Autoimmune Overlap: Understanding PBC, PSC, and AIH Combined Features
 Dec, 4 2025
Dec, 4 2025
When your liver starts acting strange - fatigue that won’t quit, itchy skin, blood tests showing odd patterns - doctors usually look for one clear cause. But sometimes, it’s not one disease. It’s two, or even three, tangled together. This is what happens in autoimmune overlap syndromes, where Primary Biliary Cholangitis (PBC), Primary Sclerosing Cholangitis (PSC), and Autoimmune Hepatitis (AIH) show up at the same time. These aren’t rare oddities. They’re real, underdiagnosed, and require a completely different approach than treating each condition alone.
What Exactly Is an Autoimmune Overlap Syndrome?
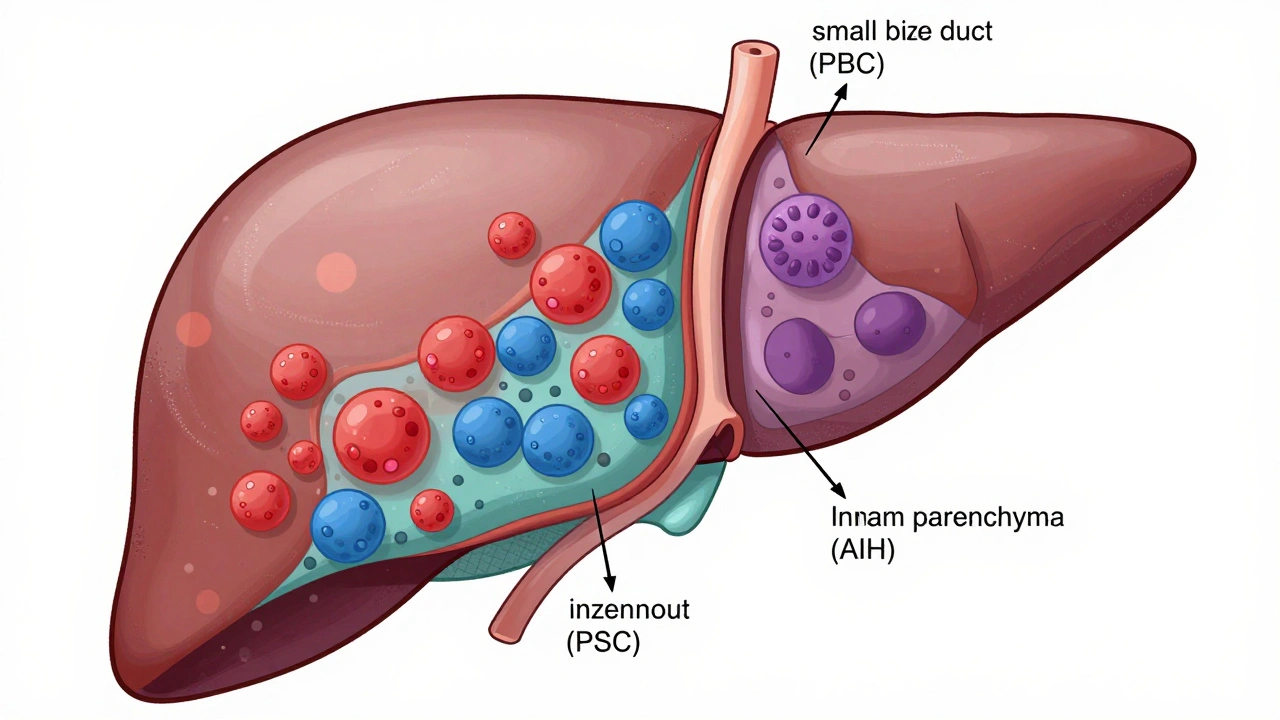
Think of your immune system as a security team. In autoimmune diseases, the team gets confused and starts attacking your own body. In PBC, it targets the small bile ducts in the liver. In PSC, it goes after the larger bile ducts, causing scarring and blockages. In AIH, it attacks the liver cells themselves. When two or more of these attacks happen at once, you’ve got an overlap syndrome. The most common version is AIH-PBC. About 1 to 3% of people with PBC also show clear signs of AIH. In some studies, up to 7% of AIH patients have features of PBC. PSC-PBC overlap? That’s a different story. Despite a few scattered case reports, experts agree there’s no solid evidence this combination truly exists as a distinct syndrome. PSC and AIH together? That happens, but it’s rarer than AIH-PBC. The confusion comes because these diseases don’t always behave like textbook cases. A patient might have the classic blood markers of PBC - like anti-mitochondrial antibodies (AMA) - but also show high liver enzymes typical of AIH. Or their biopsy might show bile duct damage from PBC but also the telltale interface hepatitis of AIH. That’s when doctors start suspecting overlap.How Do You Spot an Overlap? The Clues in Blood and Tissue
Diagnosing a single autoimmune liver disease is hard enough. Diagnosing two at once? It’s like solving a puzzle with half the pieces missing. For PBC, the gold standard is finding anti-mitochondrial antibodies (AMA) in the blood. Around 90 to 95% of PBC patients have them. If they’re not there, doctors look for other antibodies like anti-sp100 or anti-gp210. Blood tests also show high alkaline phosphatase (ALP) and gamma-glutamyl transferase (γ-GT) - signs the bile flow is backed up. AIH looks totally different. Instead of high ALP, you see sky-high ALT and AST - enzymes that leak out when liver cells are damaged. IgG levels are usually elevated, and you’ll find antinuclear antibodies (ANA) or smooth muscle antibodies (SMA). A liver biopsy showing interface hepatitis - immune cells eating away at the edge of liver tissue - confirms it. In an overlap, you get a mix. Someone might have AMA and high ALP (PBC) but also high IgG and interface hepatitis (AIH). That’s the classic AIH-PBC overlap. The diagnostic rule most doctors use? You need to meet at least two out of three criteria for both diseases. It’s not perfect, but it’s the best we have right now.Why PSC Is the Odd One Out
PSC is different. It’s often linked to inflammatory bowel disease, especially ulcerative colitis. It causes thickening and scarring of the big bile ducts, leading to repeated infections and bile buildup. On imaging, you’ll see a “beaded” appearance in the ducts. But here’s the problem: PSC doesn’t have a reliable blood marker like AMA for PBC. The antibodies associated with PSC - like p-ANCA - are also found in other conditions, including AIH. That’s why it’s so hard to say if someone truly has PSC and AIH together. Many experts think what looks like a PSC-AIH overlap might actually be AIH that’s mimicking PSC, or PSC with secondary inflammation. And PBC-PSC overlap? There’s no real evidence it exists. Case reports exist, but they’re outliers. Most researchers believe if someone has features of both, they likely have PSC with some secondary bile duct changes from another process - not a true overlap.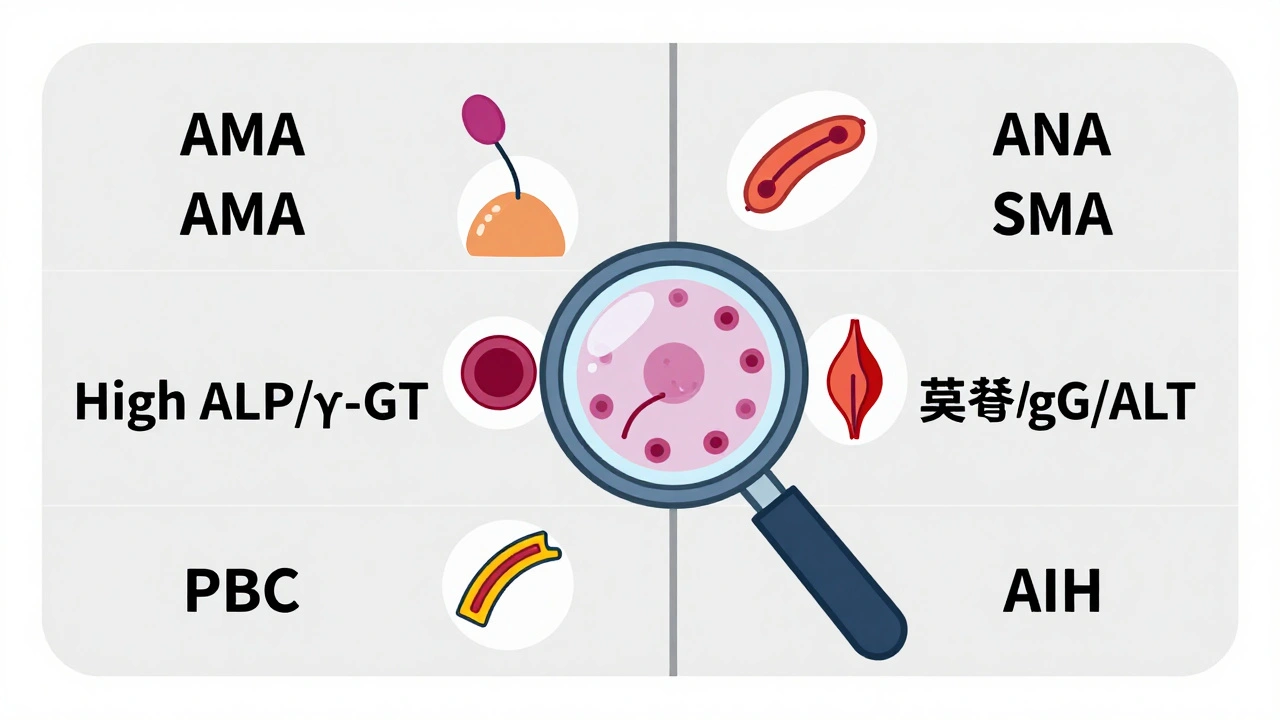
Treatment Isn’t One-Size-Fits-All
This is where things get urgent. Treating AIH-PBC overlap with just one drug usually fails. Standard PBC treatment is ursodeoxycholic acid (UDCA). It helps bile flow and slows damage. Standard AIH treatment is corticosteroids like prednisone, often paired with azathioprine to suppress the immune system. But if you have both? UDCA alone isn’t enough. Studies show 30 to 40% of overlap patients don’t respond to UDCA by themselves. Their liver enzymes stay high. Their fibrosis keeps progressing. That’s when you add immunosuppressants. A 2020 case report described a 39-year-old man with asymptomatic liver enzyme spikes for six years. He was diagnosed with PBC because of AMA and high ALP. But his ALT was also elevated - unusual for pure PBC. A biopsy confirmed interface hepatitis. He started on UDCA. Within months, his ALT didn’t drop. His doctor added azathioprine. Only then did his enzymes normalize. There’s no official protocol. Treatment is personalized. Doctors look at which disease is more active. If AIH features are dominant, they start with steroids. If PBC is the main driver, they begin with UDCA and add immunosuppression if needed. The goal? Stop the damage before cirrhosis sets in.What Happens If It’s Missed?
The biggest danger? Delayed diagnosis. In community clinics, misdiagnosis rates for overlap syndromes are estimated at 15 to 20%. A patient might be told they have “just PBC” and given UDCA. But if they also have AIH, that drug won’t touch the immune attack on liver cells. Over time, their liver keeps getting worse. Untreated overlap syndromes can lead to cirrhosis in 30 to 40% of cases within 10 years - just like pure PBC or AIH. But because the damage comes from two directions, progression can be faster. Some patients end up needing a liver transplant sooner than expected. And the symptoms? They’re vague. Fatigue. Joint pain. Itchy skin. Weight loss. These are easy to brush off as stress, aging, or depression. That’s why specialists emphasize looking beyond the obvious. If a PBC patient has high ALT or IgG, don’t assume it’s just a fluke. Dig deeper.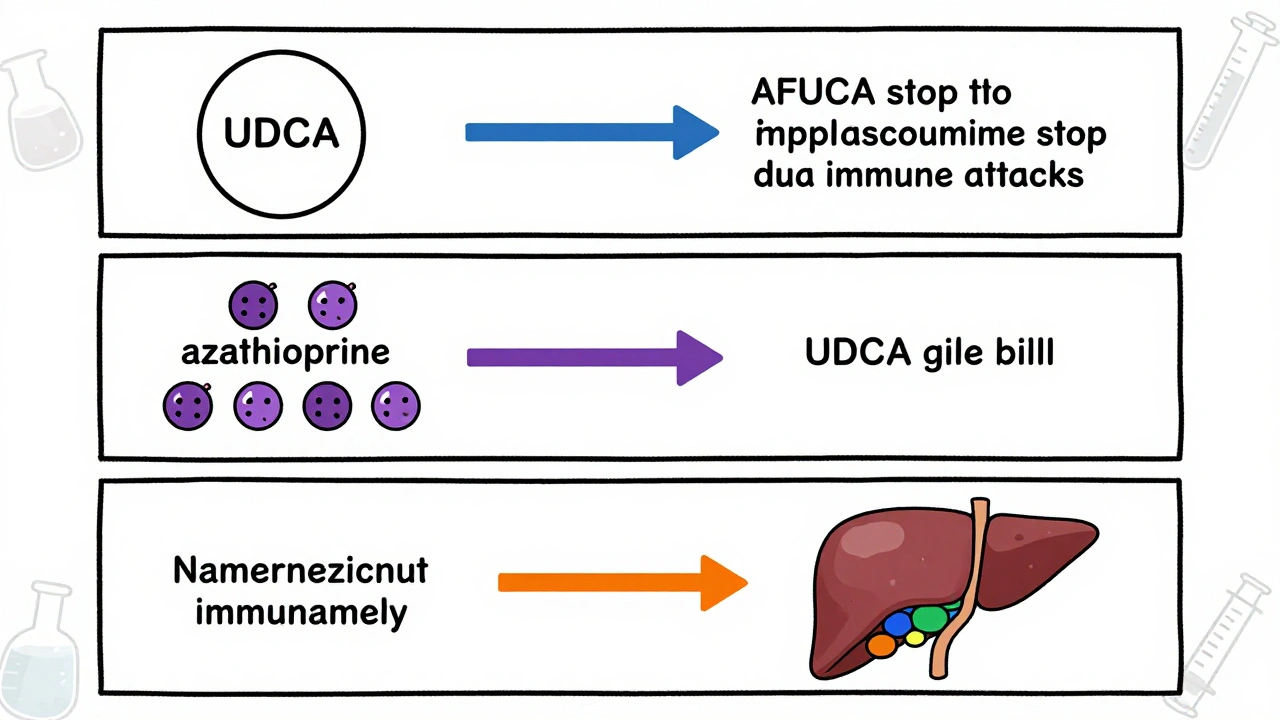
What’s Next for Diagnosis and Treatment?
Right now, the diagnostic criteria for overlap syndromes aren’t validated by large studies. That’s changing. The European Association for the Study of the Liver (EASL) and the International Autoimmune Hepatitis Group are working together on a new set of criteria, with results expected in 2024-2025. Researchers are also finding new autoantibodies beyond AMA - like anti-sp100 and anti-gp210 - that help identify AMA-negative PBC cases. That’s crucial because some overlap patients don’t have AMA at all. There’s growing evidence that autoimmune liver diseases aren’t separate boxes. They’re points on a spectrum. Some people have clear AIH. Others have clear PBC. But many fall in the middle - with features of both. Overlap syndromes might just be the tip of that iceberg. For now, the key is awareness. If you have a liver disease and your treatment isn’t working, ask: Could there be something else going on? If your blood tests don’t fit the pattern, push for a biopsy. If your doctor dismisses it, get a second opinion from a hepatologist who’s seen these cases before.Frequently Asked Questions
Can you have PBC and PSC at the same time?
There’s no clear evidence that a true PBC-PSC overlap syndrome exists. While a few case reports describe patients with features of both, most experts believe these are either misdiagnosed cases or PSC with secondary changes from another condition. The diagnostic criteria for PBC and PSC are too different, and the bile duct damage patterns don’t align in a way that suggests a true overlap.
How common is AIH-PBC overlap?
AIH-PBC overlap is the most common type. Studies show it affects 1 to 3% of people with PBC and up to 7% of those with AIH. Some larger studies report rates as high as 9% in PBC populations. While not rare, it’s still underdiagnosed because its symptoms can look like either disease alone.
Is a liver biopsy always needed to diagnose overlap?
No, it’s not always required - but it’s often critical. PBC can be diagnosed with AMA and elevated ALP alone. AIH is often diagnosed with IgG, autoantibodies, and clinical signs. But when features of both are present, a biopsy is the only way to confirm interface hepatitis (for AIH) and bile duct damage (for PBC). Most specialists recommend a biopsy if there’s any doubt.
Can medications cause overlap syndromes?
Yes. Rare cases have been linked to drugs like hydralazine, used for high blood pressure. These are called drug-induced overlap syndromes. The immune system gets triggered by the medication and starts attacking the liver in ways that mimic both AIH and PBC. Stopping the drug often helps, but some patients still need long-term treatment.
What’s the long-term outlook for someone with an overlap syndrome?
With early diagnosis and proper treatment, many patients do well. The key is using combination therapy - UDCA plus immunosuppressants - when needed. Without treatment, 30 to 40% develop cirrhosis within 10 years. Liver transplantation is still an option for advanced cases, and outcomes are similar to those with single diseases. Lifelong monitoring is essential to catch progression early.
Jessica Baydowicz
December 5, 2025 AT 21:32Okay but like... has anyone else noticed how everyone just shrugs and says 'it's probably just stress' when you're itching nonstop and can't get out of bed? I was told that for 18 months before someone finally looked at my labs again. 🤦♀️
Martyn Stuart
December 6, 2025 AT 22:16Just to clarify-AMA-negative PBC is still PBC, and it’s often the first clue in overlap syndromes. If you have interface hepatitis + elevated IgG + no AMA, don’t dismiss it as 'atypical AIH.' It’s probably AIH-PBC. Biopsy is non-negotiable. I’ve seen too many patients get misdiagnosed because someone skipped the histology.
Gareth Storer
December 8, 2025 AT 22:03So let me get this straight-we’re diagnosing liver diseases based on a checklist written by people who’ve never met a real patient? Cool. Cool cool cool.
Jordan Wall
December 10, 2025 AT 04:39OMG YES. The AMA-PBC-AIH overlap is the *ultimate* diagnostic rabbit hole. I had a patient last month with AMA+, ALP 800, ALT 400, IgG 28, and interface hepatitis-classic. But the rheumatologist swore it was 'just seronegative RA with hepatic involvement.' 😭 We had to fight for the biopsy. Spoiler: it was overlap. UDCA alone? Useless. Added azathioprine-enzymes normalized in 6 weeks. 🤯
Also-anti-gp210 is underused. If you’re AMA-negative but have PBC-like cholestasis, test for it. It’s 95% specific. Why aren’t we doing this first?
And PSC-PBC overlap? Please. That’s like saying you have a unicorn and a dragon in your backyard. Cute story. Not real. PSC is a structural beast; PBC is a ductal autoimmune one. They don’t cuddle.
Also-why are we still calling it 'overlap'? It’s not two diseases crashing into each other. It’s one immune system having a full-on nervous breakdown and attacking everything in sight. We need a new taxonomy.
And yes, hydralazine can trigger this. I’ve seen it. It’s rare, but if someone’s on it and suddenly their LFTs go nuts? Pull the drug. And then biopsy. Don’t just blame the med and move on.
Also-PSC is not 'just IBD with liver issues.' That’s lazy. The bile duct fibrosis is primary. It’s not secondary. Stop saying that.
And no, you don’t need a biopsy for every case. But if your patient’s not responding to UDCA? You’re not being thorough. You’re being negligent.
Also-why is no one talking about the gut-liver axis here? PSC patients have dysbiosis. AIH patients have gut permeability. Is that causal? Or just correlated? We need more microbiome studies.
And the EASL criteria coming in 2024? Long overdue. But let’s hope they don’t just codify the same flawed assumptions. We need phenotyping, not just labeling.
Also-this isn’t just about liver enzymes. It’s about quality of life. Fatigue isn’t 'normal.' Itching isn’t 'just a symptom.' These patients are suffering silently because no one believes them. 😔
TL;DR: If your PBC patient has high ALT or IgG-don’t ignore it. It’s not a fluke. It’s a red flag. And if your doctor says 'it’s fine'-go elsewhere.
Karl Barrett
December 11, 2025 AT 06:48There’s something deeply philosophical about autoimmune overlap-it’s like the immune system doesn’t believe in boundaries. It doesn’t care if you're PBC or AIH. It just sees 'liver' and says 'attack.' Maybe we’re wrong to treat them as separate diseases. Maybe they’re just different expressions of the same underlying immune chaos.
I’ve watched patients go from 'I have PBC' to 'I have PBC and AIH' to 'I have a broken immune system'-and the last one is the most accurate. The labels help us communicate, but they don’t capture the lived experience.
Also, the fact that we still rely on 1980s antibody panels and biopsies is wild. We have single-cell RNA sequencing now. Why aren’t we mapping the immune infiltrates in real time? We’re diagnosing with typewriters while the rest of medicine has smartphones.
Pavan Kankala
December 11, 2025 AT 18:57They don’t want you to know this, but PSC and PBC are both controlled by the same shadowy pharma group that profits from lifelong UDCA prescriptions. The 'overlap' thing? A distraction. They don’t want a cure-they want patients on drugs forever. Wake up.
George Graham
December 12, 2025 AT 01:44Thank you for writing this. I’ve been told for years that my fatigue is 'just anxiety.' I had AMA+ and high ALP, but my ALT was also elevated-my GI doctor said, 'Oh, that’s just inflammation.' It took me going to a hepatologist and demanding a biopsy to find out I had AIH-PBC overlap. I’m on UDCA + azathioprine now. My energy’s better. But I wish someone had told me sooner.
You’re not alone. And you’re not crazy. Keep pushing.
Elizabeth Crutchfield
December 12, 2025 AT 03:33i had the same thing!! i was like 'why am i still so tired??' and my dr was like 'you’re 35, it’s normal' and i was like 'no i’m not, i’m crying in the shower again' and then i found this post and went back to my dr and demanded the biopsy. it was overlap. i’m on meds now and i’m not crying in the shower as much. 🥹
Bill Wolfe
December 13, 2025 AT 06:14Wow. Just wow. Another piece of medical dogma being sold as science. AMA? AIH? Biopsies? Please. These are just markers the industry uses to sell drugs. The real cause? Glyphosate. Mold toxicity. EMFs. The liver is a detox organ. When it’s overwhelmed by modern toxins, it starts attacking itself. No one wants to talk about that because it’s not profitable. But your 'overlap syndrome' is just your body screaming for detox. Try bentonite clay. Saunas. Chlorella. Stop the drugs.
Scott van Haastrecht
December 14, 2025 AT 22:28Oh great. Another 10-page essay from someone who thinks they’re a liver whisperer because they read a NEJM article. You think you’re helping? You’re just scaring people with jargon. 'Interface hepatitis'? 'Anti-gp210'? Who even talks like this? Just tell me if I need a transplant or not. Stop with the 'overlaps' and 'syndromes.' You’re making it worse.
John Filby
December 15, 2025 AT 07:45Just had my first liver biopsy last week-turns out I have AIH-PBC overlap. I’m 28. Never smoked. Never drank. My doctor said ‘weird case.’ I’m on UDCA now and waiting to start azathioprine. Honestly? I’m terrified. But reading this thread helped. I didn’t know I wasn’t alone. Thanks, everyone.
Ben Choy
December 16, 2025 AT 19:03My cousin was misdiagnosed with PBC for 5 years. Then she got a second opinion and found out she had AIH-PBC. She started steroids and now she’s hiking again. 🙌 It’s scary how easy it is to miss this. If you’re not improving-push. Hard.
Rachel Bonaparte
December 16, 2025 AT 21:40Let me tell you what they don’t want you to know-this isn’t autoimmune. It’s not even about the liver. It’s about the gut microbiome being poisoned by Roundup, then the liver being forced to detoxify it, then the immune system getting confused because the liver is leaking endotoxins into the bloodstream, then the body starts attacking bile ducts because it thinks they’re the source. The AMA? It’s a red herring. The real marker is LPS-lipopolysaccharide. The pharmaceutical industry suppresses this because if you fix the gut, you don’t need 10 years of UDCA and azathioprine. And guess what? They’ve known this since 1998. But you won’t hear it from your hepatologist because they’re paid by the drug companies. The truth is buried under layers of profit. Wake up.
Shofner Lehto
December 17, 2025 AT 01:16One of the most thoughtful and clinically accurate summaries I’ve read on this topic. The point about PSC not having a reliable serologic marker is critical. And the push for biopsy when there’s discordance between labs and symptoms? Spot on. I’ve trained residents to think: 'If the disease doesn’t fit the textbook, it’s not because the patient is wrong-it’s because the textbook is incomplete.' This is why we need more hepatologists who think like detectives, not checklist robots.