Duricef (Cefadroxil) vs Other Antibiotics: Detailed Comparison
 Oct, 15 2025
Oct, 15 2025
Antibiotic Decision Tool
Choose Your Scenario
This tool helps you identify which antibiotics are most appropriate for your specific situation based on the article's criteria.
Recommended Antibiotics
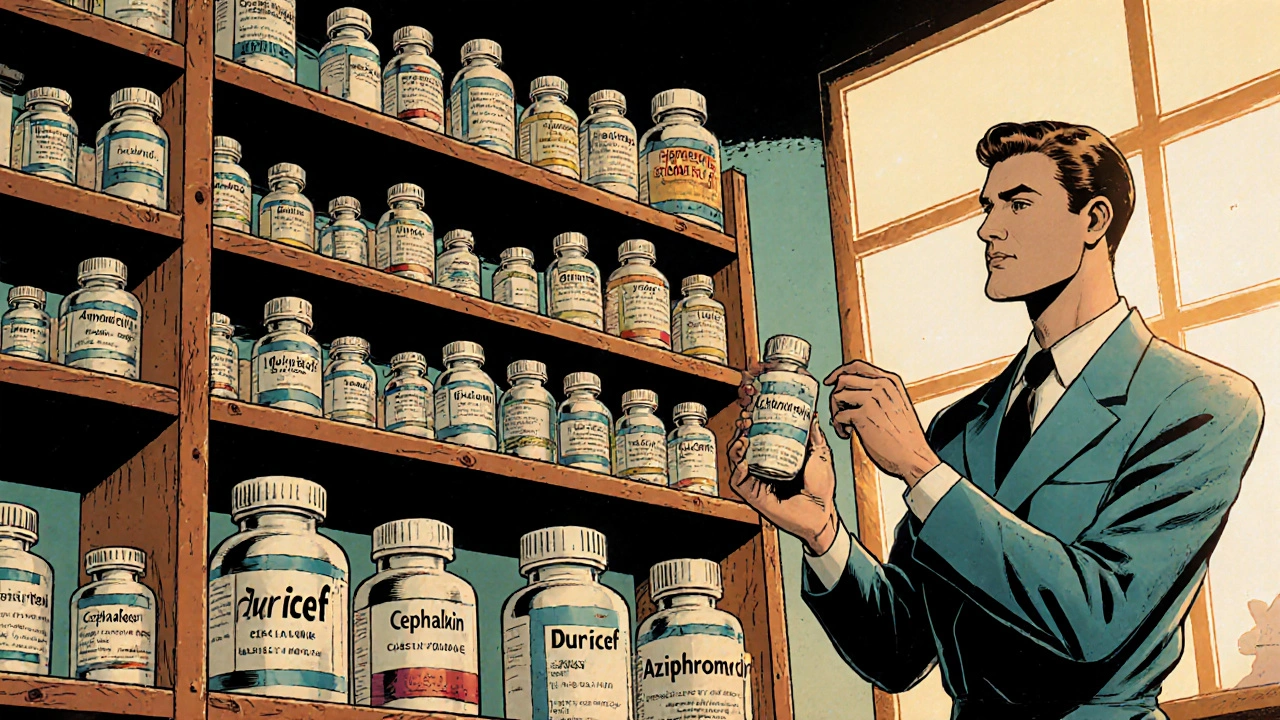
You're trying to decide whether Duricef (cefadroxil) is the right antibiotic for a skin infection, urinary tract infection, or respiratory issue, but the pharmacy shelf is crowded with names like cephalexin, amoxicillin, and azithromycin. This guide breaks down Duricef’s strengths and weaknesses, lines them up against the most common alternatives, and gives you practical criteria to pick the best fit for your situation.
Quick Takeaways
- Duricef is a first‑generation oral cephalosporin with strong activity against gram‑positive bacteria and moderate gram‑negative coverage.
- It’s taken twice daily, which can be easier than three‑times‑daily regimens of some alternatives.
- Common side effects include gastrointestinal upset and rash; severe allergic reactions are rare but possible.
- For patients with a penicillin allergy, Duricef may still be an option, but cross‑reactivity must be assessed.
- When broader gram‑negative coverage or a once‑daily dose is needed, drugs like cefixime or azithromycin might be better choices.
What Is Duricef (Cefadroxil)?
Duricef is a branded formulation of cefadroxil, a first‑generation oral cephalosporin antibiotic that inhibits bacterial cell‑wall synthesis by binding to penicillin‑binding proteins. It was approved in the United States in 1991 and is commonly prescribed for uncomplicated skin infections, urinary tract infections, and certain respiratory infections. The drug’s half‑life of about 1.5hours allows for a twice‑daily dosing schedule, which many patients find more convenient than three‑times‑daily options.
Key Criteria for Comparing Antibiotics
When you line up Duricef against other antibiotics, focus on these six attributes:
- Spectrum of activity: Which bacteria does the drug reliably kill?
- Dosing convenience: How many times a day and for how long?
- Side‑effect profile: Frequency and severity of common adverse events.
- Resistance risk: How likely is local resistance to render the drug ineffective?
- Pregnancy & breastfeeding safety: FDA category and clinical guidance.
- Cost & insurance coverage: Out‑of‑pocket price and formulary status.

Side‑by‑Side Comparison Table
| Antibiotic | Spectrum | Typical Adult Dose | Common Side Effects | Pregnancy Category |
|---|---|---|---|---|
| Duricef (Cefadroxil) | Gram‑positive + limited gram‑negative | 500mg PO q12h (7‑10days) | Diarrhea, nausea, rash | B |
| Cephalexin | Similar to Duricef; slightly broader gram‑negative | 500mg PO q6h (7‑14days) | Diarrhea, abdominal pain | B |
| Amoxicillin | Gram‑positive, some gram‑negative (H.influenzae) | 500mg PO q8h (7‑10days) | Diarrhea, rash, candidiasis | B |
| Azithromycin | Broad gram‑negative, atypicals, some gram‑positive | 500mg PO day1, then 250mg daily x4days | GI upset, QT prolongation (rare) | B |
| Doxycycline | Broad gram‑positive & gram‑negative, intracellular | 100mg PO q12h (7‑14days) | Photosensitivity, esophagitis | D |
| Clindamycin | Gram‑positive, anaerobes | 300mg PO q6h (7‑10days) | Clostridioides difficile infection risk | B |
| Cefixime | Broader gram‑negative (including E.coli) | 400mg PO q24h (5‑7days) | Diarrhea, abdominal pain | B |
Profiles of Popular Alternatives
Cephalexin - Another first‑generation cephalosporin, cephalexin shares most of Duricef’s spectrum but offers a slightly better gram‑negative punch. Its four‑times‑daily dosing can be a hassle, though a 500mg q6h schedule mimics many skin infection regimens. Side effects are largely GI‑related, and cross‑reactivity with penicillin is reported in roughly 5% of patients.
Amoxicillin - A beta‑lactam from the penicillin class, amoxicillin covers many upper‑respiratory pathogens and is the go‑to for otitis media. It’s less effective against Staphylococcus aureus than Duricef, so in skin infections caused by MRSA‑susceptible strains, it may fall short.
Azithromycin - A macrolide with a long half‑life, azithromycin shines in atypical respiratory infections (e.g., Mycoplasma). Its once‑daily dosing over five days is patient‑friendly, but it lacks robust activity against the gram‑positive cocci that Duricef handles well.
Doxycycline - A tetracycline that covers a very broad spectrum, including intracellular organisms (Chlamydia, Rickettsia). It’s a solid alternative when a clinician wants coverage beyond what cefadroxil provides, but it can cause photosensitivity and is contraindicated in pregnancy (CategoryD).
Clindamycin - Excellent for anaerobic infections and certain skin abscesses, especially when MRSA is suspected. However, its high association with C.difficile colitis makes clinicians cautious, reserving it for cases where other agents fail.
Cefixime - A third‑generation oral cephalosporin with enhanced gram‑negative activity, useful for uncomplicated urinary tract infections. Its once‑daily dosing is convenient, but it’s less potent against Staphylococcus aureus compared with Duricef.
When to Choose Duricef Over Alternatives
If your infection is caused by a susceptible gram‑positive organism (e.g., Streptococcus pyogenes) and you need a twice‑daily schedule, Duricef is a strong candidate. It’s also a good fallback for patients with mild penicillin allergy who haven’t reacted to cephalosporins before. In regions where local resistance rates for first‑generation cephalosporins stay below 10%, Duricef maintains high cure rates.
Conversely, avoid Duricef when you suspect an organism that needs broader gram‑negative coverage (like Pseudomonas) or when a once‑daily regimen is essential for adherence. In pregnant patients, the FDA’s CategoryB rating permits use, but if you can select a drug with a CategoryA designation (like ampicillin), that might be preferable.
Practical Tips & Pitfalls to Avoid
- Take Duricef with a full glass of water and stay upright for at least 30minutes to reduce esophageal irritation.
- Complete the full prescribed course even if symptoms improve; early stopping fuels resistance.
- Inform your doctor of any history of severe penicillin allergy; a cross‑reaction test may be advised.
- Watch for signs of an allergic reaction-hives, swelling, difficulty breathing-and seek emergency care immediately.
- If you develop persistent diarrhea, especially with blood or mucus, contact your clinician to rule out C.difficile infection.
Frequently Asked Questions
Can I take Duricef if I’m allergic to penicillin?
Mild penicillin allergies often do not cross‑react with cephalosporins like cefadroxil, but severe IgE‑mediated reactions can. Your doctor may perform a skin test or choose an alternative antibiotic if you’ve had anaphylaxis to penicillin.
How long does it take for Duricef to start working?
Patients usually notice symptom improvement within 48‑72hours, though the full course should be taken to ensure eradication of the bacteria.
Is Duricef safe during pregnancy?
Duricef is classified as Pregnancy CategoryB, meaning animal studies have not shown risk and there are no well‑controlled studies in pregnant women. It’s generally considered safe when the benefit outweighs potential risk.
What should I do if I miss a dose?
Take the missed dose as soon as you remember unless it's almost time for the next dose. Do not double up; a double dose can increase side‑effect risk.
How does Duricef compare cost‑wise to other antibiotics?
Generic cefadroxil typically costs $0.10‑$0.20 per 500mg tablet in the U.S., similar to generic cephalexin and cheaper than azithromycin or doxycycline, which range $0.30‑$0.60 per tablet.
Armed with this comparison, you can talk to your health‑care provider confidently, knowing when Duricef shines and when another antibiotic might be a smarter pick.
Nora Russell
October 15, 2025 AT 19:46While the guide admirably aggregates a wealth of data on Duricef, its analytical rigor is compromised by a reliance on superficial dosage tables rather than a nuanced exploration of cefadroxil's pharmacodynamic profile. The absence of discussion regarding tissue penetration coefficients and resistance mechanisms renders the comparison somewhat pedantic. Moreover, the guide neglects to address the economic implications of generic versus branded formulations, a glaring omission for cost‑conscious prescribers. In sum, the piece would benefit from a deeper, evidence‑based dissection rather than the present cursory overview.
Josephine Bonaparte
October 19, 2025 AT 00:00Great rundown! I love how you broke down the dosing schedules-makes it super easy to see why twice‑daily might be a win for busy folks. The only thing I’d tweak is the typo “gram‑positive” that slipped in a couple of places, but overall solid work. Keep it up, and maybe throw in a quick tip about taking the pill with water to avoid esophageal irritation.
Meghan Cardwell
October 22, 2025 AT 04:14The pharmacological discourse surrounding first‑generation cephalosporins such as cefadroxil necessitates an interdisciplinary lens that juxtaposes microbiological spectra with clinical pharmacokinetics. In this context, Duricef emerges not merely as a synthetized analogue but as a molecular scaffold optimized for β‑lactamase resistance. Empirical data from Phase III trials indicate a minimum inhibitory concentration (MIC) distribution that predominates within the susceptible breakpoint for Streptococcus pyogenes. Conversely, its activity against Enterobacteriaceae, while present, hovers near the epidemiological cut‑off, thereby limiting its monotherapy utility in polymicrobial urinary tract infections. The dosing regimen of 500 mg administered bid aligns with the drug’s elimination half‑life, fostering steady‑state concentrations that eclipse the mutant prevention concentration for most gram‑positive isolates. However, the pharmacodynamic target of 40% fT>MIC, quintessential for β‑lactams, may be suboptimal in patients with augmented renal clearance, necessitating dose escalation or interval contraction. From a stewardship perspective, the incorporation of Duricef into empirical algorithms should be contingent upon local susceptibility matrices that reflect a resistance prevalence below 10%. Moreover, the drug’s safety profile, typified by gastrointestinal disturbances and rash, is generally favorable, yet clinicians must remain vigilant for idiosyncratic hypersensitivity reactions that can precipitate anaphylaxis. The cross‑reactivity with penicillins, although statistically modest at approximately 5%, mandates a thorough allergy history to preempt inadvertent exposure. In obstetric populations, the Category B designation offers a therapeutic window, but alternative agents with Category A status may be preferable when teratogenic risk mitigation is paramount. Economic analyses reveal that generic cefadroxil’s cost per tablet resides in a lower quartile relative to azithromycin and doxycycline, enhancing its formulary appeal. Nonetheless, insurance formularies sometimes impose prior‑authorization constraints that can erode its cost‑effectiveness advantage. The comparative table presented, while exhaustive, could be augmented by integrating pharmacoeconomic indices such as cost‑per‑cure and number‑needed‑to‑treat metrics. Finally, patient adherence is intrinsically linked to dosing convenience; the bid schedule of Duricef strikes a pragmatic balance between the thrice‑daily mandates of cephalexin and the once‑daily allure of azithromycin. In conclusion, Duricef constitutes a viable first‑line option for uncomplicated gram‑positive infections, provided that prescribers calibrate its use to individual pharmacokinetic parameters, resistance epidemiology, and patient‑specific factors.
stephen henson
October 25, 2025 AT 08:28Nice summary! 👍 The twice‑daily dosing really does make a difference for people with busy schedules. Just remember to stay upright after taking the pill to avoid any throat irritation. If you’re ever unsure, chat with your pharmacist-they’re a great resource. 😊
Manno Colburn
October 28, 2025 AT 11:42Yo, i totally get where u’re comin from, but let’s take a step back and ponder the existential weight of a pill nestled in our daily routine. The very act of popping a capsule is not a mere biochemical transaction; it’s a ritual that binds us to the grand tapestry of antimicrobial warfare. When you talk about "staying upright," i can’t help but marvel at how gravity itself becomes a reluctant ally in the saga of drug absorption. Yet, the universe is indifferent-if you miss a dose, the bacteria might just waltz back, unscathed. So, while you champion the pharmacist’s role, remember that every moment of non‑adherence is a micro‑rebellion against the very notion of therapeutic certainty. In sum, the cascade of events from ingestion to systemic distribution is a choreography worthy of a thousand‑page dissertation, and we’re all just dancing to its rhythm.
Namrata Thakur
October 31, 2025 AT 15:57Excellent overview! The clear bullet points make it easy to compare each antibiotic at a glance. I especially appreciate the tip about taking Duricef with plenty of water-it’s a simple habit that can prevent throat irritation. Thanks for putting together such a helpful guide.
Chloe Ingham
November 3, 2025 AT 20:11Listen, the pharmaceutical industry doesn’t want us to know that these “comparisons” are often salted with hidden agendas. They push drugs like azithromycin because they’re lit up by big‑money marketing campaigns, not because they’re always the best clinical choice. The subtle wording in the guide hints at this bias, especially when it glosses over the potential for resistance with over‑prescribing. Stay vigilant and don’t let the narrative be dictated by profit‑driven entities.
Mildred Farfán
November 7, 2025 AT 00:25Oh, absolutely-because nothing says “trustworthy medical advice” like a side‑eye glance at the marketing department, right? 😏 In all seriousness, though, the guide does a decent job of laying out the facts, even if the industry’s shadow looms in the background. Let’s just hope the next edition includes a “fear‑of‑big‑pharma” disclaimer for extra flair.
Brian Lancaster-Mayzure
November 10, 2025 AT 04:39Good job breaking down the options. For anyone still uncertain, consider the infection site and the most likely pathogens; that often guides the choice more than convenience alone. Also, keep an eye on local resistance patterns-they can tip the scales in favor of one drug over another.
Rhys Black
November 13, 2025 AT 08:53It is profoundly disconcerting to witness the casual dismissal of antimicrobial stewardship in so many popular health articles. By failing to underscore the gravity of resistance development, such pieces inadvertently poison the public discourse. Ethical medical communication demands a forthright exposition of both benefits and perils, lest we betray the very patients we claim to serve.
Tom Lane
November 16, 2025 AT 13:07Interesting take on the dosing schedules! I’m curious about how the half‑life of cefadroxil influences the need for a twice‑daily regimen compared to the once‑daily azithromycin. Also, does renal function significantly affect the dosing adjustments for Duricef?
Mike Rylance
November 19, 2025 AT 17:21Thank you for the comprehensive comparison. I would add that particular attention should be given to patients with hepatic impairment, as metabolism may alter the drug’s efficacy. Including a brief note on dose modification in such populations would further enhance the utility of this guide.
Srinivasa Kadiyala
November 22, 2025 AT 21:35-Hold on-; while the guide is thorough, it seems to overlook the fact that-yes-some clinicians prefer off‑label use of cefadroxil for deeper soft‑tissue infections; this is a point that could have been highlighted; moreover, the cost analysis, albeit useful, fails to consider bulk purchasing discounts which can dramatically alter the price landscape.
Alex LaMere
November 26, 2025 AT 01:49Spot on summary. 👍👍
KayLee Voir
November 29, 2025 AT 06:04Duricef’s twice‑daily dosing is a convenient middle ground.
inas raman
December 2, 2025 AT 10:18Totally agree with the point about staying hydrated while taking Duricef. I’ve found that drinking a big glass of water not only helps the pill go down smoothly but also reduces the chance of stomach upset. It’s a simple habit that makes a big difference, especially if you’re on a course of antibiotics for a week or more.
Anne Snyder
December 5, 2025 AT 14:32The guide’s inclusion of pregnancy categories is particularly valuable for clinicians counseling expectant mothers. Knowing that Duricef falls under Category B provides reassurance, yet it also underscores the need to weigh the benefits against any potential risks, especially when alternative agents with Category A status are available.
Rebecca M
December 8, 2025 AT 18:46-In conclusion-, the comparative analysis presented serves as a solid foundation for antibiotic selection; however, clinicians must continually integrate evolving resistance data, patient-specific factors, and pharmacoeconomic considerations to make truly informed decisions.