Agranulocytosis from Medications: Infection Risks and How to Monitor for It
 Nov, 7 2025
Nov, 7 2025
Agranulocytosis Symptom Checker
Check Your Symptoms
This tool helps identify if your symptoms might indicate agranulocytosis. Based on CDC and FDA guidelines, if you're taking high-risk medications like clozapine or antithyroid drugs, recognize these warning signs:
What Is Agranulocytosis, and Why Should You Care?
Agranulocytosis isn’t a common condition, but when it happens, it can turn deadly in hours. It’s when your body stops making enough neutrophils - the white blood cells that fight off bacteria and fungi. Without them, even a minor sore throat or a small cut can lead to a full-blown infection that spreads fast. The absolute neutrophil count (ANC) drops below 100 per microliter. For comparison, a normal ANC is between 1,500 and 7,000. At this level, your immune system is essentially offline.
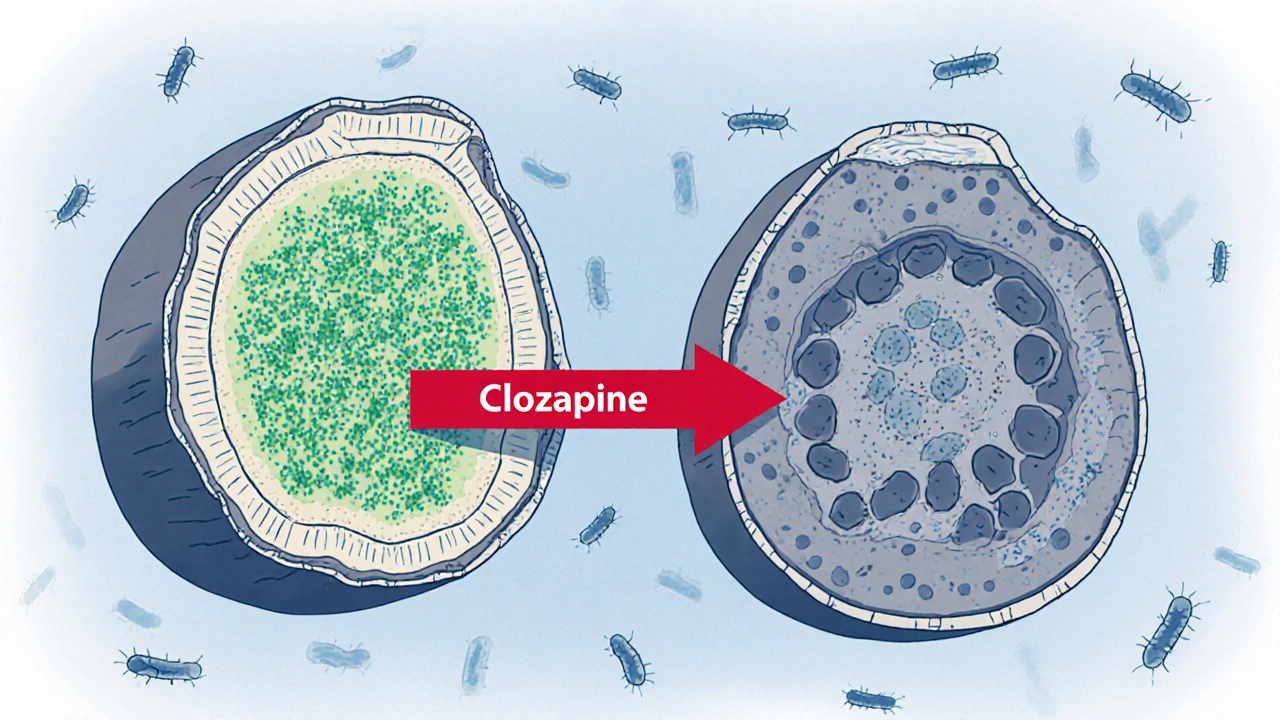
Most cases - about 70% - come from medications. It’s not the drug itself that’s always the problem. It’s how your body reacts to it. Some drugs trigger your immune system to attack your own neutrophils. Others poison the bone marrow where these cells are made. Either way, the result is the same: no defense against infection.
Which Medications Are Most Likely to Cause It?
Over 200 drugs have been linked to agranulocytosis, but only a handful carry real risk. The biggest offender is clozapine, used for treatment-resistant schizophrenia. About 0.8% of people taking it develop agranulocytosis. That sounds low, but in a population of 10,000 patients, that’s 80 cases. Because of this, the FDA requires weekly blood tests for the first six months of treatment. Even then, about 25% of cases happen despite following the rules.
Antithyroid drugs like propylthiouracil and methimazole are next. Propylthiouracil carries a 0.36% risk per year, while methimazole is safer at 0.16%. That’s why many doctors now start with methimazole unless the patient has a specific reason not to.
Antibiotics like trimethoprim-sulfamethoxazole (Bactrim) raise your risk 15 times compared to other antibiotics. NSAIDs like dipyrone (not available in the U.S. but used elsewhere) are also risky. Even common drugs like ibuprofen have almost no link - so don’t panic if you take Advil.
The key isn’t avoiding all meds. It’s knowing which ones need watchful monitoring. Clozapine and propylthiouracil are the top two to watch.
How Do You Know It’s Happening? The Warning Signs
Agranulocytosis doesn’t come with a red flag. It sneaks up. The first sign is often a fever over 38.3°C (101°F). That’s not just a cold. That’s your body screaming that something’s wrong. Other early symptoms include:
- Sore throat or mouth ulcers
- Chills or sweating
- Fatigue that doesn’t go away
- Swollen gums or painful swallowing
Here’s the problem: most people - and even some doctors - mistake these for a flu or a viral infection. A 2022 survey found that 63% of patients had their symptoms dismissed at first. By the time they got a blood test, it was already critical.
If you’re on clozapine, propylthiouracil, or Bactrim, and you develop a fever, don’t wait. Go to the ER. Get an ANC test. Delaying by even 24 hours can increase your chance of death.

How Doctors Diagnose It - And What They Look For
Diagnosis isn’t based on symptoms alone. You need two things:
- Two blood tests showing ANC below 100/μL
- A bone marrow biopsy showing almost no neutrophil precursors
That second part sounds scary, but it’s often not needed if the blood tests are clear and the drug history fits. Many doctors will skip the biopsy if the ANC is below 50 and the patient is on a known high-risk drug.
There’s also a new tool: the HLA-DQB1*05:02 genetic test. Approved by the FDA in early 2023, it checks for a gene variant that makes you 14 times more likely to develop agranulocytosis from clozapine. If you test positive, your doctor might choose a different medication or prepare for tighter monitoring.
Monitoring Protocols - What Works and What Doesn’t
The good news? Agranulocytosis is preventable. The bad news? Many people aren’t monitored properly.
For clozapine, the FDA’s REMS program requires:
- Weekly blood tests for the first 6 months
- Biweekly for months 7-12
- Monthly after that
But a 2020 study found only 68% of U.S. prescribers followed this. Rural areas are worse - 38% of patients there can’t get blood tests on time.
Now there’s a game-changer: the Hemocue WBC DIFF device. It’s a handheld machine that gives an ANC result in 5 minutes, right in the doctor’s office. It’s FDA-cleared and cuts the wait from days to minutes. In one trial, adherence jumped by over 30%. This is especially helpful for patients who travel far for care.
For antithyroid drugs, guidelines now recommend monthly CBCs for the first 6 months, then every 2-3 months. If ANC drops below 1,000/μL, the drug is stopped - even if it’s not yet below 100. That’s a newer standard from the European Hematology Association in 2023. Waiting until it hits 500 is too late.
What Happens If You Get It?
If agranulocytosis is caught early, recovery is likely. Stop the drug. That’s it. Most people’s neutrophil counts bounce back in 1-3 weeks. But if you develop a fever, it becomes a medical emergency.
The Infectious Diseases Society of America says: if you have a fever and ANC under 500, start broad-spectrum antibiotics immediately - especially ones that cover Pseudomonas aeruginosa. This single step cuts death rates from 21% to under 6%.
Some patients need hospitalization, IV antibiotics, and even growth factors like G-CSF to speed up neutrophil recovery. But the key is speed. Every hour counts.
Why Some People Still Die - And How to Avoid It
Deaths from medication-induced agranulocytosis aren’t random. They happen because:
- Patients don’t know the risks
- Doctors don’t check blood counts regularly
- Symptoms are ignored as "just a cold"
- Monitoring isn’t available in rural areas
Dr. Lisa Brown of the CDC found that rural and underserved patients die 2.3 times more often. Why? No access to labs. No hematologists nearby. No point-of-care testing.
Here’s how to protect yourself:
- If you’re prescribed clozapine or propylthiouracil, ask: "What’s my monitoring plan?" Get it in writing.
- Keep a log of your ANC results. Know your baseline.
- Call your doctor immediately if you have a fever - don’t wait for your next appointment.
- Ask about the HLA-DQB1*05:02 test if you’re starting clozapine.
- If you live far from a hospital, ask about portable ANC testing options.
The Future: Better Tools, Fewer Deaths
The field is moving fast. AI-powered alerts in electronic health records can now flag patients whose ANC is dropping too fast - even before the doctor sees it. One study showed a 47% drop in missed cases.
By 2028, 40% of high-risk medications may require genetic screening before you even start taking them. That’s not science fiction - it’s already happening with clozapine.
Pharmaceutical companies are being held accountable. AstraZeneca paid $187 million in lawsuits over Seroquel-related cases. That’s pushing them to improve warnings and monitoring systems.
But the biggest change won’t come from tech. It’ll come from awareness. If you’re on one of these drugs, know your risk. Speak up. Don’t assume someone else is watching your blood counts.
Rachel Puno
November 8, 2025 AT 10:44Steve Phillips
November 9, 2025 AT 05:44Clyde Verdin Jr
November 10, 2025 AT 07:23Brad Seymour
November 11, 2025 AT 08:13Cris Ceceris
November 12, 2025 AT 16:54Malia Blom
November 14, 2025 AT 16:25Erika Puhan
November 15, 2025 AT 19:53Edward Weaver
November 16, 2025 AT 00:24Lexi Brinkley
November 16, 2025 AT 09:52Kelsey Veg
November 16, 2025 AT 13:30Alex Harrison
November 17, 2025 AT 14:18Key Davis
November 19, 2025 AT 10:14Jay Wallace
November 20, 2025 AT 16:07