid Eye Disease (TED) or Graves' orbitopathy, isn't just about dry eyes or puffiness. It's a serious condition where your immune system attacks the tissues around your eyes-fat, muscles, and connective tissue-causing swelling, pain, and sometimes permanent vision changes. It’s most common in people with Graves’ disease, but it can also show up in those with underactive or even normal thyroid function. About one in three people with Graves’ disease will develop eye symptoms, often within the first six months after diagnosis. What makes TED tricky is that it doesn’t always match up with how your thyroid feels. You could feel fine, but your eyes could be screaming for help.
What Does Thyroid Eye Disease Actually Look Like?
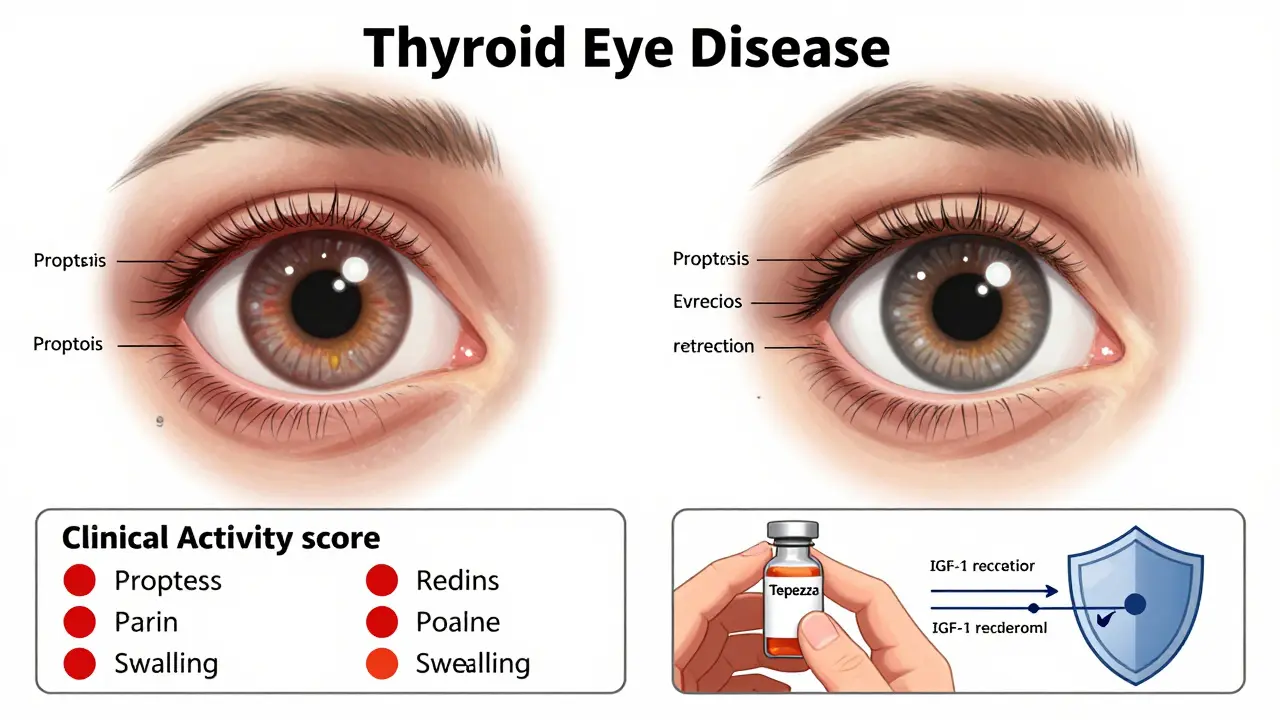
People often mistake TED for allergies or fatigue. But the symptoms are distinct and hard to ignore. The most common sign is bulging eyes-proptosis-where the eyeballs push forward, making you look wide-eyed even when you’re not. About 78% of patients report a gritty, sandy feeling in their eyes, like there’s sand under the lids. Dryness and watery eyes happen together because the inflammation messes with tear production and drainage. Light sensitivity is another big one; 60% of patients can’t stand bright lights or glare.
Double vision affects about half of those with moderate to severe TED. It’s not just annoying-it can make driving, reading, or even walking down stairs dangerous. Pain behind the eyes, especially when moving them up or down, is reported by 40-60% of patients. And if you can’t fully close your eyelids, which happens in 45% of cases, your cornea is at risk. Without treatment, 15-20% develop corneal ulcers, which can lead to scarring and vision loss.
One of the most telling signs is asymmetry. In 70% of cases, one eye is noticeably worse than the other. That’s not normal aging or tiredness-it’s inflammation targeting tissue unevenly. And in severe cases, the optic nerve gets squeezed. Color vision changes are often the first warning sign here. If you start seeing reds as dull or blues as washed out, that’s not normal. It means your vision is already under threat.
How Is It Diagnosed?
There’s no single test for TED. Diagnosis requires putting together pieces from multiple exams. Thyroid function tests-TSH, free T4, free T3-are the first step. But the real clue is the anti-TSHR antibody level. In 75% of cases, higher levels mean more severe eye disease. That’s why doctors don’t just check your thyroid; they check your immune system’s fingerprints.
Eye exams go deeper than a basic vision test. Doctors use the Clinical Activity Score (CAS), which looks at seven signs: redness, swelling, pain with movement, and more. A score of 3 or higher means active inflammation-time to act. Imaging is often needed. Orbital CT or MRI scans show which eye muscles are swollen. The medial rectus muscle is affected in 90% of cases, followed by the inferior rectus. That’s why looking up or down often hurts the most.
Optical coherence tomography (OCT) checks for swelling in the optic nerve, while visual field tests catch early signs of nerve damage. And don’t overlook simple measurements-how far your eyelids sit from your pupil, how much your eyes bulge out. These numbers matter. They’re tracked over time to see if treatment is working.
Treatment Has Changed Dramatically in the Last Five Years
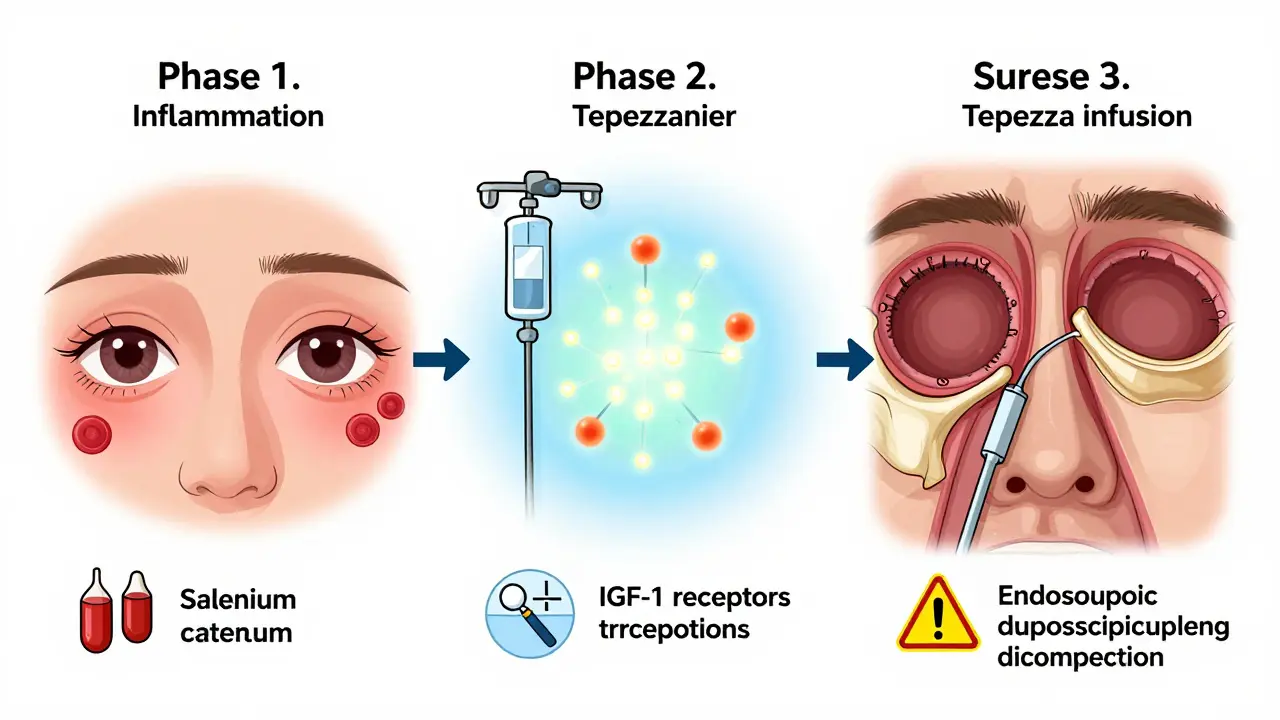
Before 2020, treatment was limited. Mild cases got selenium supplements-100 mcg twice daily-which can reduce progression by 35%. Moderate to severe cases were treated with high-dose steroids like methylprednisolone. But steroids come with risks: liver damage in 15% of patients, blood sugar spikes in 25-30%, and mood swings that make life harder.
Then came teprotumumab (Tepezza). Approved by the FDA in January 2020, it was the first drug designed specifically for TED. It targets the IGF-1 receptor, which plays a key role in the inflammation cycle. In clinical trials, 71% of patients saw their eyes bulge less-compared to only 20% on placebo. Double vision improved in 68% of those on Tepezza, versus 29% on placebo. That’s not a small improvement. That’s life-changing.
But it’s not cheap. Each infusion costs about $5,500. A full course is eight infusions, spaced three weeks apart-totaling around $44,000. Insurance often fights it; 35% of initial requests get denied. Still, for many, it’s worth fighting for. Patients report being able to drive again, sleep without eye pain, and look in the mirror without dread.
Side effects happen. Muscle cramps are common-82% of users on Reddit reported them. A small number (12%) experienced hearing loss, which led the FDA to require stricter monitoring in 2022. But for most, the trade-off is worth it. The 2022 OPTIC-X study showed that 85% of people who responded to Tepezza still had improvement a year later. This isn’t just masking symptoms-it’s changing the disease’s course.
Surgery Comes Later, But It’s Still Vital
Tepezza doesn’t fix everything. Once the inflammation calms down-which takes one to three years-you’re left with scarring, misaligned eyes, or eyelids that won’t close. That’s when surgery steps in.
Orbital decompression surgery removes bone around the eye socket to create more space. It’s done in 5-10% of cases, mostly when the optic nerve is compressed. Today, 65% of these are done endoscopically-through the nose-with fewer scars and faster recovery than old-school external approaches.
Strabismus surgery repositions eye muscles to fix double vision. It works in 30-40% of cases, but only after the disease has been inactive for at least six months. Eyelid surgery to correct retraction is done in 25-35% of patients. Success rates are 75-85% when timed right.
Here’s the catch: most people need more than one surgery. About 20% go through multiple procedures over time. That’s why care needs to be coordinated. You need an endocrinologist, an ophthalmologist, and often an oculoplastic surgeon-all talking to each other.
Smoking Makes Everything Worse
If you have TED and you smoke, you’re making it harder for any treatment to work. Smoking increases your risk of developing TED by 7.7 times. If you already have it, smoking doubles your chance of ending up with severe disease. Quitting isn’t just good advice-it’s medical necessity. Studies show that even after quitting, the risk drops over time. But the longer you wait, the more damage you risk.
Why So Many People Are Misdiagnosed
It takes an average of six months for someone with TED to get the right diagnosis. Primary care doctors mistake it for allergies, sinus infections, or dry eye syndrome 47% of the time. That delay is dangerous. The window for the best treatment-especially with Tepezza-is within the first 12 months. After that, inflammation turns to scar tissue, and drugs can’t undo it.
Only 32% of primary care physicians correctly identify TED on first sight. But oculoplastic surgeons get it right 92% of the time. That’s why going to a specialized TED clinic matters. Major hospitals now offer coordinated care teams that cut diagnosis time by 45 days. If you suspect TED, don’t wait. Ask for an endocrinologist and an ophthalmologist who specialize in thyroid eye disease.
Life Beyond the Diagnosis
TED doesn’t just hurt your eyes-it hurts your life. In a 2022 survey, 74% of patients reported anxiety or depression. 63% felt embarrassed by their appearance. 52% couldn’t drive at night because of double vision. Some lost jobs. Others were passed over for promotions because people assumed they were tired, angry, or unwell.
Support helps. The Graves’ Disease & Thyroid Foundation runs a patient navigator program that’s helped over 12,000 people. There’s also a mobile app called TED Tracker, used by 8,500 people to log symptoms and track their Clinical Activity Score. Knowing what’s happening and having a record makes you a stronger advocate for your own care.
And the future looks brighter. Tepezza is now approved for teens as young as 12 in Europe. New drugs like rituximab and satralizumab are in late-stage trials. Researchers are even working on vaccines that could stop TED before it starts-by blocking the antibodies that trigger it. This isn’t just about treating symptoms anymore. It’s about stopping the disease before it takes hold.
What You Should Do Now
If you have Graves’ disease and notice any eye changes-bulging, redness, double vision, pain-see a specialist within 30 days. Don’t wait for it to get worse. If you don’t have Graves’ but have unexplained eye symptoms, ask for thyroid tests and anti-TSHR antibody screening.
If you’re already diagnosed, know your phase. Are you in active inflammation? Then focus on stopping the damage-Tepezza, selenium, steroids. Are you in the inactive phase? Then focus on restoring function-surgery, vision therapy, eyelid repair.
And if you smoke-stop. No matter how hard it is, it’s the single most effective thing you can do.
TED is rare, but it’s real. And with the right care, it doesn’t have to define your life anymore.
Can thyroid eye disease go away on its own?
Yes, but not always in a good way. The active inflammatory phase usually lasts one to three years and then stabilizes. Symptoms like redness and swelling may improve, but structural damage-bulging eyes, double vision, eyelid retraction-often remains. Without treatment, this damage can become permanent. Waiting for it to "go away" can mean missing the window for effective therapy like Tepezza, which works best early on.
Is Tepezza covered by insurance?
Coverage varies. While Tepezza is FDA-approved and clinically proven, insurance companies often deny initial requests-35% of applications are rejected. Many require proof that steroids failed or that the disease is active (Clinical Activity Score ≥3). Appeals are common and often successful with doctor support. Patient assistance programs through Horizon Therapeutics can help with out-of-pocket costs if denied.
Can you get TED without having Graves’ disease?
Yes, but it’s rare. About 90% of TED cases happen with Graves’ disease (hyperthyroidism). However, a small percentage-around 5-10%-occur in people with hypothyroidism (Hashimoto’s) or even normal thyroid levels. The same antibodies (anti-TSHR) are often present, suggesting the immune system is targeting eye tissue independently. Always check thyroid function if you have unexplained eye symptoms.
Does stress make thyroid eye disease worse?
Stress doesn’t directly cause TED, but it can worsen autoimmune activity overall. High stress levels may trigger immune flare-ups, potentially accelerating inflammation in the eyes. While not a direct cause, managing stress through sleep, exercise, or therapy can support better immune balance and may help reduce symptom severity.
How long does Tepezza treatment last?
A full course of Tepezza is eight infusions, given every three weeks, totaling about 21 weeks (five months). Most patients start noticing improvements within the first few weeks-reduced swelling, less pain, better eye movement. The full effect is usually seen by the end of treatment. Long-term studies show that 85% of patients maintain their improvements for at least a year after the last infusion.
Are there natural remedies that help with TED?
Selenium is the only natural supplement with proven benefit. Taking 100 mcg twice daily during the early stages can reduce progression to moderate or severe disease by 35%. Other supplements like omega-3s or turmeric may help with general inflammation, but there’s no solid evidence they affect TED specifically. Never replace medical treatment with unproven remedies-TED can cause permanent vision loss.
Can TED come back after treatment?
Relapse is uncommon after successful Tepezza treatment. Most patients maintain long-term improvement. However, if the underlying autoimmune condition (like Graves’) remains active, new inflammation can occur. That’s why ongoing thyroid monitoring and avoiding triggers like smoking are critical. Surgery can also need revision if scarring changes over time.
Is TED hereditary?
TED itself isn’t directly inherited, but the tendency to develop autoimmune thyroid disease runs in families. If a close relative has Graves’ disease or Hashimoto’s, your risk of developing TED increases. Genetics play a role, but environmental triggers-like smoking, stress, or infection-are usually needed to start the disease.
Michael Burgess
January 5, 2026 AT 01:36Just had my 4th Tepezza infusion last week. The difference in eye pain is insane - I can finally sleep without my eyes feeling like they’re stuffed with gravel. Also, my wife said I stopped looking like a startled owl. Small wins, right? 🙌
Kerry Howarth
January 6, 2026 AT 16:54Smoking cessation isn’t optional if you have TED. Period. I quit after my diagnosis and my CAS score dropped from 5 to 1 in 8 weeks. Your eyes don’t care about your excuses.
Hank Pannell
January 8, 2026 AT 07:45What’s fascinating is how Tepezza targets the IGF-1 receptor - it’s not just immunosuppression, it’s pathway modulation. The fact that it reverses proptosis rather than just halting progression suggests we’re finally addressing the root signaling cascade, not just downstream inflammation. This isn’t just a drug - it’s a paradigm shift in autoimmune orbital biology. The 85% durability rate in OPTIC-X? That’s not placebo. That’s disease modification.
Neela Sharma
January 9, 2026 AT 07:28They say the eyes are windows to the soul… but for us? They’re the battlefield. I used to avoid mirrors. Now I catch myself smiling at my reflection - not because I’m fixed, but because I’m fighting. And that’s enough for today. 💛
Angela Goree
January 10, 2026 AT 17:01Why is this drug so expensive? Because American pharma is a cartel. I paid $38K out of pocket after insurance denied it TWICE. Meanwhile, the CEO of Horizon made $140M last year. This isn’t medicine - it’s exploitation dressed in lab coats.
Liam Tanner
January 11, 2026 AT 01:34For anyone feeling alone in this - you’re not. I’ve met people from Nigeria to Norway who’ve been through this. TED doesn’t care where you’re from, but community does. Find your tribe. Talk. Share your OCT scans. Ask for help. We’ve all been there.
Ian Ring
January 12, 2026 AT 12:09Just wanted to say - I’m so glad I found this thread. My wife had TED, and we were lost until we got to the Mayo Clinic’s specialized team. The endoscopic decompression? Life-changing. She can blink normally again. Thank you for sharing this. 🙏
Shanahan Crowell
January 13, 2026 AT 15:40Tepezza’s muscle cramps? Real. I got them bad. But I started magnesium glycinate at night and electrolyte sips during infusions - cramps dropped from daily to once a week. Small tweaks, big difference. Don’t suffer in silence - tweak your protocol.
Ian Detrick
January 14, 2026 AT 20:28It’s wild how medicine can be so advanced yet so slow to reach people. I waited 14 months for diagnosis. By then, my optic nerve was already compromised. If you’re reading this and you’ve got unexplained eye changes - don’t wait for the perfect doctor. Go to the first oculoplastic surgeon you can find. Even if they’re 3 hours away. Your vision isn’t negotiable.
veronica guillen giles
January 15, 2026 AT 03:12Oh wow, so now we’re supposed to be grateful because Tepezza works? Let me guess - next they’ll tell us to thank the pharmaceutical gods for letting us live. Meanwhile, the insurance reps still ask if we’ve tried "warm compresses and rest."
Shruti Badhwar
January 16, 2026 AT 07:51As a physician in Mumbai, I’ve seen TED in patients with no access to Tepezza. We use steroids, selenium, and palliative care. Many lose vision. The disparity is not just economic - it’s moral. Why should access to sight depend on geography or insurance approval? This is not a luxury - it’s a human right.
Tiffany Channell
January 17, 2026 AT 08:59Let’s be real - 71% response rate sounds great until you realize 29% still end up with permanent damage. And the hearing loss? That’s not a side effect - it’s a warning sign they buried in the fine print. This drug isn’t a miracle. It’s a gamble with your ears.